Published online Jan 26, 2020. doi: 10.4252/wjsc.v12.i1.87
Peer-review started: June 18, 2019
First decision: July 31, 2019
Revised: August 12, 2019
Accepted: October 14, 2019
Article in press: October 14, 2019
Published online: January 26, 2020
Breast cancer is a common malignant tumor that seriously threatens women’s health. Breast cancer stem cell (CSC)-like cell population may be the main factor for breast cancer metastasis. Therefore, targeted therapy for CSCs has great potential significance. Hypoxia-inducible factor is a transcription factor widely expressed in tumors. Studies have shown that down-regulation of the hypoxia signaling pathway inhibits tumor stem cell self-renewal and increases the sensitivity of stem cells to radiotherapy and chemotherapy mediated by hypoxia-inducible factor-2α (HIF-2α). However, the specific mechanism remains unclear and further research is necessary.
To investigate the effect of HIF-2α down-regulation on stem cell markers, microsphere formation, and apoptosis in breast cancer cell line MDA-MB-231 under hypoxia and its possible mechanism.
Immunohistochemistry was used to detect the expression of HIF-2α and CD44 in triple-negative breast cancer (TNBC) and non-TNBC tissues. Double-labeling immunofluorescence was applied to detect the co-expression of HIF-2α and CD44 in MDA-MB-231 cells and MCF-7 cells. HIF-2α was silenced by RNA interference, and the expression of CD44 and transfection efficiency were detected by real-time fluorescent quantitative PCR. Further, flow cytometry, TdT-mediated X-dUTP nick end labeling, and mammosphere formation assays were used to evaluate the effect of HIF-2α on CSCs and apoptosis. The possible mechanisms were analyzed by Western blot.
The results of immunohistochemistry showed that HIF-2α was highly expressed in both TNBC and non-TNBC, while the expression of CD44 in different molecular types of breast cancer cells was different. In in vitro experiments, it was found that HIF-2α and CD44 were expressed almost in the same cell. Compared with hypoxia + negative-sequence control, HIF-2α small interfering ribonucleic acid transfection can lower the expression of HIF-2α and CD44 mRNA(P < 0.05), increase the percentage of apoptotic cells (P < 0.05), and resulted in a reduction of CD44+/CD24− population (P < 0.05) and mammosphere formation (P < 0.05) in hypoxic MDA-MB-231 cells. Western blot analysis revealed that phosphorylated protein-serine-threonine kinase (p-AKT) and phosphorylated mammalian target of rapamycin (p-mTOR) levels in MDA-MB-231 decreased significantly after HIF-2α silencing (P < 0.05).
Down-regulation of HIF-2α expression can inhibit the stemness of human breast cancer MDA-MB-231 cells and promote apoptosis, and its mechanism may be related to the CD44/phosphoinosmde-3-kinase/AKT/mTOR signaling pathway.
Core tip: Cancer stem cells (CSCs) play an important role in tumor formation, growth, invasion, metastasis, and recurrence. Hypoxia can promote the differentiation of various tumor cells, enable cells to acquire stem cell characteristics, and enhance tumor cell invasion and tumorigenicity. In the long-term exposure of tumors to hypoxia, the major regulatory factor is hypoxia-inducible factor-2α (HIF-2α), which can promote the malignant biological behavior of tumors by activating its downstream target genes. Studies have shown that the effect of HIF-2α on tumor cells may be related to CD44, a marker for breast CSCs. In this study, breast cancer cell line MCF-7 and basal breast cancer cell line MDA-MB-231 were utilized to investigate the relationship between HIF-2α and CD44 gene expression and the regulatory effect of HIF-2α on CD44.
- Citation: Bai J, Chen WB, Zhang XY, Kang XN, Jin LJ, Zhang H, Wang ZY. HIF-2α regulates CD44 to promote cancer stem cell activation in triple-negative breast cancer via PI3K/AKT/mTOR signaling. World J Stem Cells 2020; 12(1): 87-99
- URL: https://www.wjgnet.com/1948-0210/full/v12/i1/87.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v12.i1.87
Breast cancer is one of the most common malignant tumors. Its incidence rate is the highest in females and has a rising trend[1-3]. Although advanced medical technology has significantly improved the 5-year survival rate of many types of breast cancer, there are still 20% to 30% of patients who will have recurrence, serious complications, and even death after treatment[4-6]. According to the report by Dent et al[7], the 5-year survival rate of patients with recurrent breast cancer is only about 60%. Distant metastasis is one of the most important reasons. In particular, attention needs to be paid to patients with triple-negative breast cancer (TNBC), which is highly invasive and more prone to recurrence and metastasis than other forms of breast cancer[8-10]. Therefore, studies on TNBC are popular in clinical research. In recent years, researchers have found a small number of highly tumorigenic cell populations in breast tumors that express stem cell-like properties and are capable of self-renewal and differentiation, which are considered to be the source of tumor recurrence[11-13]. Some latest studies have suggested that deaths caused by TNBC are mainly associated with persistent cancer stem cells (CSCs)[14-16]. An in vitro experiment with CSCs from Lu et al[17] also showed that chemotherapy can enrich CSCs in TNBC and induce recurrence. Hence, targeted therapy for inhibiting CSC population has great clinical value. In the study of Samanta et al[18], hypoxia can promote the ability of tumor cells to obtain the features of stem cells and enhance the resistance of breast cancer cells to chemotherapy. Carroll et al[19] revealed the role of gene expression of hypoxia-inducible factor-1α (HIF-1α) and hypoxia-inducible factor-2α (HIF-2α) in breast cancer cell proliferation. It is worth noting that HIF-2α is more important in regulating the state of CSCs. Studies have confirmed that HIF-2α can affect the biological characteristics of breast CSCs, which is related to CD44 and its downstream pathway[20,21]. As a widely distributed transmembrane glycoprotein, CD44 regulates the phosphoinosmde-3-kinase (PI3K)/protein-serine-threonine kinase (AKT)/mammalian target of rapamycin (mTOR) signaling pathway and participates in the migration of cancer cells. It is also highly expressed in CSCs and is one of the important markers of CSCs. Current studies have shown that the change of CD44 expression is consistent with the trend of HIF-2α expression[22-24], but the relationship between CD44 and HIF-2α and its regulation mechanism are still unknown. The aim of this study was to investigate the relationship between HIF-2α, CD44, and PI3K/AKT/mTOR signaling by using breast cancer cell line MDA-MB-231, and further analyze the mechanism of CSC activation in TNBC and its role in the malignant progression of TNBC.
A total of 49 female patients with primary breast cancer diagnosed at Cangzhou Central Hospital were enrolled in our study from 2016 to 2017. Among them are 29 cases of TNBC and 20 cases of lumen type breast cancer (non-TNBC). All the patients had never been treated with radiotherapy or chemotherapy and the diagnosis was confirmed pathologically by more than two pathologists. Patients who had recurrent or metastatic breast cancer were excluded. Tumor tissues from TNBC and non-TNBC patients obtained during surgery were fixed in 10% neutral buffered formalin and then embedded in paraffin wax for immunohistochemistry analysis. This study was approved by the Ethics Committee of Cangzhou Central Hospital.
