Copyright
©The Author(s) 2023.
World J Hepatol. Apr 27, 2023; 15(4): 497-514
Published online Apr 27, 2023. doi: 10.4254/wjh.v15.i4.497
Published online Apr 27, 2023. doi: 10.4254/wjh.v15.i4.497
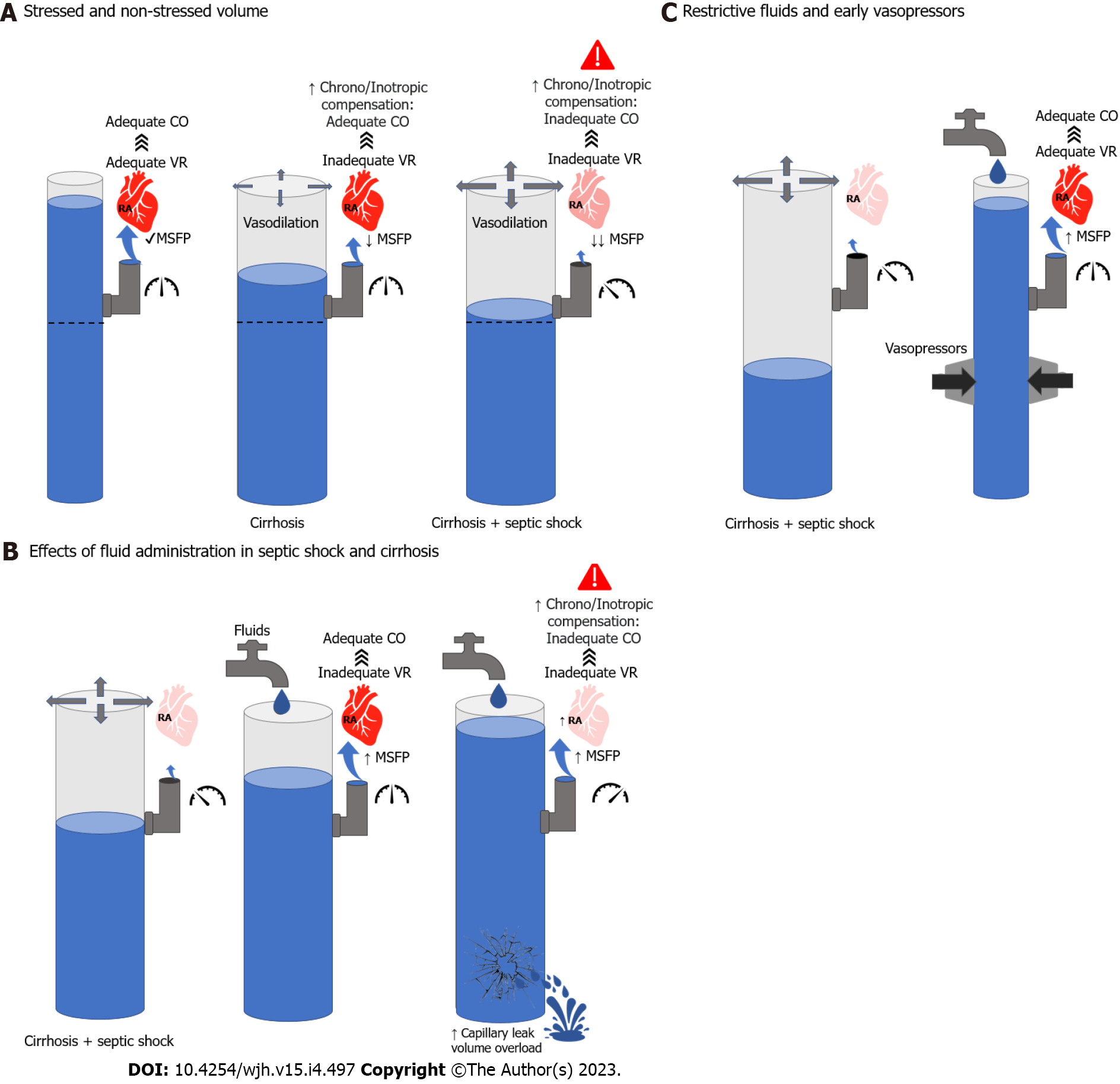
Figure 1 Hemodynamic considerations in the management of cirrhosis and septic shock.
