Published online Dec 14, 2016. doi: 10.3748/wjg.v22.i46.10260
Peer-review started: July 15, 2016
First decision: August 29, 2016
Revised: September 13, 2016
Accepted: September 28, 2016
Article in press: September 28, 2016
Published online: December 14, 2016
Schwannomas are mesenchymal neoplasms with low malignant potential that arise from Schwann cells. They can occur almost anywhere, although the most common locations are the head, neck and extremities. Primary benign schwannoma of the hepatoduodenal ligament is rare. To date, only three cases have been reported in the English literature. In the present study, we report a case of hepatoduodenal ligament schwannoma in a 43-year-old male, who was admitted to our hospital because of a abdominal mass found by physical examination. It was hard to determine the definitive location and diagnosis of the mass using ultrasound, computed tomography and magnetic resonance cholangiopancreatography. During laparotomy, the mass was found in the hepatoduodenal ligament and close to the cholecystic duct, so we resected the gallbladder and cholecystic duct along with the mass. The gross specimen revealed an 8.5 cm × 5.5 cm × 3.0 cm localized tumor. Microscopic examination showed that the tumor was mainly composed of spindle-shaped cells. Immunohistochemical staining showed a strong positive S-100 protein reaction. Finally, the lesion was diagnosed as a benign schwannoma in the hepatoduodenal ligament. However, one month later, the patient was readmitted to our hospital because of skin and sclera jaundice caused by common bile duct stenosis without common bile duct stone or tumor. The patient recovered well after implantation of a common bile duct stent under endoscopic retrograde cholangiopancreatography. He was followed up for a period of 17 mo, during which he was well with no complications.
Core tip: To date, only three cases of the hepatoduodenal ligament schwannomas have been reported in the English literature. We present the fourth hepatoduodenal ligament schwannoma. It is challenging to determine the location and obtain a precise diagnosis prior to operation. Following complete tumor excision, patients with benign schwannomas generally have a good prognosis. Common bile duct stenosis after resection of the schwannoma in hepatoduodenal ligament has not been reported and we present the first one cured by implanting a common bile duct stent under endoscopic retrograde cholangiopancreatography. We also conduct a literature review so as to deepen the understanding of the subject.
- Citation: Xu SY, Sun K, Xie HY, Zhou L, Zheng SS, Wang WL. Schwannoma in the hepatoduodenal ligament: A case report and literature review. World J Gastroenterol 2016; 22(46): 10260-10266
- URL: https://www.wjgnet.com/1007-9327/full/v22/i46/10260.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i46.10260
Schwannomas are neurogenic tumors originating from the Schwann cells in nerve sheaths[1]. They can occur in patients at all ages with no obvious gender difference. As revealed by cytogenetic analysis, most schwannomas showed either monosomy 22 or loss of 22q material[2]. More than 90% of schwannomas are benign and comprise about 5% of benign soft-tissue neoplasms[3,4]. They can arise in almost every location, although the most common sites are the head, neck and extremities[5]. Schwannomas in the hepatoduodenal ligament are uncommon and only three cases have been reported in the English literature[6-8]. Patients with schwannomas in the hepatoduodenal ligament are normally asymptomatic and the tumors are found incidentally. We present a case of hepatoduodenal ligament schwannoma in a 43-year-old male and review the literature. He is believed to be the first patient with subsequent common bile duct stenosis after complete removal of hepatoduodenal ligament schwannoma and to be cured by implantation of a common bile duct stent under endoscopic retrograde cholangiopancreatography (ERCP).