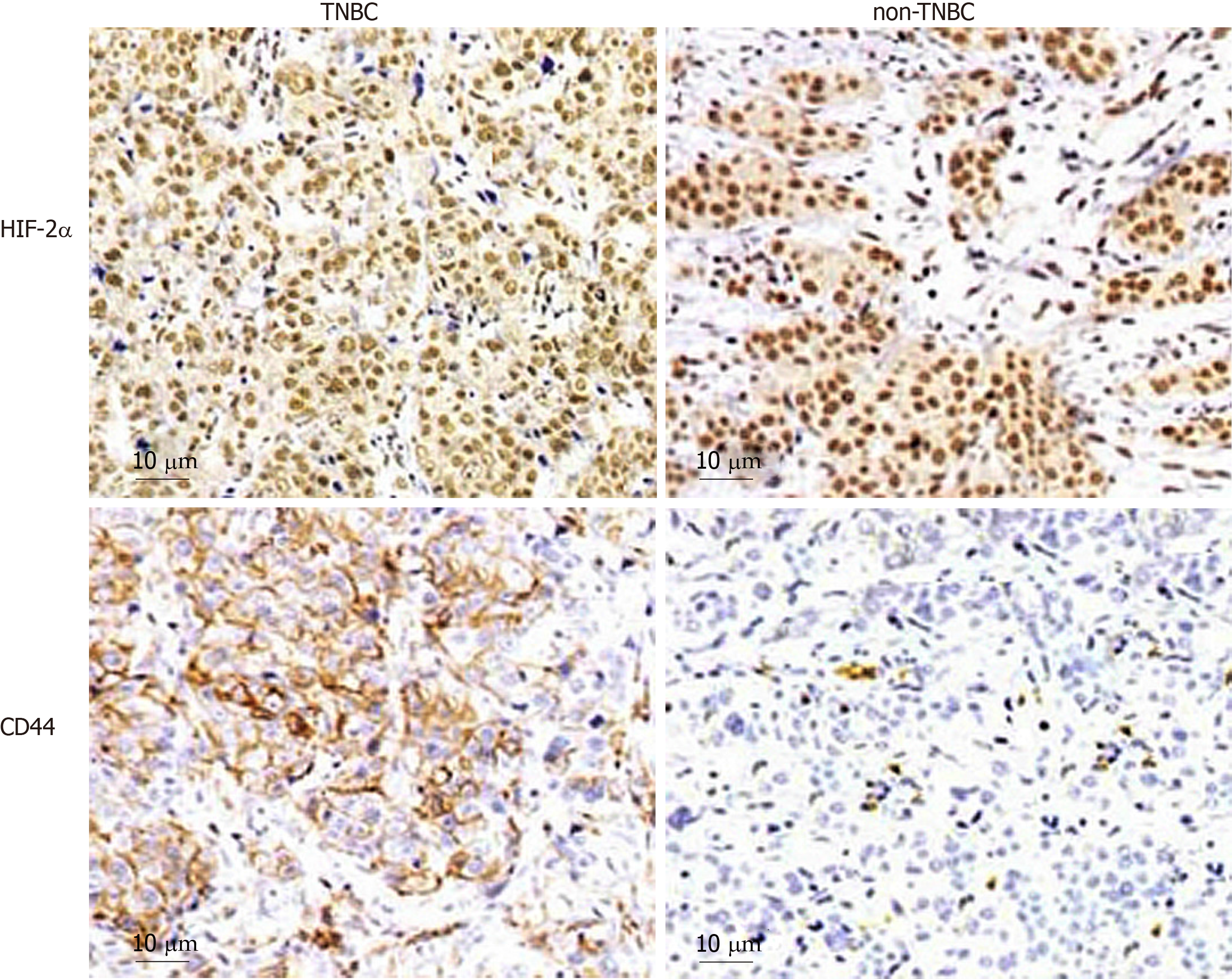
The expression of HIF-2α and CD44 in breast cancer was measured by immuno-histochemistry analysis. Briefly, sections of 4 μm thickness, obtained from patients with TNBC and non-TNBC, were subjected to deparaffinization, rehydration, and microwave antigen retrieval. The tissue sections were incubated in 0.3% H2O2 for 10 min and blocked using 1% BSA/PBS. The slides were then incubated with the following primary antibodies: anti-CD44 (dilution, 1:800) and anti-HIF-2α antibodies (dilution, 1:400; Abcam, Cambridge, MA, United States) overnight at 4 °C. Afterwards, the tissues were incubated with horseradish peroxidase-labeled secondary antibody (dilution, 1:1000; Santa Cruz Biotechnology, Inc) at 37 °C for 30 min and and stained with DAB, followed by haematoxylin counterstaning. The result was evaluated by pathologists based on the following criteria: >10% of cells stained represented positive expression and >30% of cells stained were considered as high expression.
Human breast cancer cell lines MDA-MB-231 and MCF-7 were obtained from American Type Culture Collection (ATCC, Manassas, VA, United States) and routinely cultured in Dulbecco’s modified Eagle’s medium-F12 medium containing 10% fetal bovine serum, 100 U/mL penicillin, and 100 μg/mL streptomycin (Gibco, Grand island, NY, United States). Cells were grown at 37 °C in a humidified incubator containing 5% CO2 and the complete medium changed 24 h. Digestion and passage were performed and cells in exponential growth stage were harvested for various experiments. For hypoxia treatment, all cells were cultured in a constant-temperature incubator with 1%O2, 5%CO2, and 94%N2.
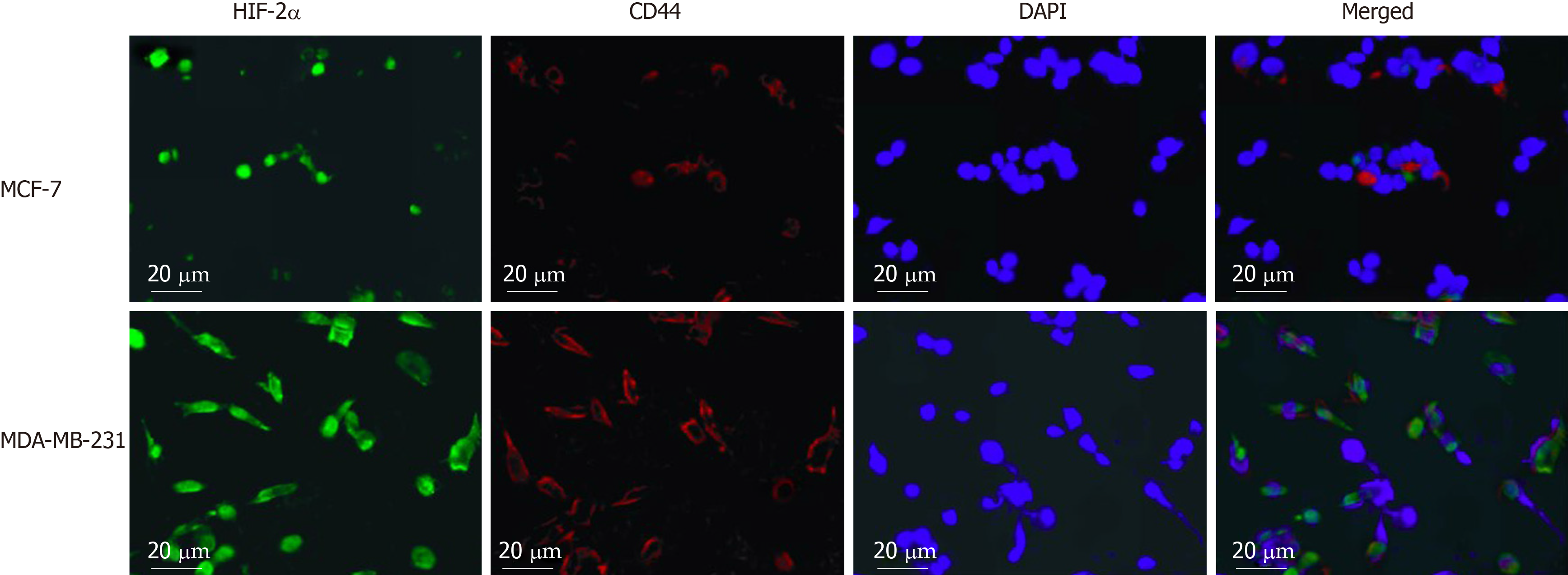
Cells were seeded on coverslides for 24 h and then fixed in 4% paraformaldehyde, followed by permeabilization with 0.2% Triton X-100. The nonspecific sites of samples were blocked with normal sheep serum at room temperature, and then the cells were stained with the primary antibody CD44-PE (dilution, 1:200) and rabbit anti-HIF-2α antibody (dilution, 1:600) provided by BD Biosciences overnight at 4 °C. Then, the samples were washed three times with PBS and incubated with the fluorophore-labelled goat anti-rabbit antibody for an additional 30 min at room temperature. After three washes with PBS, the samples were counterstained with 1 μg/mL 4',6-diamidino-2-phenylindole (Sigma, St. Louis, MO, United States) to visualize cell nuclei and the stained cells were analyzed under a fluorescence microscope.
