Copyright
©The Author(s) 2015.
World J Hepatol. Mar 27, 2015; 7(3): 327-343
Published online Mar 27, 2015. doi: 10.4254/wjh.v7.i3.327
Published online Mar 27, 2015. doi: 10.4254/wjh.v7.i3.327
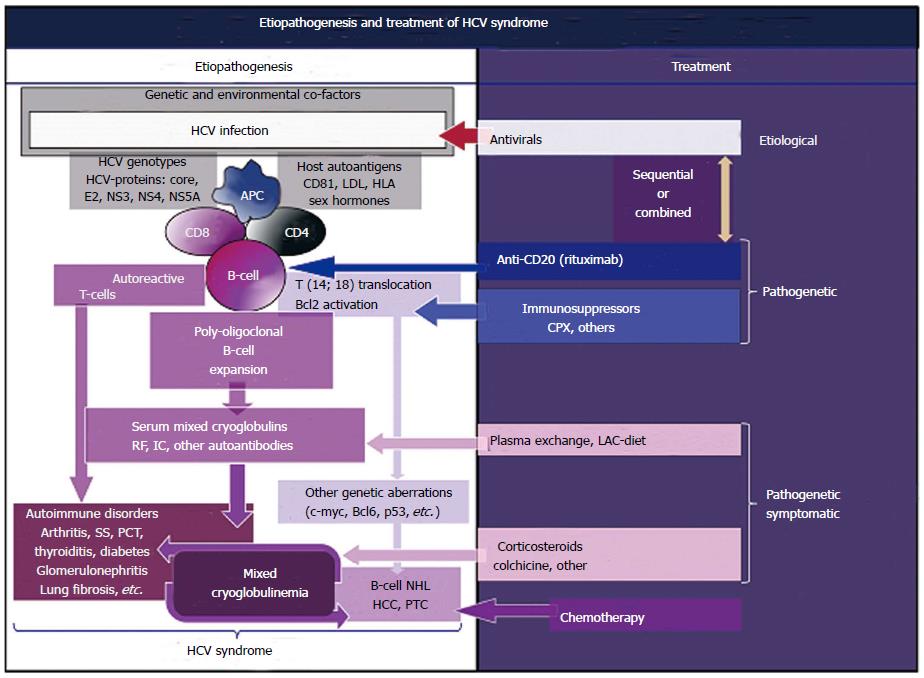
Figure 1 Etiopathogenetic cascade of hepatitis C virus syndrome, including both hepatic and extra-hepatic disorders, is a multifactorial and multistep process: The remote events include hepatitis C virus infection, predisposing genetic factors and, possibly, unknown environmental/toxic triggers (Left).
The HCV-driven immune-system alterations with prominent “benign” lymphoproliferation, from one side, and oncogenic alterations, from another side, may be the result of different pathogenetic mechanisms not mutually exclusive, through a multifactorial and multistep process: Viral antigens (core, envelope E2, NS3, NS4, NS5A proteins) may exert a chronic stimulus on the host immune system, the high-affinity binding between HCV-E2 and CD81 and consequent t(14;18) translocation with bcl-2 proto-oncogene activation, a cross-reaction between particular HCV antigens and host autoantigens, i.e., a molecular mimicry mechanism, and a direct infection of B-lymphocytes by HCV responsible for neoplastic cell transformation. Predisposing host factors may include particular HLA alleles, and both metabolic and hormonal conditions. The main consequence is a “benign” B-cell proliferation with production of various autoantibodies, among which RF and cryo- and non-cryoprecipitable IC. These serological alterations may be correlated with different organ- and non-organ-specific autoimmune disorders, including the systemic manifestations of MCs, or cryoglobulinemic vasculitis. Moreover, the activation of Bcl2 proto-oncogene, responsible for prolonged B cell survival, may be a predisposing condition to other genetic aberrations (c-myc, Bcl6, and p53 activation), which may lead to frank B cell lymphomas (B-NHL) and other malignancies (HCC: Hepatocellular carcinoma; PTC: Papillary thyroid cancer). The appearance of malignant neoplasias can be seen in a small but significant percentage of patients, usually as a late complication. Both immunological and neoplastic disorders show a clinico-serological and pathological overlap. Often, autoimmune organ-specific manifestations may evolve to systemic conditions, such as mixed cryoglobulinemia syndrome, and less frequently to overt malignancies. Conversely, it is not uncommon that patients with malignancies develop one or more autoimmune manifestations. In this scenario, MCs is at the crossing road between autoimmune and neoplastic disorders; Right: There are not comprehensive therapeutical guidelines for the HCV syndrome because of the complexity of its pathogenetic and clinico-prognostic characteristics; we can adopt in part the therapeutical strategy used for MCs, which often encompasses the different clinical variants of HCV syndrome. This therapeutical approach is essentially based on three main levels of intervention: the etiological treatment by means of antiviral drugs directed at HCV eradication, the pathogenetic therapies with immunomodulating/antineoplastic drugs, and the pathogenetic/symptomatic therapies such as corticosteroids and plasma exchange (see also text). HCV: Hepatitis C virus; IC: Immune complexes; SS: Sicca syndrome; PCT: Porphyria cutanea tarda; RF: Rheumatoid factor; MCs: Mixed cryoglobulinemia syndrome; CPX: Cyclophosphamide.
- Citation: Ferri C, Sebastiani M, Giuggioli D, Colaci M, Fallahi P, Piluso A, Antonelli A, Zignego AL. Hepatitis C virus syndrome: A constellation of organ- and non-organ specific autoimmune disorders, B-cell non-Hodgkin’s lymphoma, and cancer. World J Hepatol 2015; 7(3): 327-343
- URL: https://www.wjgnet.com/1948-5182/full/v7/i3/327.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i3.327