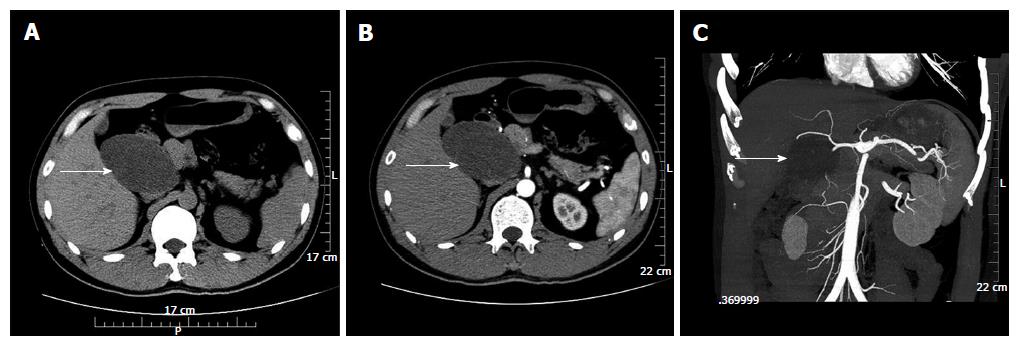
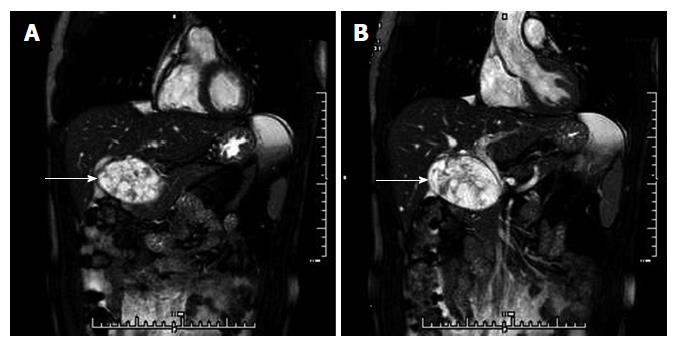
On November 21, 2014, a 43-year-old male was admitted to our hospital for physical examination. His abdomen was soft, lax and nondistended without evidence of a palpable mass. His family history had no significant disease. Laboratory results were normal. Ultrasound (US) revealed an 8.3 cm × 5.2 cm, well-defined hypodense lesion, between the pancreatic head and portal vein. No blood flow signal was found within the mass by Color Doppler US. An unenhanced computed tomography (CT) scan showed an 8.2 cm × 5.1 cm well-defined cystic and solid mass above the pancreatic head and adjacent to the common hepatic artery. The pancreaticoduodenal artery was compressed by the mass. On contrast-enhanced CT, the mass showed no obvious enhancement (Figure 1B). Computed tomography angiography showed that the blood supply of the tumor was probably from the branches of the pancreaticoduodenal artery (Figure 1C). Magnetic resonance cholangiopancreatography (MRCP) showed that the mass was inhomogeneous and hyperintense on T2-weighted images and probably located in the pancreatic head, and the middle-low segment of the common bile duct was compressed (Figure 2). According to the imaging examinations, an abdominal mass was primarily considered.
After sufficient preoperative preparation, exploratory laparotomy was performed. We found a mass surrounded by a fibrous capsule in the hepatoduodenal ligament, closely adjacent to the gallbladder, cholecystic duct, common bile duct, portal vein, right hepatic artery, duodenum and postcava, without biliary duct dilatation. The tumor blood supply was mainly from the surrounding vessels of the duodenum. We carefully separated these tissues around the tumor and ligated the tumor blood vessels. However, the mass and cholecystic duct were too close to separate, so we resected the gallbladder and cholecystic duct along with the mass. Intraoperative frozen-section pathology could not offer an accurate diagnosis and only suggested a soft-tissue tumor.