A: Left; Normal mean systemic filling pressures (MSFP) leading to adequate venous return and cardiac output (CO). Middle; vasodilation in cirrhosis leading to lower MSFP and inadequate venous return (VR). However, compensatory mechanisms are able to maintain adequate CO. Right; further vasodilation leading to lower MSFP and inadequate VR. In this case, neurohumoral and cardiac compensation are not enough to maintain CO; B: Left; cirrhosis and septic shock pathophysiology. Middle; Effects of adequate volume resuscitation leading to increased MSFP. In the context of normal filling pressures, this will increase VR and CO. Right; Excessive fluid resuscitation will lead to high filling pressures which will decrease VR and CO. In addition, it may lead to volume overload and capillary leak; C: Left; cirrhosis and septic shock pathophysiology. Right; adjuvant effect of fluids and vasopressors on MSFP, VR and CO without leading to volume overload. CO: Cardiac output; MSFP: Mean systemic filling pressures; RA: Right atrium; VR: Venous return.
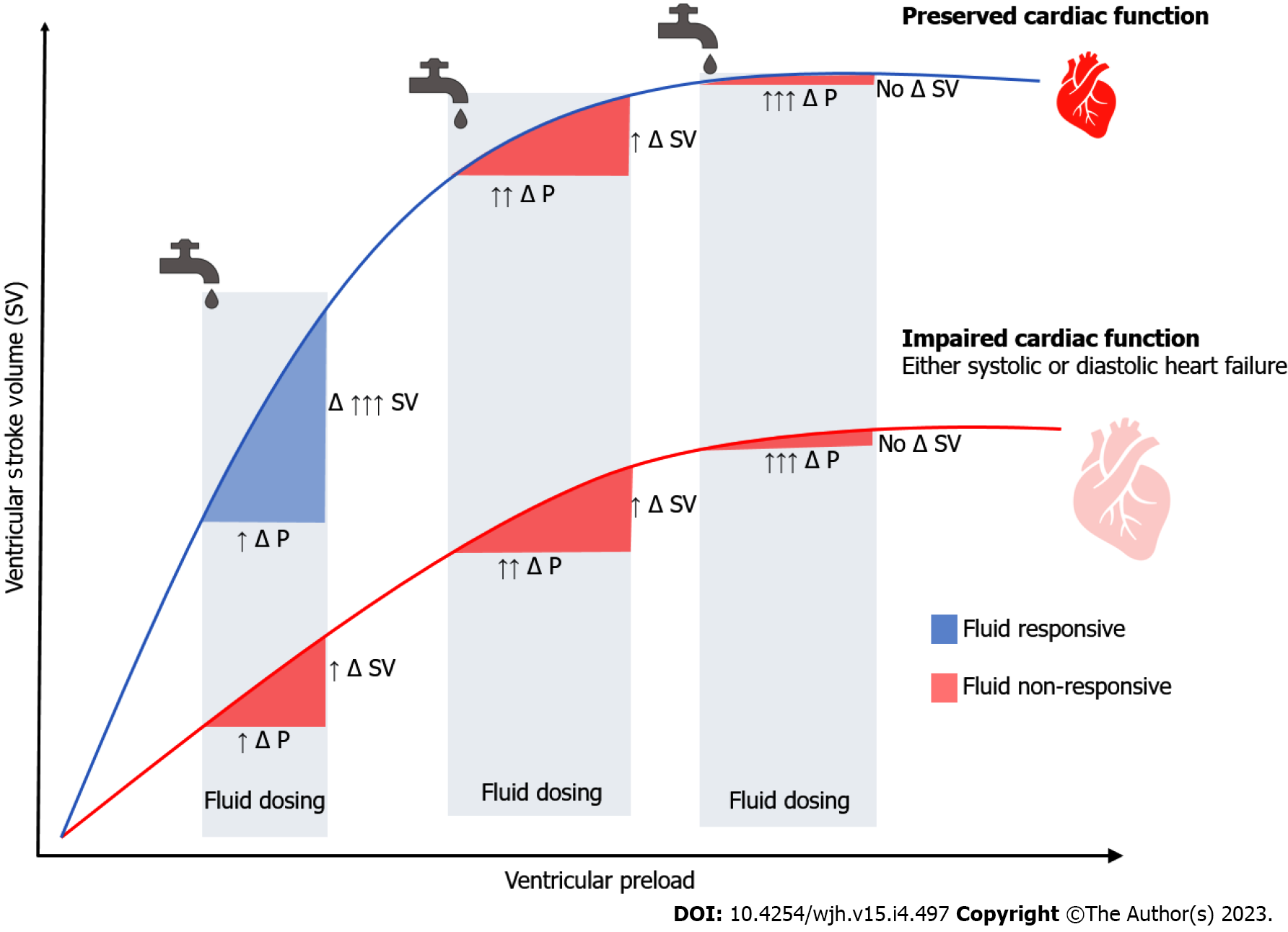
Figure 2 Frank-Starling curves in septic shock.
