Copyright
©The Author(s) 2021.
World J Stem Cells. Jul 26, 2021; 13(7): 825-840
Published online Jul 26, 2021. doi: 10.4252/wjsc.v13.i7.825
Published online Jul 26, 2021. doi: 10.4252/wjsc.v13.i7.825
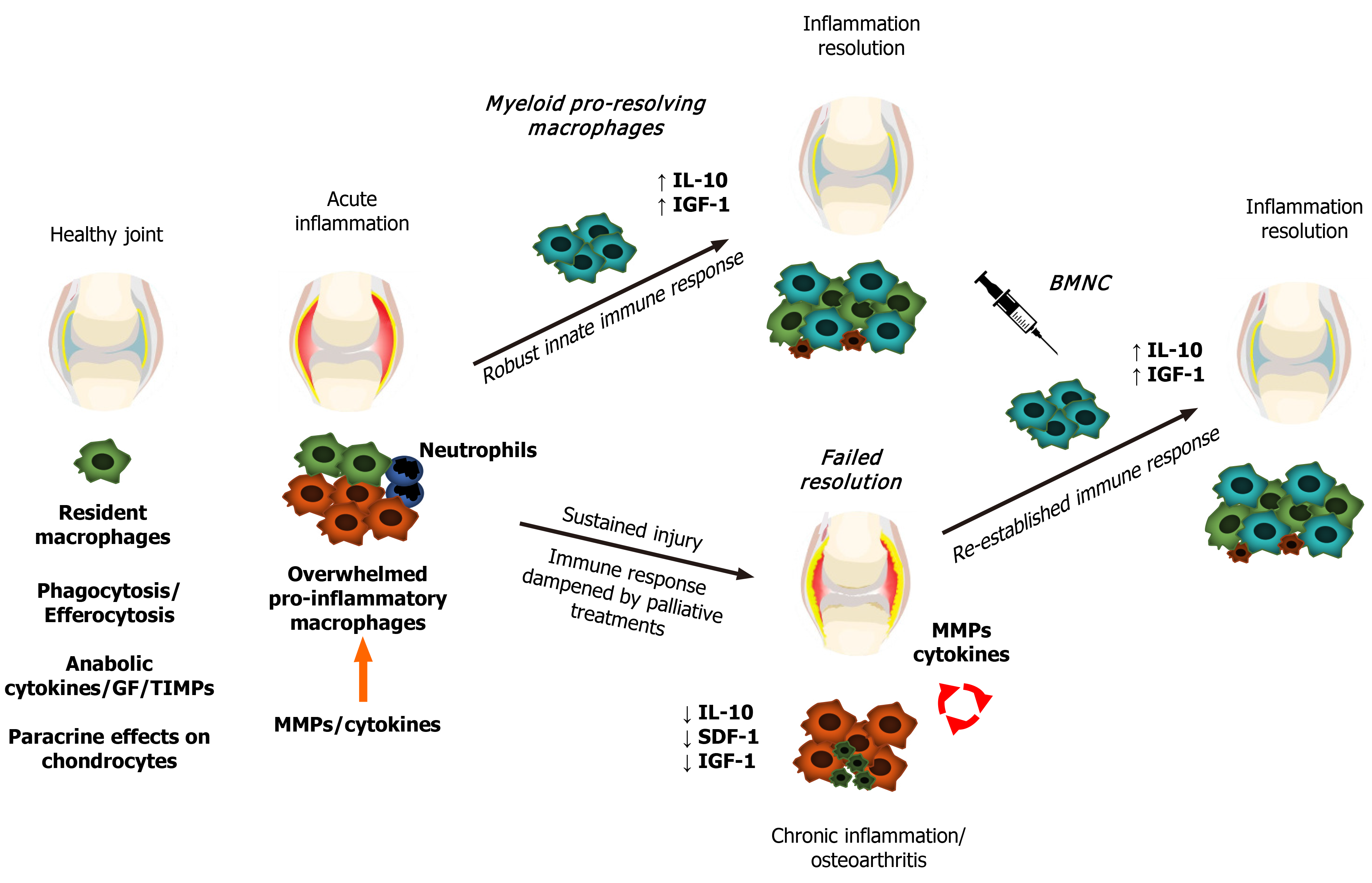
Figure 1 Schematic representation of macrophage status and responses during joint health and disease.
Macrophages promote synovial health through phagocytosis, efferocytosis, secretion of synovial fluid cytokines and growth factors, and paracrine effects on chondrocyte metabolism. Following damage, synovial macrophages form a shield to the injured site to further drive tissue repair. If the extent of the injury or continuing trauma overwhelms the shielding and repairing capacity of macrophages, macrophages increase expression of cytokines, including interleukin (IL)-1, IL-6, and tumor necrosis factor -α in a phlogistic inflammatory response, recruiting first neutrophils, followed by myeloid macrophages. These macrophages have a strong pro-resolving capacity associated with high production of IL-10 and insulin-like growth factor 1, which then leads to inflammation resolution and tissue repair. If interfering factors impair the resolution of the inflammatory process, chronic low-grade inflammation persists, leading to aberrant remodeling of synovial tissues and joint degeneration. Joint injection with bone marrow mononuclear cells in chronically inflamed joints augments the macrophage-mediated mechanisms of joint homeostasis, resolving joint inflammation. GF: Growth factors; TIMPs: Tissue inhibitors of metalloproteinases; MMPs: Matrix metalloproteinases; IL-10: Interleukin 10; IGF-1: Insulin-like growth factor 1; SDF-1: Stromal-derived factor 1; BMNC: Bone marrow mononuclear cells.
- Citation: Menarim BC, MacLeod JN, Dahlgren LA. Bone marrow mononuclear cells for joint therapy: The role of macrophages in inflammation resolution and tissue repair. World J Stem Cells 2021; 13(7): 825-840
- URL: https://www.wjgnet.com/1948-0210/full/v13/i7/825.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i7.825