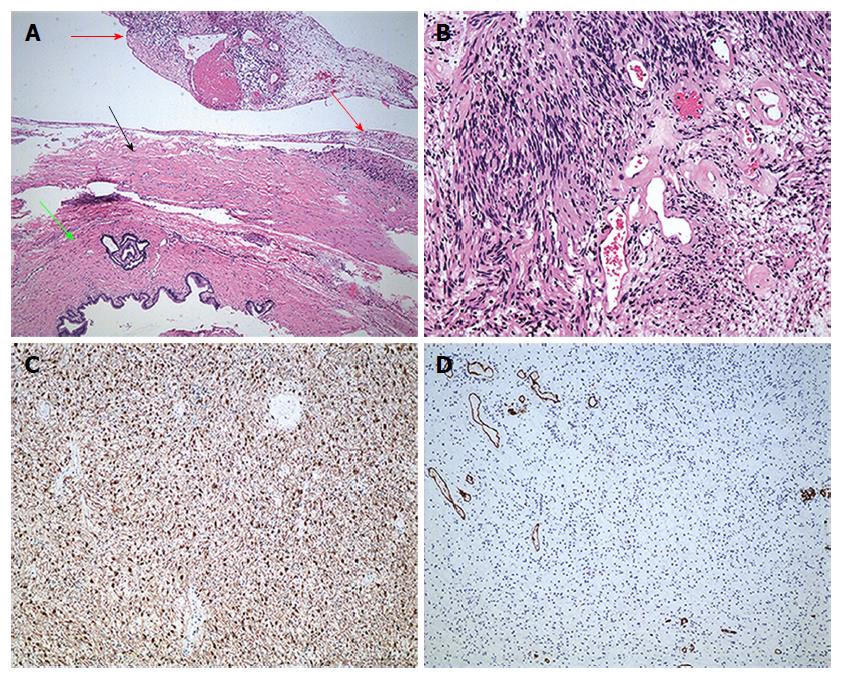
Macroscopically, there was a mass in the hepatoduodenal ligament 8.5 cm × 5.5 cm × 3.0 cm in size and yellowish-white in color. Microscopically, the tumor had a capsule that was adjacent to the cholecystic duct (Figure 3A) and mainly consisted of spindle-shaped cells with no atypia, compatible with a benign schwannoma with both hypercellular and hypocellular areas visible (Figure 3B). Immunohistochemical investigation showed that protein S-100 was positive (Figure 3C), while CD34 (Figure 3D), CD117 and smooth muscle actin (SMA) were negative. Finally, the tumor was diagnosed as schwannoma in the hepatoduodenal ligament. After surgery, the patient recovered uneventfully and left the hospital 6 d later.
However, one month later, the patient was readmitted to our hospital because of skin and sclera jaundice without abdominal distension, abdominal pain, fever, nausea and vomiting. Laboratory results were: total bilirubin 113 μmol/L (0-21), direct bilirubin 76 μmol/L (0-5), indirect bilirubin 37 μmol/L (3-14), aspartate transaminase 301 U/L (8-40), alanine transaminase 543 U/L (5-35), alkaline phosphatase 452 U/L (40-150), γ-glutamyl transpeptidase (GGT) 441 U/L (11-50) and creatinine 90 μmol/L (45-84). No other abnormal laboratory results were found.
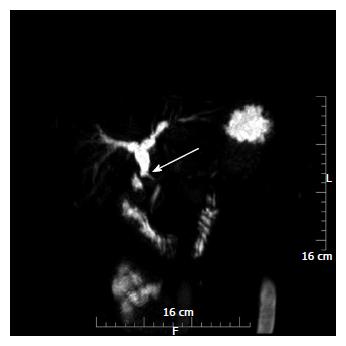
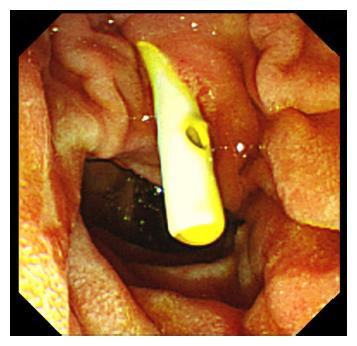
US showed that the intra- and extrahepatic bile ducts were expanded. The diameter of the initial segment of the common bile duct was 1.1 cm with no mass or stones in the duct. MRCP showed that the middle common bile duct segment was narrow and even interrupted, while the higher common bile duct segment and intrahepatic bile ducts were expanded (Figure 4). So, the patient was diagnosed with jaundice caused by common bile duct stenosis. Under ERCP, we implanted a stent into the strictured common bile duct (Figure 5). One day later, the patient recovered well and left our hospital. He was followed up for 17 mo, during which, he was well with no complications.