5 × 105 cells were seeded in 6-well plates containing antibiotic-free medium after enzyme digestion and cultured in a CO2 incubator for 24 h. Transfection was performed in cells at 70%-80% confluence with small interfering ribonucleic acid (siRNA) using Lipofectamine 2000 (Invitrogen, United States) according to the manufacturer’s instructions. siRNAs targeting HIF-2α were designed and synthesized by Sangon Biotech (Shanghai) Co., Ltd. Three siRNAs were tested and that with the highest efficiency of HIF-2α down-regulation was chosen. Briefly, siRNA and Lipofectamine 2000 were diluted with Opti-MEM medium (Invitrogen, United States) prior to the mixing and then cultured at room temperature for 20 min to allow the formation of a mixture of siRNA-Lipofectamine 2000. The mixture was added to each well, and culturing continued for 24 h. The medium was replaced with complete medium and incubated for an additional 24 h after hypoxia treatment. RNA was harvested to detect the expression of HIF-2α after 48 h by reverse transcription-PCR.
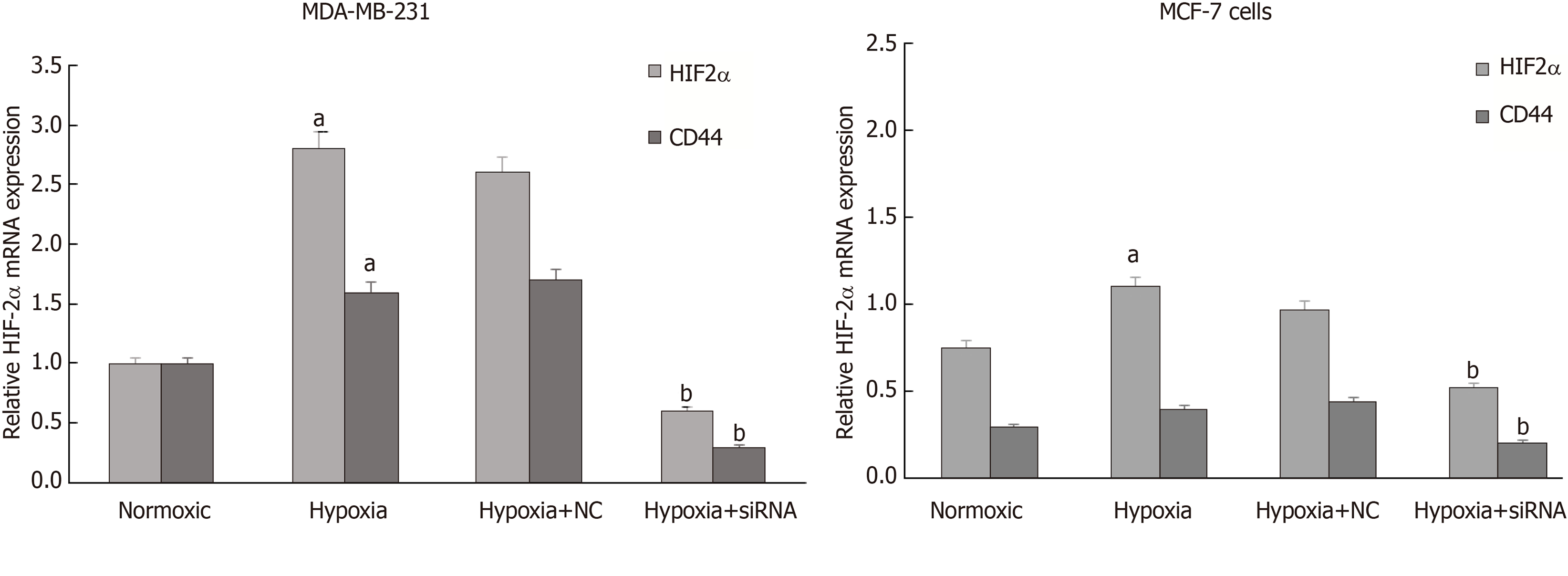
Total RNA was isolated from MDA-MB-231 and MCF-7 cells with Trizol reagent (Invitrogen, United States) and the quality of RNA was detected by 1% agarose gel electrophoresis in strict accordance with the manual. 3μg of mRNA was used as template to reverse-transcribe into cDNA, and real-time fluorescent quantitative PCR was conducted utilizing Maxima SYB RGreen /ROX qPCR Master Mix (2X) (Fermentas, United States) and the ABI 7500 real-time PCR system. The 2-ΔΔCt method was used to calculate the relative expression level of target genes. GAPDH as a housekeeping gene control was purchased from Sangon Biotech (Shanghai) Co., Ltd, and the specific primer sequences were designed using Primer 5. 0 software as follows: HIF-2α forward, 5’-GG TGAAAGTCTACAACAACTGCC-3’ and reverse, 5’-ATGGGTGCTGGATTGGTTC-3’; CD44 forward, 5’-CCAAGACACATTCCACCCCA-3’ and reverse, 5’-GCCAAGAGGGATGCCAAGAT-3’; GAPDH forward, 5’-TGGCACCCAGCACAATGAA-3’ and reverse 5’-CTAAGTCATAGTCCGC CTAGAAGCA-3’. The conditions for qPCR reactions were: 95 °C for 10 min, followed by 45 cycles of 15 s at 95 °C, 15 s at 57 °C, and 30 s at 72 °C. Melting curve analysis was performed to confirm the specificity of the target gene.
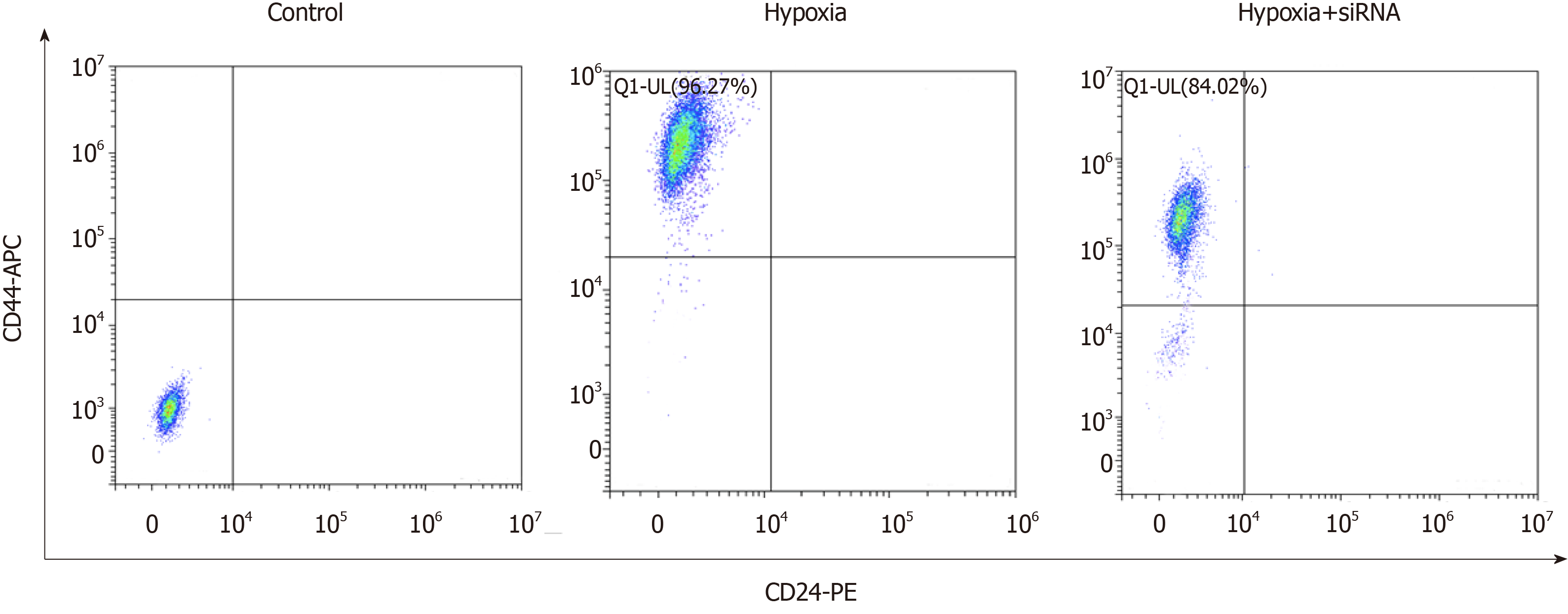
Briefly, MDA-MB-231 cells were washed once with PBS and enzymatically dissociated with trypsin-EDTA (Corning, Manassas, VA, United States). Detached cells were resuspended in PBS supplemented with 2% fetal bovine serum. The cell suspension at a density of 106 cells/100 μL were incubated with staining buffer containing monoclonal antibodies purchased from BD Biosciences (San Diego, CA, United States), including anti-human CD44-APC at a dilution of 1:40 and CD24-PE at a dilution of 1:40, for 30 to 40 min on ice, with IgG antibody labeled with APC and PE as isotype controls. Labeled cells were washed and resuspended in PBS, and analyzed on a Becton-Dickinson FACSCalibur flow cytometer. Specific CSC markers in control and HIF-2α siRNA transfected cells were detected.