Every fluid bolus will lead in a change in pressure (Δ P) and a change in stroke volume (Δ SV). The effect of fluids on cardiac output among patients with normal (upper curve) and impaired (lower curve) myocardial function is depicted. Even among patients with normal myocardial reserve, excess fluid administration may significantly increase pressure without significantly increasing stroke volume, which may ultimately lead to anasarca. Δ P: Change in pressure; Δ SV: Change in stroke volume.
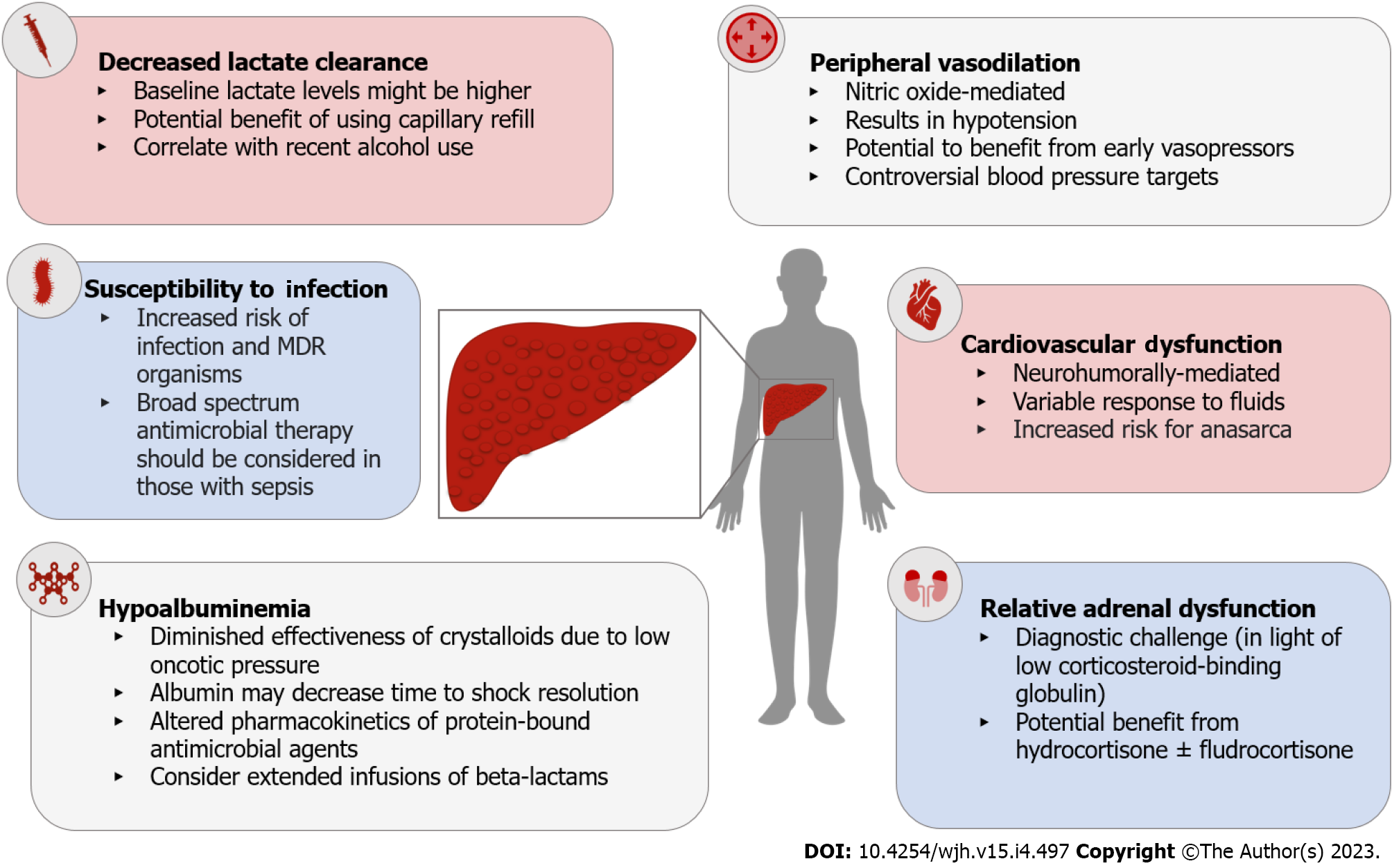
Figure 3 Pathophysiologic changes in cirrhosis that impact the management of septic shock.
MDR: Multi-drug resistant.
- Citation: Jimenez JV, Garcia-Tsao G, Saffo S. Emerging concepts in the care of patients with cirrhosis and septic shock. World J Hepatol 2023; 15(4): 497-514
- URL: https://www.wjgnet.com/1948-5182/full/v15/i4/497.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i4.497