Schwannomas are neoplasms that originate from Schwann cells of nerve sheaths[9]. More than 90% of schwannomas are benign and comprise only approximately 5% of benign soft-tissue neoplasms[5]. Schwannomas can occur in patients at any age with no significant gender difference, but are most commonly found in patients between 20 and 50 years old[5]. They can arise almost anywhere, although the head, neck and extremities are the most common sites[10]. In the abdominal cavity, the retroperitoneum (6% of primary retroperitoneal tumors)[11] and stomach[12] are the most frequently involved sites. However, schwannomas in the ligaments[13], bowel mesentery[14] and abdominal organs including the gallbladder[15], pancreas[16] and liver[17] are rare. To the best of our knowledge, only three cases of schwannoma in the hepatoduodenal ligament have been reported[6-8]. The clinical characteristics of these cases including the present one are shown in Table 1. One patient was female and the other three patients were male, aged 62, 29, 50 and 43 years, respectively (mean age, 46 years). One patient presented with pain in the right abdomen following trauma and a mass in the hepatoduodenal ligament was occasionally found by imaging. The remaining patients were all asymptomatic and the masses were found by routine physical examination. Although every patient received more than two imaging examinations, none was accurately diagnosed as schwannoma in the hepatoduodenal ligament preoperatively.
| Ref. | Year | Sex/age | Symptom | Imaging method | No. | Size (cm) | Preoperative diagnosis | Treatment | Follow-up (mo) | Status |
| Nagafuchi et al[6] | 1993 | F/62 | Asymptomatic | US, CT, ERC, CA | Solitary | 9 × 5 × 4.5 | NA | Laparotomy | 26 | Survived |
| Pinto et al[7] | 2011 | M/29 | Asymptomatic | US, endoscopy, US, biopsy, MRI | Solitary | 4.5 × 2.9 | Spindle cell neoplasia or stromal tumor | Laparotomy | NA | NA |
| Tao et al[8] | 2016 | M/50 | Right abdominal pain | US, CT | Solitary | 4.5 × 2.5 × 2.5 | Stromal tumor | Laparoscopic surgery | 7 | Survived |
| Present case | 2016 | M/43 | Asymptomatic | US, CT, MRCP, CTA, ERCP | Solitary | 8.5 × 5.5 × 3.0 | Abdominal mass | Laparotomy | 17 | Survived |
Accurate preoperative diagnosis of the tumor is a huge challenge because neither the clinical symptoms nor the radiological characteristics of schwannomas are specific. Definitive diagnosis can only be determined by histopathological and immunohistochemical examinations of surgical specimens. Schwannomas are encapsulated tumors that consist of hypercellular (Antoni type A) and hypocellular (Antoni type B) areas, with varying amounts of these two histological components[8]. The former is composed of closely packed spindle cells with occasional nuclear palisading, as well as Verocay bodies. The latter consists of loosely arranged tumor cells and abundant myxoid stroma. Occasionally, these may degenerate and become cystic[8]. Immunohistochemically, schwannomas are strongly positive for S-100, and negative for desmin, smooth muscle myosin, SMA, CD34 and CD117[18].
Precise diagnosis of these tumors prior to operation is difficult. Multiple imaging modalities including US, CT and magnetic resonance imaging (MRI) can be performed to establish a probable diagnosis. Schwanommas are usually showed as well-defined hypodense lesions by US and no echoic enhancement is demonstrated by Color Doppler US[8]. On unenhanced CT, schwannomas are usually well-defined hypodense lesions with encapsulation and/or cystic degeneration. Schwannomas with high Antoni A areas appear inhomogeneous due to increased lipid content. Antoni B areas of schwannomas appear cystic and multiseptated and show low density due to loose stroma and low cellularity[2]. On contrast-enhanced CT, Antoni A areas are usually enhancing lesions, whereas Antoni B areas are frequently nonenhancing lesions[8]. On MRI, the schwanommas typically appear hypointense on T1-weighted images and inhomogeneous and hyperintense on T2-weighted images[2,19]. By outlining the degree of vascular involvement of the tumor, MRI is also useful to assess the potential biological behavior of these tumors as benign or malignant[19]. Endoscopic US (EUS) is helpful to clarify the location and nature of the mass[7]. In addition, celiac angiography can be used to indicate the arteries supplying the tumor[6]. EUS-fine needle aspiration (FNA) may contribute to precise preoperative diagnosis. In a case reported by Li et al[20], a pancreatic schwannoma was accurately diagnosed preoperatively by EUS-FNA. In another report, three cases of asymptomatic retroperitoneal tumors were diagnosed as benign schwannomas by EUS-FNA, thus avoiding surgical resection[21].
Surgery can demonstrate the tumor site and be curative. In the present case, we found by laparotomy that the mass was located in the hepatoduodenal ligament and adjacent to important tissues and organs including the gallbladder, cholecystic duct, common bile duct, duodenum and postcava. The tumor vascular supply was mainly from the surrounding vessels of the duodenum. We carefully separated these tissues around the tumor and ligated the blood vessels. However, the mass and cholecystic duct was too close to separate, so the gallbladder and cholecystic duct were removed completely along with the tumor. Histopathological and immunohistochemical examinations of surgical specimens showed a schwannoma in the hepatoduodenal ligament. However, 1 mo later, the patient was readmitted to our hospital because of jaundice and diagnosed with obstruction of the common bile duct without a mass or stones in the duct. Fortunately, the patient was cured by implantation of a common bile duct stent under ERCP.
In conclusion, schwannoma in the hepatoduodenal ligament is rare. We have presented the fourth hepatoduodenal ligament schwannoma. It is a challenge to determine the location and obtain a precise diagnosis prior to surgery, although multiple imaging modalities are used. Following complete tumor excision, patients with benign schwannomas generally have good prognosis. Common bile duct stenosis after resection of schwannoma in the hepatoduodenal ligament has not been reported previously. We have presented the first case to be cured by implantation of a common bile duct stent under ERCP.
A 43-year-old man was referred to our hospital because of an abdominal mass found by physical examination.
The abdomen was soft, lax and nondistended without evidence of a palpable mass.
Abdominal sarcoma, abdominal neurogenic tumor, pancreatic cancer and cholangiocarcinoma.
Before surgery, laboratory results were normal.
Ultrasound (US) revealed an 8.3 cm × 5.2 cm, well-defined hypodense lesion between the pancreatic head and portal vein. No blood flow signal was found within the mass by Color Doppler US. An unenhanced computed tomography (CT) scan showed an 8.2 cm × 5.1 cm well-defined cystic and solid mass above the pancreatic head and adjacent to the common hepatic artery. The pancreaticoduodenal artery was compressed by the mass. On contrast-enhanced CT, the mass showed no obvious enhancement. Computed tomography angiography showed that the blood supply of the tumor was probably from branches of the pancreaticoduodenal artery. Magnetic resonance cholangiopancreatography showed that the mass was inhomogeneous and hyperintense on T2-weighted images and probably located in the pancreatic head, with compression of the middle-low segment of the common bile duct. According to imaging examinations, an abdominal mass was primarily considered.
Microscopically, the tumor had a capsule and was adjacent to the cholecystic duct (Figure 3A), and mainly consisted of spindle-shaped cells with no atypia, compatible with a benign schwannoma with both hypercellular and hypocellular areas. Immunohistochemical investigation showed that the tumor was positive for protein S-100, but negative for CD34, CD117 and smooth muscle actin. Finally, the tumor was diagnosed as a schwannoma in the hepatoduodenal ligament.
The patient underwent complete resection of the gallbladder and cholecystic duct along with the tumor in the hepatoduodenal ligament.
Schwannoma in the hepatoduodenal ligament is rare. To date, only four cases have been reported in the English literature, including our case presented in this report.
It is a challenge to determine the location and obtain a precise diagnosis prior to surgery, although multiple imaging modalities are used. Following complete tumor excision, patients with benign schwannomas generally have good prognosis. Common bile duct stenosis after resection of the schwannoma in hepatoduodenal ligament has not been reported and we present the first case to be cured by implantation of a common bile duct stent under endoscopic retrograde cholangiopancreatography.
This study highlights the diagnosis and treatment of a rare schwannoma in hepatoduodenal ligament and the authors also conducted a literature review so as to deepen the understanding of the subject. The information of this paper is valuable to the readers.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Armstrong N, Pavlovic M S- Editor: Qi Y L- Editor: A E- Editor: Zhang FF
| 1. | Le Guellec S. [Nerve sheath tumours]. Ann Pathol. 2015;35:54-70. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | J D, R S, K C, Devi NR. Pancreatic schwannoma - a rare case report. J Clin Diagn Res. 2014;8:FD15-FD16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Ariel IM. Tumors of the peripheral nervous system. CA Cancer J Clin. 1983;33:282-299. [PubMed] [Cited in This Article: ] |
| 4. | Pilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol. 2004;52:229-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 231] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 5. | Das Gupta TK, Brasfield RD. Tumors of peripheral nerve origin: benign and malignant solitary schwannomas. CA Cancer J Clin. 1970;20:228-233. [PubMed] [Cited in This Article: ] |
| 6. | Nagafuchi Y, Mitsuo H, Takeda S, Ohsato K, Tsuneyoshi M, Enjoji M. Benign schwannoma in the hepatoduodenal ligament: report of a case. Surg Today. 1993;23:68-72. [PubMed] [Cited in This Article: ] |
| 7. | Pinto J, Afonso M, Veloso R, Tente D, Fernandes S, Proença L, Carvalho J, Pontes JM, Fraga J. Benign schwannoma of the hepatoduodenal ligament. Endoscopy. 2011;43 Suppl 2 UCTN:E195-E196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Tao L, Xu S, Ren Z, Lu Y, Kong X, Weng X, Xie Z, Hu Z. Laparoscopic resection of benign schwannoma in the hepatoduodenal ligament: A case report and review of the literature. Oncol Lett. 2016;11:3349-3353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Das Gupta TK, Brasfield RD, Strong EW, Hajdu SI. Benign solitary Schwannomas (neurilemomas). Cancer. 1969;24:355-366. [PubMed] [Cited in This Article: ] |
| 10. | Abell MR, Hart WR, Olson JR. Tumors of the peripheral nervous system. Hum Pathol. 1970;1:503-551. [PubMed] [Cited in This Article: ] |
| 11. | Xu SY, Sun K, Xie HY, Zhou L, Zheng SS, Wang WL. Hemorrhagic, calcified, and ossified benign retroperitoneal schwannoma: First case report. Medicine (Baltimore). 2016;95:e4318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Tao K, Chang W, Zhao E, Deng R, Gao J, Cai K, Wang G, Zhang P. Clinicopathologic Features of Gastric Schwannoma: 8-Year Experience at a Single Institution in China. Medicine (Baltimore). 2015;94:e1970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Bayraktutan U, Kantarci M, Ozgokce M, Aydinli B, Atamanalp SS, Sipal S. Education and Imaging. Gastrointestinal: benign cystic schwannoma localized in the gastroduodenal ligament; a rare case. J Gastroenterol Hepatol. 2012;27:985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Tang SX, Sun YH, Zhou XR, Wang J. Bowel mesentery (meso-appendix) microcystic/reticular schwannoma: case report and literature review. World J Gastroenterol. 2014;20:1371-1376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 21] [Cited by in F6Publishing: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Liu LN, Xu HX, Zheng SG, Sun LP, Guo LH, Wu J. Solitary schwannoma of the gallbladder: a case report and literature review. World J Gastroenterol. 2014;20:6685-6690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Nishikawa T, Shimura K, Tsuyuguchi T, Kiyono S, Yokosuka O. Contrast-enhanced harmonic EUS of pancreatic schwannoma. Gastrointest Endosc. 2016;83:463-464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Xu SY, Guo H, Shen Y, Sun K, Xie HY, Zhou L, Zheng SS, Wang WL. Multiple schwannomas synchronously occurring in the porta hepatis, liver, and gallbladder: first case report. Medicine (Baltimore). 2016;95:e4378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Weiss SW, Langloss JM, Enzinger FM. Value of S-100 protein in the diagnosis of soft tissue tumors with particular reference to benign and malignant Schwann cell tumors. Lab Invest. 1983;49:299-308. [PubMed] [Cited in This Article: ] |
| 19. | Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM. Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics. 2003;23:29-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 283] [Cited by in F6Publishing: 313] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 20. | Li S, Ai SZ, Owens C, Kulesza P. Intrapancreatic schwannoma diagnosed by endoscopic ultrasound-guided fine-needle aspiration cytology. Diagn Cytopathol. 2009;37:132-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Kudo T, Kawakami H, Kuwatani M, Ehira N, Yamato H, Eto K, Kubota K, Asaka M. Three cases of retroperitoneal schwannoma diagnosed by EUS-FNA. World J Gastroenterol. 2011;17:3459-3464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |