Copyright
©The Author(s) 2021.
World J Hepatol. Sep 27, 2021; 13(9): 1079-1097
Published online Sep 27, 2021. doi: 10.4254/wjh.v13.i9.1079
Published online Sep 27, 2021. doi: 10.4254/wjh.v13.i9.1079
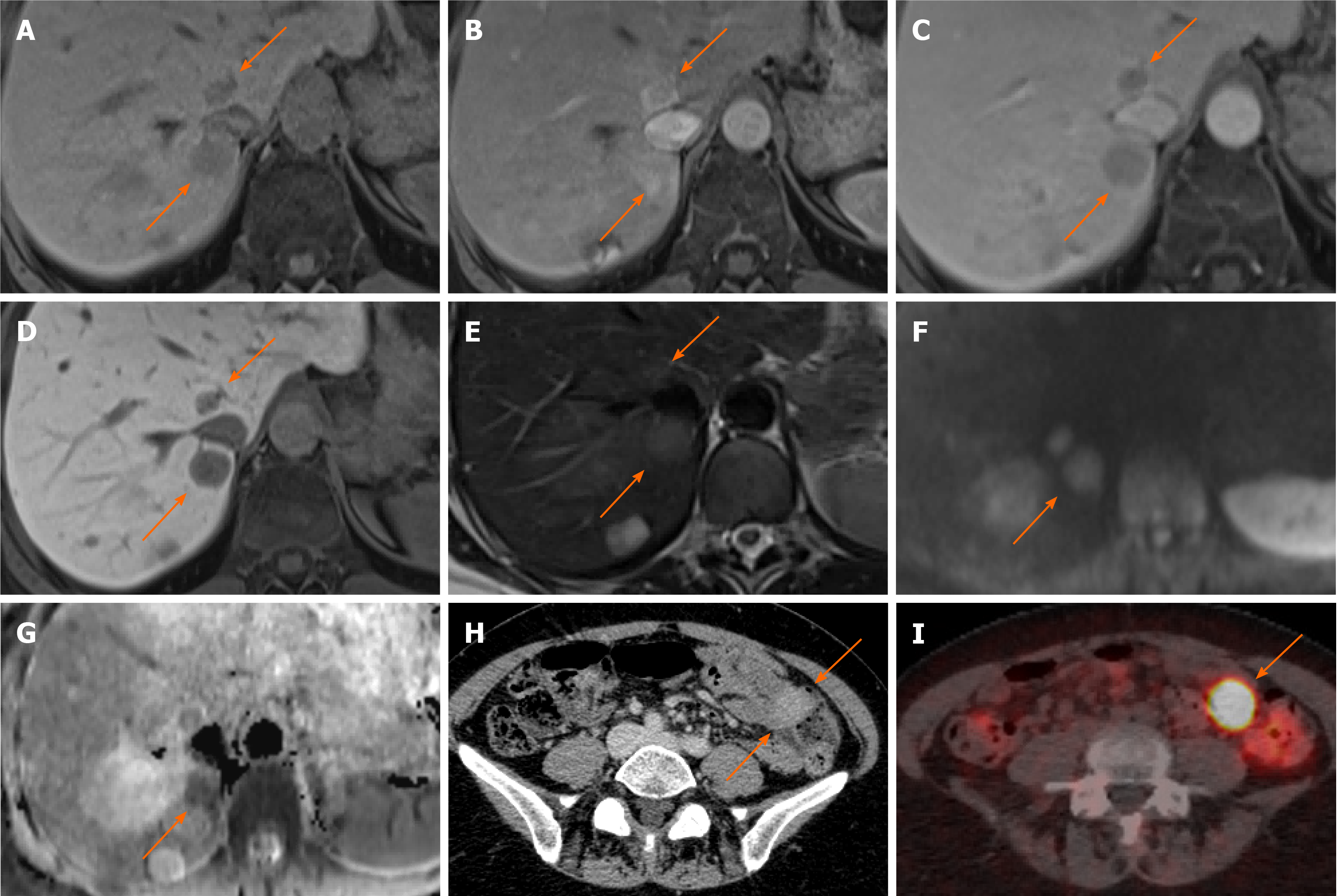
Figure 11 Neuroendocrine carcinoma metastases.
A 55-year-old female with anaemia underwent computed tomography (CT) which identified multiple liver lesions. Magnetic resonance liver was performed and confirmed multiple haemangiomas and few other lesions, two of which are shown here, showing atypical appearances. A: Pre contrast phase sequence shows two lesions of low signal on either side of the inferior vena cava; B and C: On arterial phase (B) there is enhancement followed by prompt washout on portal venous (C) phase; D: There is no contrast retention on hepatobiliary phase; E: Lesions are nearly isointense to liver on T2-weighted sequence; F and G: Diffusion weighted imaging (F) at b800 shows hyperintense signal followed by low signal on apparent diffusion coefficient (G) in keeping with diffusion restriction. The nature of these was not clear, but they were suspicious for hypervascular metastases. The patient underwent a number of investigations including oesophago-gastro-duodenoscopy, colonoscopy, CT chest, abdomen and pelvis and an ultrasound scan of pelvis. None of these investigations have identified a primary source of the liver lesions. Targeted liver biopsy was performed and histology revealed well differentiated neuroendocrine carcinoma (Ki-67 = 4%); H: In retrospect, there was an enhancing lesion within the small bowel also present on previous CT; I: Subsequent Ga68-Dotatoc positron emission tomography-CT was performed which confirmed uptake within the small bowel consistent with primary tumour.
- Citation: Noreikaite J, Albasha D, Chidambaram V, Arora A, Katti A. Indeterminate liver lesions on gadoxetic acid-enhanced magnetic resonance imaging of the liver: Case-based radiologic-pathologic review. World J Hepatol 2021; 13(9): 1079-1097
- URL: https://www.wjgnet.com/1948-5182/full/v13/i9/1079.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i9.1079