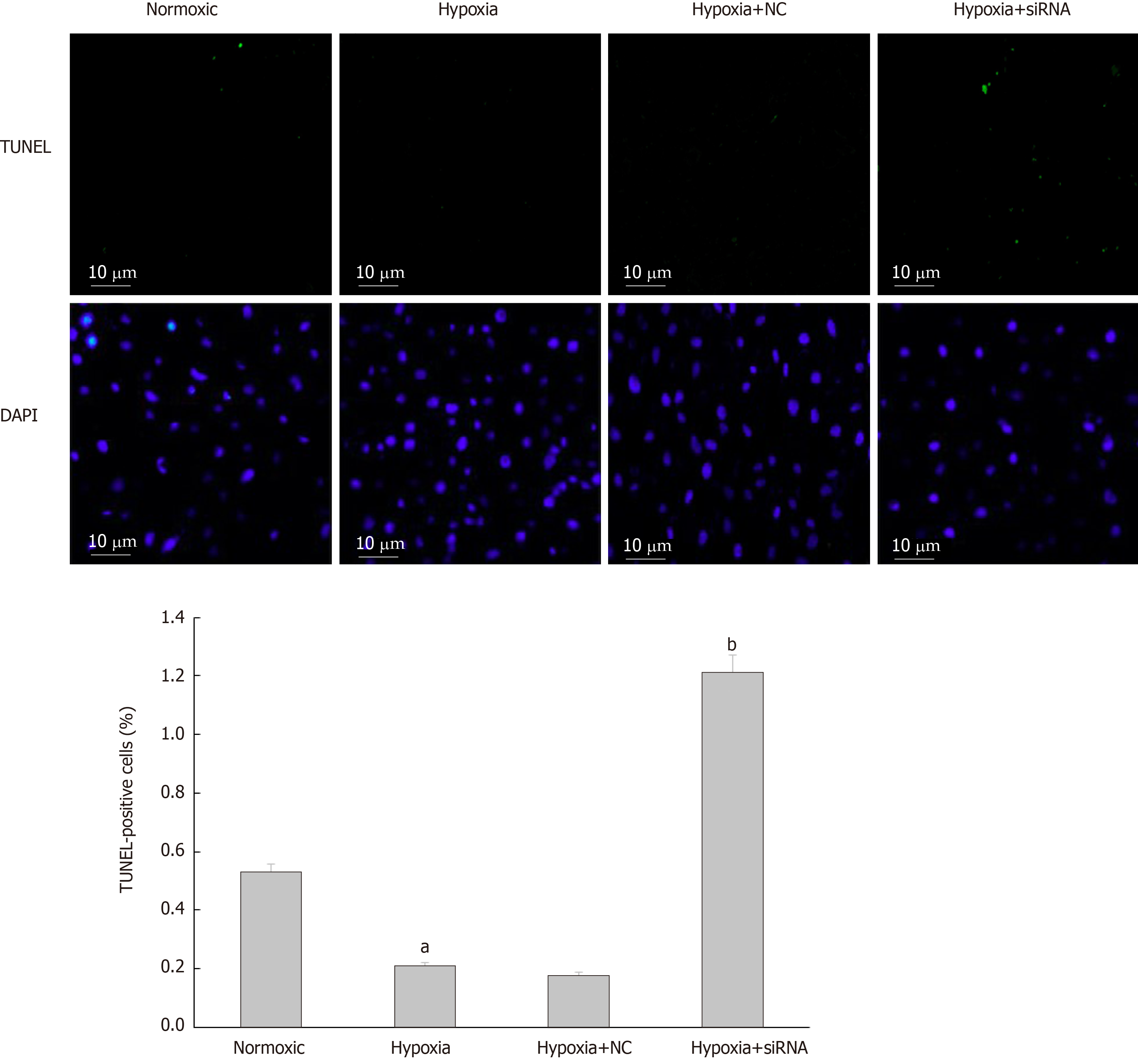
The effect of hypoxia treatment and downregulation HIF-2α on apoptosis of MDA-MB-231 cells was detected with a TUNEL assay kit following the manufacturer’s instructions (Roche Molecular Diagnostics, Pleasanton, CA, United States). In brief, cells were seeded on glass coverslips, fixed with 4% paraformaldehyde in PBS, and permeated with 0.1% Triton X-100 in 0.1% sodium citrate for 2 min on ice, after which they were incubated with 50 μL reaction mixture in a humidified chamber at 37 °C for 1 h. Then, cells were washed with PBS three times and 4',6-diamidino-2-phenylindole staining was performed for 10 min at room temperature. Five random fields of each stained section were photographed under a fluorescence microscope (Olympus Corporation, Tokyo, Japan). The percentage of TUNEL-positive cells was determined by counting cells in at least eight fields and more than 500 cells in total.
