Published online Feb 28, 2015. doi: 10.3748/wjg.v21.i8.2542
Peer-review started: July 5, 2014
First decision: July 21, 2014
Revised: August 4, 2014
Accepted: November 19, 2014
Article in press: November 19, 2014
Published online: February 28, 2015
We present a case of acute upper gastrointestinal haemorrhage in a patient with systemic vasculitis immunosuppressed on cyclophosphamide and prednisolone. The patient presented with a diffuse haemorrhagic oesophagitis and a non-specific duodenitis. Biopsies taken from the oesophagus and duodenum demonstrated infection with herpes simplex virus (HSV) and cytomegalovirus (CMV) respectively. Viral infection of the upper gastrointestinal tract is a recognised complication of immunosuppression and HSV is one of the most common pathogens. CMV on the other hand most commonly causes a colitis or less commonly oesophagitis. CMV enteritis is rare as is the synchronous infection with two viral agents in an immunocompromised patient having being described in a few case series only. Viral infection of the gastrointestinal tract in immunocompromised patients should be treated with systemic anti-viral medication and consideration to withdrawal of the immunosuppressive therapy if possible and appropriate. The authors highlight the need for a high suspicion of viral infection in immunosuppressed patients presenting with upper gastrointestinal bleeding.
Core tip: Viral infection of the gastrointestinal tract is a recognised complication of immunosuppression and in severe cases can lead to gastrointestinal haemorrhage. Although uncommon, synchronous infection with more than one viral agent is possible. Clinicians should have a low threshold for suspecting viral aetiology of mucosal inflammation and ulceration in immunosupressed patients and consider empirical antiviral therapy in immunosupressed patients.
- Citation: Smith LA, Gangopadhyay M, Gaya DR. Catastrophic gastrointestinal complication of systemic immunosuppression. World J Gastroenterol 2015; 21(8): 2542-2545
- URL: https://www.wjgnet.com/1007-9327/full/v21/i8/2542.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i8.2542
Viral infection of the gastrointestinal tract is a recognised complication of immunosuppression. Herpes simplex virus (HSV) infection usually causes small vesicles and superficial ulcers, however in the context of immunosuppression the ulcers can become necrotic and lead to a diffuse hemorrhagic oesophagitis as illustrated in this case[1]. Cytomegalovirus (CMV) most commonly causes a colitis and less commonly oesophagitis[2]. CMV enteritis is rare, as is dual infectivity in the upper gastrointestinal tract with both HSV and CMV, having been reported in a few case series only[3].
A 79-year-old lady presented to our institution with melaena and haematemesis. Six weeks earlier, with no significant past medical history, she had developed an acute kidney injury, peripheral oedema and evidence of nephrotic syndrome and underwent a renal biopsy which diagnosed myeloperoxidase anti-neutrophil cytoplasmic antibody positive vasculitis. She was commenced on cyclophosphamide 100 mg nocte and high dose, tapering oral corticosteroid (prednisolone 60 mg) with prophylactic co-trimoxazole. By the time of presentation with symptoms of upper gastrointestinal haemorrhage she had been on 6 wk of high dose corticosteroids (40 mg prednisolone) and remained on the same dose of cyclophosphamide. She had complained of mouth ulceration in the two weeks preceding this admission, which had been treated with topical bonjela and nystatin by the nephrologists with no specific diagnosis having been made. Haematology at that time demonstrated a normal total white blood cell count (7.6 × 109/L); normal neutrophil count (7.6 × 109/L) but a lymphocytopenia (0.2 × 109/L) was noted.
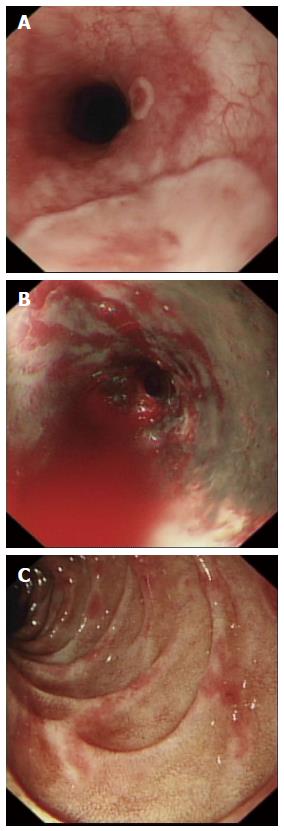
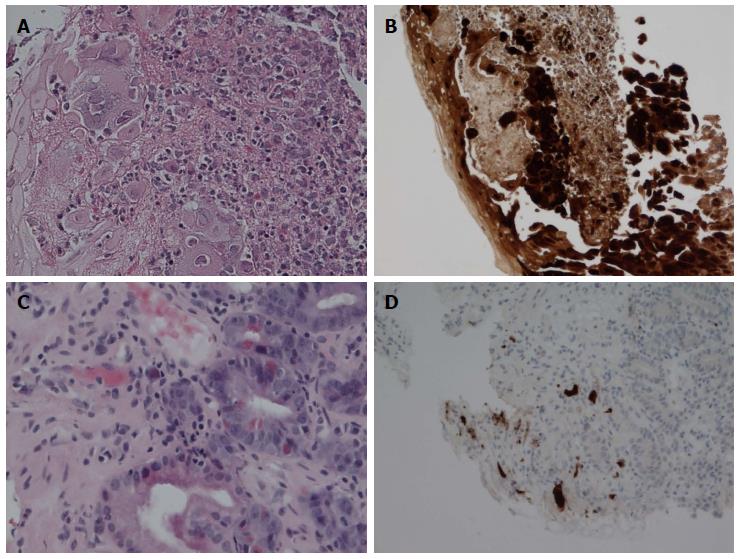
She was hemodynamically shocked on presentation with her upper gastrointestinal haemorrhage with ongoing evidence of peripheral edema. Initial hemoglobin was 106 g/L, with moderate thrombocytopenia and normal coagulation studies. She had evidence of acute on chronic kidney injury with a serum urea of 40.4 mmol/L and creatinine of 422 μmol/L. After appropriate resuscitation with both intravenous crystalloids and transfusion of 2 units of packed red cells she attended for an emergency upper gastrointestinal endoscopy. This showed discrete raised plaques in her upper oesophagus (Figure 1A) and diffuse bleeding from necrotic mucosa in the lower oesophagus (Figure 1B). The macroscopic appearances in the second part of the duodenum (Figure 1C) revealed a non-specific duodenitis. Biopsies were taken from both the upper oesophagus and duodenum. The lesions shown in Figure 1A are typical of HSV oesophagitis; confirmed with histological and immunohistochemical examination. Figure 2A shows the typical appearance of HSV esophagitis with ulcer, inflammatory debris and multinucleated squamous cells with ground glass intranuclear inclusions; positive with subsequent HSV immunostains (Figure 2B). The histology of the duodenal biopsies (Figure 2C) demonstrates large eosinophilic inclusion bodies of CMV; again confirmed on immunohistochemistry (Figure 2D). Serology showed CMV DNA PCR positivity (log 7.95 copies/mL). HSV serology was not confirmed. She had no previous virological results and thus it was unclear of these infections were reactivations or de novo infections. Cyclosphosphamide immunosuppression was stopped immediately after endoscopy, however steroids were continued and the dose increased due to risk of adrenal dependency. The patient continued to have worsening renal failure requiring haemodialysis and unfortunately died five days later of overwhelming sepsis despite treatment with intravenous aciclovir 10 mg/kg 8 hourly which was switched after 48 h to intravenous ganciclovir 1.25 mg/kg per day.
This case demonstrates the risk of serious infectious gastrointestinal complications of immunosuppression. A high suspicion for viral infection, particularly when gastrointestinal ulceration is present, and a low threshold for empirical anti-viral treatment are vital in this patient cohort. When the diagnosis is suspected at the time of endoscopy biopsies should be taken along with serum for virological testing. Consideration to stopping immunosuppression along with empiral anti-viral treatment whilst awaiting confirmation is advised.
A 79-year-old immunosuppressed patient presented with haematemesis and melaena.
The patient was noted to be haemodynamically compromised with evidence of peripheral oedema.
The patient was thought to have a significant upper gastrointestinal bleed, initially suspected to be secondary to peptic ulceration.
Laboratory findings showed a normocytic anaemia, lymphocytopenia and acute on chronic renal impairment.
After resuscitation the patient attended for an urgent upper gastrointestinal (GI) endoscopy which demonstrated a severe oesophagitis with active bleeding and plaques suggestive of viral aetiology and a non-specific appearing duodenitis.
Oesophageal biopsies demonstrated small fragments of oesophageal mucosal tissue with nuclear vacuolar changes typical of herpes viral infection whilst duodenal biopsies showed erosive and degenerative changes and were positive for cytomegalovirus (CMV) on immunostaining.
The patient was resuscitated with intravenous fluids, blood transfusion and was started on systemic anti-viral therapy with acyclovir and then ganciclovir; her immunosuppressant was withheld.
Dual viral infection in the upper GI tract has only rarely been described previously.
CMV and herpes simplex virus (HSV) are both from the herpesvirus family and are rare causes of upper GI ulceration and bleeding.
Clinicians need to consider viral infection as an aetiology of upper GI haemorrhage in immunosuppressed patients presenting with haematemesis and/or melana.
The authors have described a case of dual HSV and CMV infection in the upper GI tract of an immunosuppressed patient with renal vasculitis presenting as a GI bleed. The article highlights the need for empirical antiviral therapy in this setting and the need to consider the diagnosis in the first place.
P- Reviewer: Lorenzo-Zuniga V, Schuurman HJ, Wasano K, Yang CH S- Editor: Gou SX L- Editor: A E- Editor: Ma S
| 1. | Généreau T, Rozenberg F, Bouchaud O, Marche C, Lortholary O. Herpes esophagitis: a comprehensive review. Clin Microbiol Infect. 1997;3:397-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Baroco AL, Oldfield EC. Gastrointestinal cytomegalovirus disease in the immunocompromised patient. Curr Gastroenterol Rep. 2008;10:409-416. [PubMed] [Cited in This Article: ] |
| 3. | Vodovnik A, Cerar A. Synchronous herpes simplex virus and cytomegalovirus esophagitis. Z Gastroenterol. 2000;38:491-494. [PubMed] [Cited in This Article: ] |