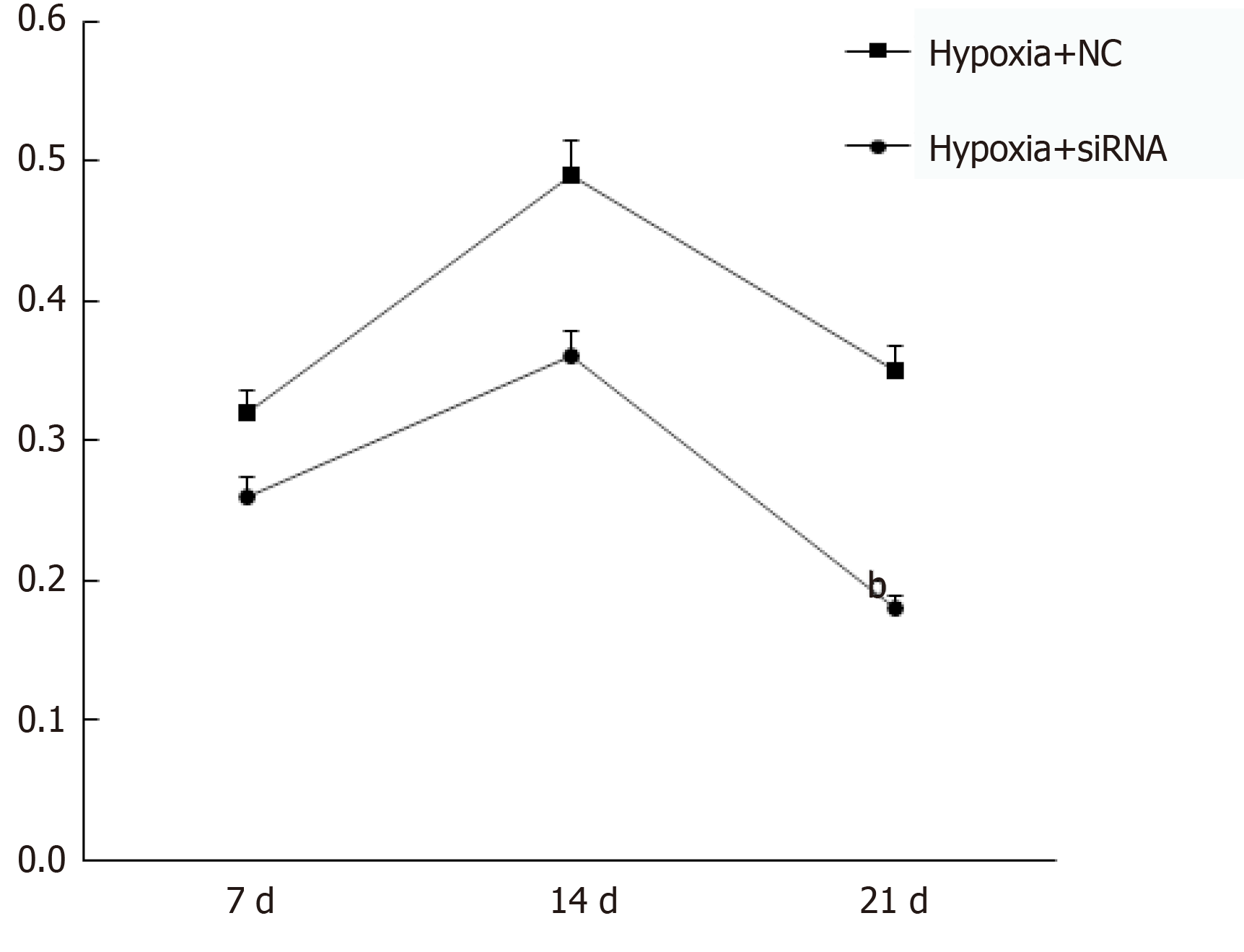
Following treatment, cells were harvested and dissociated into single cell suspension prior to filtration. Subsequently, cells were cultured in ultra-low attachment 96-well plates (Corning Incorporated, NY, United States) at a density of 1 × 105/mL. The serum-free DMEM/F-12 (HyClone, Logan, UT, United States) containing 2% B27 (Invitrogen, Carlsbed, CA, United States), 20 ng/mL b-FGF (Promega, United States), 20 ng/mL EGF (Promega, United States), and 5 μg/mL insulin was used for mammosphere culture. After culturing for 7-21 d, mammosphere were monitored and the number of mammospheres was counted with an Olympus digital camera.
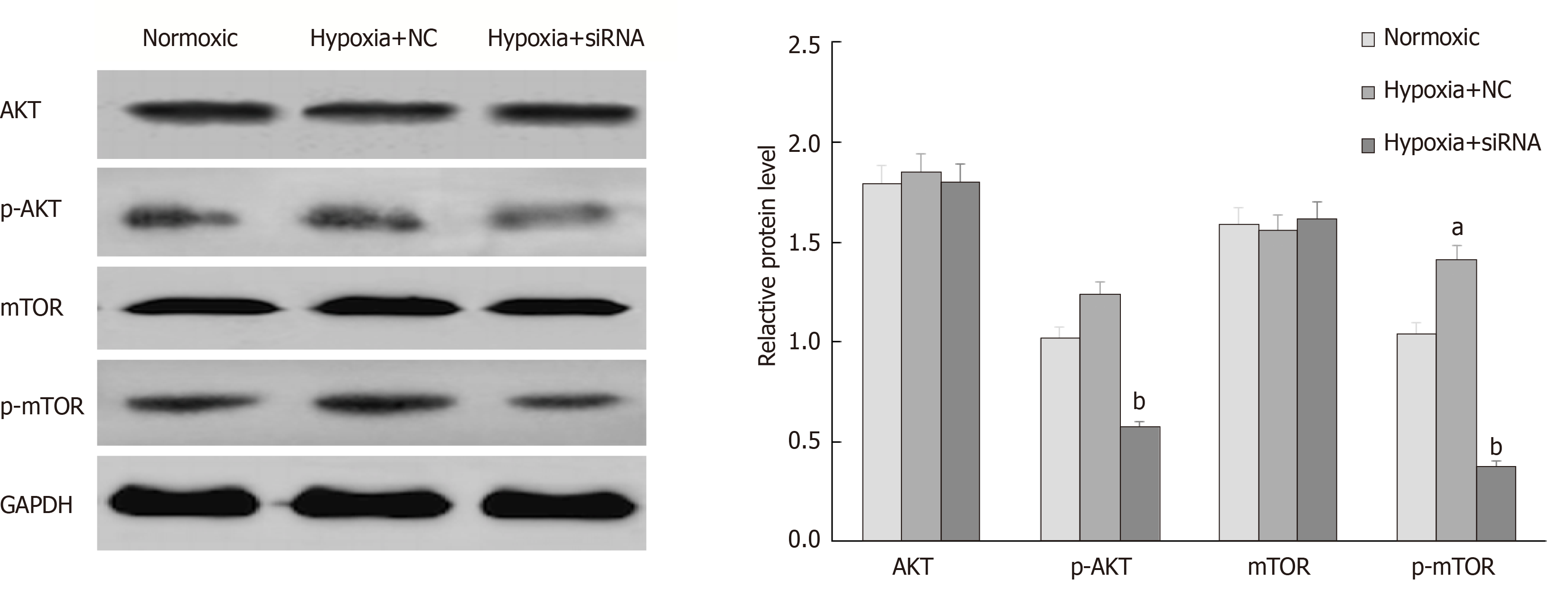
Cells were washed three times with ice-cold PBS and lysed in RIPA buffer (Beyotime, Shanghai, China) supplemented with 1% phosphatase inhibitor (Sigma-Aldrich), followed by centrifugation. The supernatant was harvested and protein concentration was determined using a bicinchoninic acid assay kit (Beyotime, Shanghai, China). Total proteins (10–30 μg) were subjected to 8%-15% sodium dodecyl sulfate-polyacrylamide gel electrophoresis. Then, the proteins were transferred to a polyvinylidene fluoride membrane (Millipore, United States), which was blocked with 5% BSA and then incubated with primary antibodies at 4 ˚C overnight. After washing, the membranes were incubated with an IgG antibody conjugated to horseradish peroxidase (dilution 1:2000) for 1 h at room temperature. Visualization of protein bands was performed with enhanced chemiluminescence solution (Thermo Fisher Scientific, Inc.), and GAPDH (Cell Signaling Technology, Danvers, United States) was used as a loading control. The primary antibodies were p-AKT (phosphor-ser473, dilution 1:500), AKT (dilution 1:500), p-mTOR (phosphor-ser2448, dilution 1:1000), and mTOR diluted to 1:1000 (Abcam, Cambridge, United Kingdom).
All data are represented as the mean ± standard deviation and analyzed with SPSS19.0 software. The independent t-test was used for two-group comparisons and one-way analysis of variance was applied to compare the means among three groups. Pairwise comparison was performed by the LSD test. P < 0.05 was considered to indicate a statistically significant difference.
In this study, we analyzed HIF-2α and CD44 expression by immunohistochemical staining. The results showed that a high density of cancer cells positive for HIF-2α was observed in both TNBC and non-TNBC cells. CD44 was highly expressed in TNBC but lowly expressed in luminal breast cancer cells. The expression of HIF-2α in different molecular types of breast cancer cells was relatively consistent, while the expression of CD44 in different molecular types of breast cancer cells was different (Figure 1).
After hypoxia treatment, immunofluorescence assay showed that HIF-2α was mainly expressed in the nucleus, while CD44 was mainly expressed on the cell membrane. It was found by image fusion that HIF-2α and CD44 were expressed almost in the same cell. The expression of HIF-2α and CD44 in MCF-7 was less than that in MDA-MB-231 cells (Figure 2).
In contrast with normoxic control, the expression of HIF-2α and CD44 mRNAs in MDA-MB-231 cells was significantly increased after induction of hypoxia. HIF-2α siRNA transfection can lower the expression of HIF-2α and CD44 mRNAs in hypoxic cells, and the difference was statistically significant (P < 0.05). The expression of HIF-2α in MCF-7 cells treated with HIF-2α siRNA and hypoxia was higher than that in cells treated by hypoxia + negative-sequence control (NC), but there was no significant difference between the normoxic control and hypoxia cells (P > 0.05) (Figure 3).
To determine the effect of HIF-2α silencing on CSC properties, we assessed the percentage of CD44+/CD24− population in hypoxia with or without HIF-2α silencing by flow cytometry. As shown in Figure 4, the percentage of CD44+/CD24− cells was 96.27% in the hypoxia group, and 84.02% in the hypoxia cells transfected with HIF-2α-siRNA. SiRNA-mediated HIF-2α depletion resulted in a reduction of CD44+/CD24− population by 12.25%.
To evaluate the effect of hypoxia and HIF-2α silencing on apoptosis in vitro, MDA-MB-231 cell apoptosis was detected using TUNEL assay. The results showed that the percentage of apoptotic cells was decreased under hypoxia compared to normoxic cells (P < 0.05). Further research found that transfection of HIF-2α–siRNA in MDA-MB-231 cells induced by hypoxia can increase the percentage of apoptotic cells than that in cells treated by hypoxia + NC, and the difference was statistically significant (P < 0.05), indicating that HIF-2α plays an important role in apoptosis of MDA-MB-231 cells (Figure 5).
From Figure 6, it is observed that mammospheres were successfully generated from MDA-MB-231 cells. In MDA-MB-231 cells, mammospheres appeared after 7 d of culture, and mammospheres of 100-200 µm in diameter formed and tended to attach after 21 d of culture. MFE of cells treated by hypoxia + NC and hypoxia + siRNA at 7 d was 0.32% ± 0.06% and 0.26% ± 0.05%, respectively. At the 21 d, MFE of the above cells was 0.33% ± 0.26% and 0.17% ± 0.09%, respectively, and the difference was statistically significant (P < 0.05). These data suggest that HIF-2α silencing significantly reduces mammosphere formation.
PI3K/AKT/mTOR signaling is commonly activated in breast cancer and plays important roles in tumor invasion and metastasis. Therefore, in this study, the main signaling molecules of the PI3K-AKT-mTOR signaling pathway including AKT, mTOR, and their phosphorylation levels were identified by Western blot analysis. The results revealed that p-AKT and p-mTOR levels in MDA-MB-231 cells increased slightly under anoxic conditions, while decreased significantly with HIF-2α knockdown, and the difference was statistically significant (P < 0.05), which suggests that hypoxia could increase the HIF-2α level to promote stem phenotype conversion via the PI3K/AKT signaling pathway (Figure 7).
CSCs are considered as cells capable of highly proliferation, self-renewal, and multidirectional differentiation, which play an important role in tumorigenesis, growth, invasion, metastasis, and recurrence[25-27]. Hypoxia can promote the dedifferentiation of differentiated cancer cells, enable cells to acquire stem cell characteristics, and enhance the invasiveness and tumorigenicity of cancer cells[28-30]. The expression of HIF-2α gene is positively correlated with the proliferation of breast cancer cells. A previous study found that HIFs and its target genes are highly expressed in TNBC[31]. Under hypoxic conditions, the expression of HIF-1α increased rapidly and generally decreased sharply within 2-12 h, while the expression of HIF-2α began to increase 48-72 h after hypoxia, and then continued to express steadily for about 2 wk[32-34]. Therefore, we believe that HIF-2α may play a more important role in tumors and other chronic hypoxic diseases. In this study, we found that HIF-2α was highly expressed in both TNBC and non-TNBC, and was higher in TNBC. This result is consistent with the findings of Goggins et al[35]. Further, clinical studies have shown that high expression of HIF-2α suggests a poor prognosis for both locally advanced breast cancer and early breast cancer patients[36-38].
The reduction of breast cancer recurrence rate and improvement of its cure rate in clinical practice are based on in-depth exploration of CSCs[39-41]. Therefore, this study analyzed the relationship between HIF-2α and CD44 by immunofluorescence after hypoxia treatment, and the results showed that HIF-2α and CD44 were expressed almost in the same cell, leading us to hypothesize that there is a close relationship between CD44 and HIF-2α. The latter may regulate the expression of the former, but the specific regulatory mechanism still needs to be further explored. Furthermore, RNA interference, flow cytometry, and TUNEL assays were applied to identify the effect of HIF-2α expression on the biological function of CSCs in breast cancer cells. In this experiment, it was found that the expression of HIF-2α mRNA in MDB-MB-231 and MCF-7 cells was significantly increased under hypoxic conditions, while significantly decreased after specific HIF-2α siRNA transfection, indicating successful cell transfection. Moreover, the results also showed that HIF-2α silencing can lower the expression of HIF-2α and CD44 mRNAs in hypoxic cells, suggesting that HIF-2α could affect the level of CD44.
In breast cancers, CSCs carry the phenotypic signature of being CD24-/CD44+[42]. Flow cytometry showed that the proportion of CD44 cells in hypoxia-induced cells was significantly lower than that in the hypoxia control group after HIF-2α down-regulation. The results confirmed that down-regulation of HIF-2α in hypoxic microenvironment can slow the formation of MDA-MB-231 tumor stem cells, and the results are consistent with those of Xie et al[43]. It is suggested that HIF-2α plays an important role in maintaining the stemness of CSCs. Alternatively, TUNEL assay showed that HIF-2α siRNA in MDA-MB-231 cells induced by hypoxia can increase the percentage of apoptotic cells, and high-level HIF-2α was believed to be linked to an increased risk of breast cancer recurrence and metastasis[44,45]. Invasion and metastasis are important factors affecting the prognosis of tumor patients. It was found that the percentage of apoptotic cells was decreased under hypoxic conditions, and increased after transfection of specific HIF-2α siRNA, which further confirms that HIF-2α can promote the migration and invasion of breast cancer cells and inhibit the apoptosis of breast cancer cells.
Activation of the PI3K/mTOR/mTOR signaling pathway is very common in breast cancer patients[46,47]. Whole-genome sequencing in ER-positive metastatic breast cancer patients revealed frequent mutations in many genes. Sharma et al[48] showed that p7170, a dual inhibitor of PI3K/mTOR, has a strong inhibitory effect on proliferation of endocrine-sensitive and -resistant ER+/Her-2- breast cancer cells. In this study, we hypothesized that HIF-2α silencing mediated by siRNA in human breast cancer MDA-MB-231 cells can inhibit the expression of CD44, thus inhibiting the expression of the intracellular p-AKT and p-mTOR, and the migration and invasion of cancer cells were suppressed.
In conclusion, down-regulation of HIF-2α expression can inhibit the stemness of human breast cancer MDA-MB-231 cells and promote apoptosis, and its mechanism may be related to the CD44/PI3K/AKT/mTOR signaling pathway, which is expected to be a target for the treatment of TNBC.
Breast cancer has a high degree of phenotype and functional heterogeneity, and the intratumoral variation is obvious. Traditional chemical and endocrine therapies are not effective in treating all cells in a tumor. Researchers have found a small group of highly tumorigenic cell populations in breast tumors. They have stem cell-like properties that are critical for tumorigenesis, progression, progression, and recurrence, and are closely associated with breast cancer metastasis. In the development of tumors, hypoxia-inducible factor-2α (HIF-2α) plays an important role in enhancing the drug resistance and migration of breast cancer stem cells. At present, whether the expression of cancer stem cells can be regulated by interfering with the expression of HIF-2α has not been reported in the literature.
Due to the rapid growth of triple-negative breast cancer (TNBC), and the lack of self-vascular supply to meet the needs of rapidly growing tumor cells, a hypoxic environment is gradually formed. In the long-term chronic hypoxia of tumors, the major regulatory factor is HIF-2α, which increases the malignant biological behavior of tumors by activating its downstream target genes. As a marker of breast cancer stem cells, CD44 is closely related to the invasion and metastasis of tumor cells. Previous studies have found that HIF-2α can regulate the expression of the cell adhesion molecule CD44, but the relationship between the two and the regulatory mechanism are not clear.
This study analyzed the relationship between the expression of HIF-2α and CD44 in patients with TNBC and non-TNBC. Then, the effects of HIF-2α on the expression of CD44 in human breast cancer cell lines MCF-7 and MDA-MB-231 and its possible mechanism were explored.
We analyzed the expression of HIF-2α and CD44 in patients with TNBC (n = 29) and non-TNBC (n = 20) using immunohistochemistry. The co-expression of HIF-2α and CD44 in MDA-MB-231 cells and MCF-7 cells was characterized by double-labeling immunofluorescence. The impact of siRNA-mediated HIF-2α knockdown on the CSCs and apoptosis of MDA-MB-231 cells was detected by real-time fluorescent quantitative PCR, flow cytometry, TUNEL, and mammosphere formation assays. Data were statistically analyzed using the independent t-test and one-way analysis of variance followed by LSD pairwise comparison tests.
Our data showed that HIF-2α had a high level expression in both TNBC and non-TNBC, and HIF-2α and CD44 were located in the same cell. Functionally, HIF-2α silencing significantly reduced the expression of HIF-2α and CD44 mRNAs, but increased cell apoptosis. Flow cytometry and mammosphere formation assay results indicated downregulation of CD44+/CD24− population (P < 0.05) and mammosphere formation upon HIF-2α suppression in hypoxic MDA-MB-231 cells. Moreover, HIF-2α siRNA transfection could decrease the levels of phosphorylated protein-serine-threonine kinase (p-AKT) and phosphorylated mammalian target of rapamycin (p-mTOR) in MDA-MB-231 cells.
HIF-2α plays an important role in the stemness and apoptosis of human breast cancer MDA-MB-231 cells via the CD44/PI3K/AKT/mTOR signaling pathway, thus emerging as a target for the treatment of TNBC.
The molecular regulation mechanism of CSCs in TNBC tissues is still unclear. Inhibition of CSC activation or elimination of CSCs has become a difficult and critical step in the current treatment of TNBC. In this study, the effect of HIF-2α on CSCs was explored by clinicopathological specimens and in vitro experiments, and the mechanism of action was preliminarily analyzed. The conclusions of this study have important clinical and pathological significance for understanding the mechanism of CSC activation in TNBC tissues, blocking the signaling pathway of HIF-2α, inhibiting the malignant progression of TNBC, and improving the prognosis of patients.
Manuscript source: Unsolicited manuscript
Specialty type: Cell and tissue engineering
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kruis W, Reich K, Manuel CF S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, Seruga B, Ocaña A, Tannock IF, Amir E. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014;23:1204-1212. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 373] [Cited by in F6Publishing: 451] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 2. | Neil-Sztramko SE, Winters-Stone KM, Bland KA, Campbell KL. Updated systematic review of exercise studies in breast cancer survivors: attention to the principles of exercise training. Br J Sports Med. 2019;53:504-512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 3. | Brandão T, Schulz MS, Matos PM. Psychological adjustment after breast cancer: a systematic review of longitudinal studies. Psychooncology. 2017;26:917-926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 4. | Ennour-Idrissi K, Maunsell E, Diorio C. Telomere Length and Breast Cancer Prognosis: A Systematic Review. Cancer Epidemiol Biomarkers Prev. 2017;26:3-10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Lee JD, Cai Q, Shu XO, Nechuta SJ. The Role of Biomarkers of Oxidative Stress in Breast Cancer Risk and Prognosis: A Systematic Review of the Epidemiologic Literature. J Womens Health (Larchmt). 2017;26:467-482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 6. | Terranova CO, Protani MM, Reeves MM. Overall Dietary Intake and Prognosis after Breast Cancer: A Systematic Review. Nutr Cancer. 2018;70:153-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Dent R, Valentini A, Hanna W, Rawlinson E, Rakovitch E, Sun P, Narod SA. Factors associated with breast cancer mortality after local recurrence. Curr Oncol. 2014;21:e418-e425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Poggio F, Bruzzone M, Ceppi M, Pondé NF, La Valle G, Del Mastro L, de Azambuja E, Lambertini M. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and meta-analysis. Ann Oncol. 2018;29:1497-1508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 249] [Article Influence: 49.8] [Reference Citation Analysis (0)] |
| 9. | Li L, Zhong Y, Zhang H, Yu H, Huang Y, Li Z, Chen G, Hua X. Association between oral contraceptive use as a risk factor and triple-negative breast cancer: A systematic review and meta-analysis. Mol Clin Oncol. 2017;7:76-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P, Narod SA. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13:4429-4434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2803] [Cited by in F6Publishing: 3240] [Article Influence: 190.6] [Reference Citation Analysis (0)] |
| 11. | Pindiprolu SKSS, Krishnamurthy PT, Chintamaneni PK. Pharmacological targets of breast cancer stem cells: a review. Naunyn Schmiedebergs Arch Pharmacol. 2018;391:463-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Mansoori M, Madjd Z, Janani L, Rasti A. Circulating cancer stem cell markers in breast carcinomas: a systematic review protocol. Syst Rev. 2017;6:262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Chen X, Liu Q, Song E. Mammary stem cells: angels or demons in mammary gland? Signal Transduct Target Ther. 2017;2:16038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Liu M, Liu Y, Deng L, Wang D, He X, Zhou L, Wicha MS, Bai F, Liu S. Transcriptional profiles of different states of cancer stem cells in triple-negative breast cancer. Mol Cancer. 2018;17:65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Ren D, Zhu X, Kong R, Zhao Z, Sheng J, Wang J, Xu X, Liu J, Cui K, Zhang XH, Zhao H, Wong STC. Targeting Brain-Adaptive Cancer Stem Cells Prohibits Brain Metastatic Colonization of Triple-Negative Breast Cancer. Cancer Res. 2018;78:2052-2064. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Shi P, Liu W, Tala, Wang H, Li F, Zhang H, Wu Y, Kong Y, Zhou Z, Wang C, Chen W, Liu R, Chen C. Metformin suppresses triple-negative breast cancer stem cells by targeting KLF5 for degradation. Cell Discov. 2017;3:17010. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 17. | Lu H, Samanta D, Xiang L, Zhang H, Hu H, Chen I, Bullen JW, Semenza GL. Chemotherapy triggers HIF-1-dependent glutathione synthesis and copper chelation that induces the breast cancer stem cell phenotype. Proc Natl Acad Sci U S A. 2015;112:E4600-E4609. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 18. | Samanta D, Gilkes DM, Chaturvedi P, Xiang L, Semenza GL. Hypoxia-inducible factors are required for chemotherapy resistance of breast cancer stem cells. Proc Natl Acad Sci U S A. 2014;111:E5429-E5438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 345] [Cited by in F6Publishing: 377] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 19. | Carroll VA, Ashcroft M. Role of hypoxia-inducible factor (HIF)-1alpha versus HIF-2alpha in the regulation of HIF target genes in response to hypoxia, insulin-like growth factor-I, or loss of von Hippel-Lindau function: implications for targeting the HIF pathway. Cancer Res. 2006;66:6264-6270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 265] [Cited by in F6Publishing: 274] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 20. | Kwak JH, Lee NH, Lee HY, Hong IS, Nam JS. HIF2α/EFEMP1 cascade mediates hypoxic effects on breast cancer stem cell hierarchy. Oncotarget. 2016;7:43518-43533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Kim RJ, Park JR, Roh KJ, Choi AR, Kim SR, Kim PH, Yu JH, Lee JW, Ahn SH, Gong G, Hwang JW, Kang KS, Kong G, Sheen YY, Nam JS. High aldehyde dehydrogenase activity enhances stem cell features in breast cancer cells by activating hypoxia-inducible factor-2α. Cancer Lett. 2013;333:18-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 22. | Johansson E, Grassi ES, Pantazopoulou V, Tong B, Lindgren D, Berg TJ, Pietras EJ, Axelson H, Pietras A. CD44 Interacts with HIF-2α to Modulate the Hypoxic Phenotype of Perinecrotic and Perivascular Glioma Cells. Cell Rep. 2017;20:1641-1653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 23. | Covello KL, Kehler J, Yu H, Gordan JD, Arsham AM, Hu CJ, Labosky PA, Simon MC, Keith B. HIF-2alpha regulates Oct-4: effects of hypoxia on stem cell function, embryonic development, and tumor growth. Genes Dev. 2006;20:557-570. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 610] [Cited by in F6Publishing: 620] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 24. | Koh MY, Lemos R, Liu X, Powis G. The hypoxia-associated factor switches cells from HIF-1α- to HIF-2α-dependent signaling promoting stem cell characteristics, aggressive tumor growth and invasion. Cancer Res. 2011;71:4015-4027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 217] [Cited by in F6Publishing: 244] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 25. | Luo M, Clouthier SG, Deol Y, Liu S, Nagrath S, Azizi E, Wicha MS. Breast cancer stem cells: current advances and clinical implications. Methods Mol Biol. 2015;1293:1-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 26. | Bettaieb A, Paul C, Plenchette S, Shan J, Chouchane L, Ghiringhelli F. Precision medicine in breast cancer: reality or utopia? J Transl Med. 2017;15:139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 27. | Lowry MC, Gallagher WM, O'Driscoll L. The Role of Exosomes in Breast Cancer. Clin Chem. 2015;61:1457-1465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 28. | Semenza GL. Hypoxia-inducible factors: coupling glucose metabolism and redox regulation with induction of the breast cancer stem cell phenotype. EMBO J. 2017;36:252-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 248] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 29. | Schito L, Rey S. Hypoxic pathobiology of breast cancer metastasis. Biochim Biophys Acta Rev Cancer. 2017;1868:239-245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 30. | Liu J, Zhang C, Zhao Y, Yue X, Wu H, Huang S, Chen J, Tomsky K, Xie H, Khella CA, Gatza ML, Xia D, Gao J, White E, Haffty BG, Hu W, Feng Z. Parkin targets HIF-1α for ubiquitination and degradation to inhibit breast tumor progression. Nat Commun. 2017;8:1823. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 137] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 31. | Lv Y, Chen C, Zhao B, Zhang X. Regulation of matrix stiffness on the epithelial-mesenchymal transition of breast cancer cells under hypoxia environment. Naturwissenschaften. 2017;104:38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Schöning JP, Monteiro M, Gu W. Drug resistance and cancer stem cells: the shared but distinct roles of hypoxia-inducible factors HIF1α and HIF2α. Clin Exp Pharmacol Physiol. 2017;44:153-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 33. | Shan C, Zheng Y, Wang M, Lin S, Tian T, Deng Y, Xu P, Hao Q, Wu Y, Yang T, Guo Y, Dai Z. Polymorphisms in HIFs and breast cancer sutarsceptibility in Chinese women: a case-control study. Biosci Rep. 2018;38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Påhlman S, Lund LR, Jögi A. Differential HIF-1α and HIF-2α Expression in Mammary Epithelial Cells during Fat Pad Invasion, Lactation, and Involution. PLoS One. 2015;10:e0125771. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Goggins E, Kakkad S, Mironchik Y, Jacob D, Wildes F, Krishnamachary B, Bhujwalla ZM. Hypoxia Inducible Factors Modify Collagen I Fibers in MDA-MB-231 Triple Negative Breast Cancer Xenografts. Neoplasia. 2018;20:131-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Regan Anderson TM, Ma SH, Raj GV, Cidlowski JA, Helle TM, Knutson TP, Krutilina RI, Seagroves TN, Lange CA. Breast Tumor Kinase (Brk/PTK6) Is Induced by HIF, Glucocorticoid Receptor, and PELP1-Mediated Stress Signaling in Triple-Negative Breast Cancer. Cancer Res. 2016;76:1653-1663. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Bharti SK, Mironchik Y, Wildes F, Penet MF, Goggins E, Krishnamachary B, Bhujwalla ZM. Metabolic consequences of HIF silencing in a triple negative human breast cancer xenograft. Oncotarget. 2018;9:15326-15339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | Karousou E, Misra S, Ghatak S, Dobra K, Götte M, Vigetti D, Passi A, Karamanos NK, Skandalis SS. Roles and targeting of the HAS/hyaluronan/CD44 molecular system in cancer. Matrix Biol. 2017;59:3-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 39. | Yang F, Xu J, Tang L, Guan X. Breast cancer stem cell: the roles and therapeutic implications. Cell Mol Life Sci. 2017;74:951-966. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 40. | Schwarz-Cruz Y Celis A, Espinosa M, Maldonado V, Melendez-Zajgla J. Advances in the knowledge of breast cancer stem cells. A review. Histol Histopathol. 2016;31:601-612. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 7] [Reference Citation Analysis (0)] |
| 41. | Zhang L, Wen X, Li M, Li S, Zhao H. Targeting cancer stem cells and signaling pathways by resveratrol and pterostilbene. Biofactors. 2018;44:61-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 42. | Goyette S, Liang Y, Mafuvadze B, Cook MT, Munir M, Hyder SM. Natural and synthetic progestins enrich cancer stem cell-like cells in hormone-responsive human breast cancer cell populations in vitro. Breast Cancer (Dove Med Press). 2017;9:347-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 43. | Xie G, Liu Y, Yao Q, Zheng R, Zhang L, Lin J, Guo Z, Du S, Ren C, Yuan Q, Yuan Y. Hypoxia-induced angiotensin II by the lactate-chymase-dependent mechanism mediates radioresistance of hypoxic tumor cells. Sci Rep. 2017;7:42396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Fuady JH, Gutsche K, Santambrogio S, Varga Z, Hoogewijs D, Wenger RH. Estrogen-dependent downregulation of hypoxia-inducible factor (HIF)-2α in invasive breast cancer cells. Oncotarget. 2016;7:31153-31165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 45. | Shiraishi A, Tachi K, Essid N, Tsuboi I, Nagano M, Kato T, Yamashita T, Bando H, Hara H, Ohneda O. Hypoxia promotes the phenotypic change of aldehyde dehydrogenase activity of breast cancer stem cells. Cancer Sci. 2017;108:362-372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Deng L, Chen J, Zhong XR, Luo T, Wang YP, Huang HF, Yin LJ, Qiu Y, Bu H, Lv Q, Zheng H. Correlation between activation of PI3K/AKT/mTOR pathway and prognosis of breast cancer in Chinese women. PLoS One. 2015;10:e0120511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 47. | Pierobon M, Ramos C, Wong S, Hodge KA, Aldrich J, Byron S, Anthony SP, Robert NJ, Northfelt DW, Jahanzeb M, Vocila L, Wulfkuhle J, Gambara G, Gallagher RI, Dunetz B, Hoke N, Dong T, Craig DW, Cristofanilli M, Leyland-Jones B, Liotta LA, O'Shaughnessy JA, Carpten JD, Petricoin EF. Enrichment of PI3K-AKT-mTOR Pathway Activation in Hepatic Metastases from Breast Cancer. Clin Cancer Res. 2017;23:4919-4928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 48. | Sharma VR, Gupta GK, Sharma AK, Batra N, Sharma DK, Joshi A, Sharma AK. PI3K/Akt/mTOR Intracellular Pathway and Breast Cancer: Factors, Mechanism and Regulation. Curr Pharm Des. 2017;23:1633-1638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |