Published online Aug 14, 2015. doi: 10.3748/wjg.v21.i30.9223
Peer-review started: February 10, 2015
First decision: March 10, 2015
Revised: April 7, 2015
Accepted: June 15, 2015
Article in press: June 16, 2015
Published online: August 14, 2015
A 91-year-old man was referred to our hospital with intermittent dysphagia. He had undergone esophagectomy for esophageal cancer (T3N2M0 Stage III) 11 years earlier. Endoscopic examination revealed an anastomotic stricture; signs of inflammation, including redness, erosion, edema, bleeding, friability, and exudate with white plaques; and multiple depressions in the residual esophagus. Radiographical examination revealed numerous fine, gastrografin-filled projections and an anastomotic stricture. Biopsy specimens from the area of the anastomotic stricture revealed inflammatory changes without signs of malignancy. Candida glabrata was detected with a culture test of the biopsy specimens. The stricture was diagnosed as a benign stricture that was caused by esophageal intramural pseudodiverticulosis. Accordingly, endoscopic balloon dilatation was performed and anti-fungal therapy was started in the hospital. Seven weeks later, endoscopic examination revealed improvement in the mucosal inflammation; only the pseudodiverticulosis remained. Consequently, the patient was discharged. At the latest follow-up, the patient was symptom-free and the pseudodiverticulosis remained in the residual esophagus without any signs of stricture or inflammation.
Core tip: Although esophageal intramural pseudodiverticulosis (EIPD) itself is a very rare disease, we encountered a case of EIPD occurring in the residual esophagus after esophagectomy. To our knowledge, no previous reports have described EIPD as a cause of benign stricture in esophagogastric anastomosis. The mucosal inflammation and stricture were treated with endoscopic balloon dilatation and anti-fungal therapy. Herein, we report the first case of EIPD showing anastomosis stricture 11 years after esophagectomy was performed to treat esophageal cancer.
- Citation: Takeshita N, Kanda N, Fukunaga T, Kimura M, Sugamoto Y, Tasaki K, Uesato M, Sazuka T, Maruyama T, Aida N, Tamachi T, Hosokawa T, Asai Y, Matsubara H. Esophageal intramural pseudodiverticulosis of the residual esophagus after esophagectomy for esophageal cancer. World J Gastroenterol 2015; 21(30): 9223-9227
- URL: https://www.wjgnet.com/1007-9327/full/v21/i30/9223.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i30.9223
Esophageal intramural pseudodiverticulosis (EIPD) was first described by Mendl et al[1] in 1960. It is a rare disease that is characterized by multiple small, flask-shaped outpouchings of the esophageal wall. To date, only approximately 200-300 cases of EIPD have been reported worldwide[2,3]. The predominant symptom is dysphagia, which is often accompanied by an esophageal stricture. However, to the best of our knowledge, there has been no previous report on EIPD developing in the residual esophagus after esophagectomy. We report the first case of EIPD with an anastomosis stricture that was observed 11 years after esophagectomy, which had been performed to treat esophageal cancer.
A 91-year-old man was referred to our hospital because of intermittent dysphagia. He had undergone esophagectomy with gastric tube reconstruction and intrathoracic anastomosis for esophageal cancer (T3N2M0 Stage III; using the seventh edition of the Union for International Cancer Control TNM classification system) 11 years earlier. No recurrence had been observed. Other than the previous esophageal cancer and hypertension, his medical history was unremarkable. He had been a heavy, regular drinker for several years. Physical examination showed a chronic, ill-looking overall appearance. Laboratory data showed anemia (hemoglobin: 9.3 g/dL) and renal dysfunction (serum creatinine: 1.69 mg/dL).
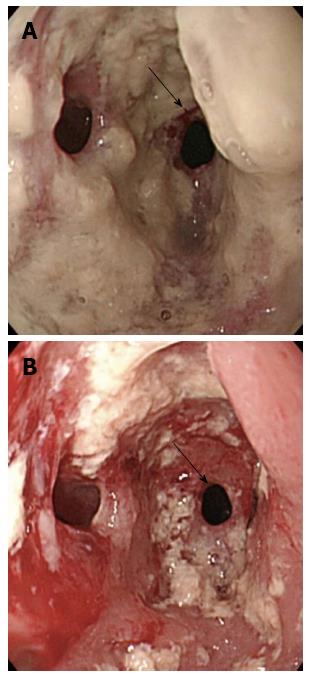
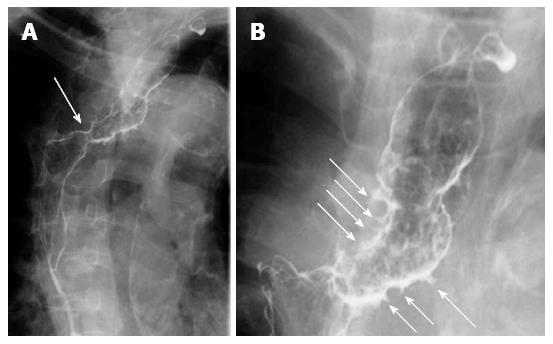
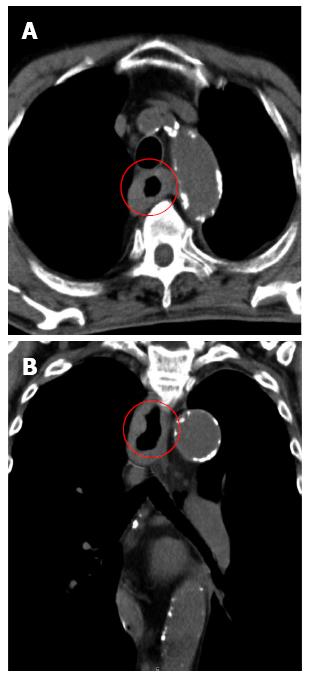
Endoscopy of the upper gastrointestinal tract was performed, which revealed an anastomotic stricture, and the mucosa in the residual esophagus exhibited chronic inflammation, showing redness, erosion, edema, bleeding, friability, and exudate with numerous white plaques. After washing the exudate with plaques, multiple depressions were found, and the endoscope could not pass the anastomosis (Figure 1). Radiographical examination revealed numerous fine, gastrografin-filled projections and an anastomotic stricture (Figure 2). Computed tomography was used to show the thickness of the wall of the residual esophagus, and no metastatic lesions were observed (Figure 3). Biopsy specimens from the area of the anastomotic stricture revealed only inflammatory changes without any signs of malignancy. Candida glabrata was detected with a culture test of the biopsy specimens. Based on these findings, the stricture was diagnosed as a benign stricture caused by EIPD instead of esophageal cancer recurrence; accordingly, endoscopic balloon dilatation was performed and oral anti-fungal therapy (amphotericin B) was started in the hospital.
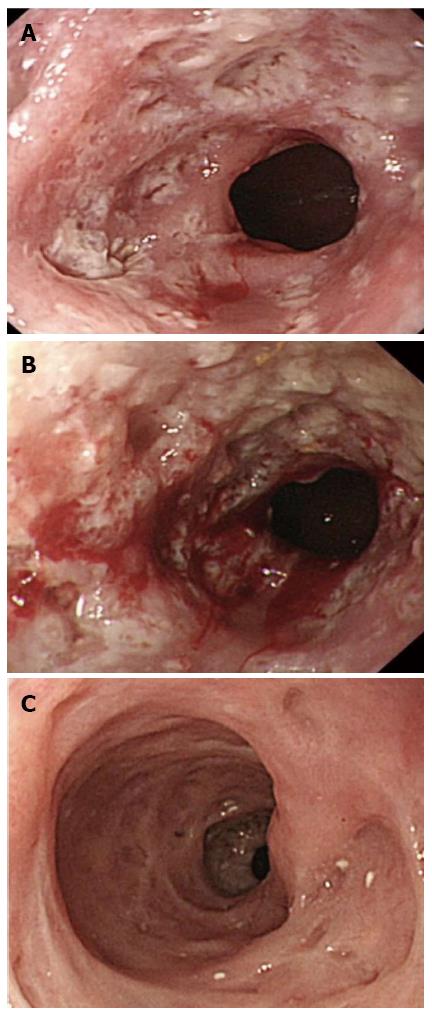
Two weeks later, endoscopic examination showed that the dilated anastomosis remained and the mucosal inflammation was partially improved (Figure 4A). As the symptoms had dramatically improved, the patient was discharged. However, 3 wk after discharge, even though endoscopic examination showed that the dilated anastomosis still remained, the mucosal inflammation had worsened (Figure 4B). Accordingly, the patient was readmitted and started on micafungin treatment by intravenous administration. Two weeks after readmission, endoscopic examination revealed improvement of the mucosal inflammation. Only tiny orifices, corresponding to pseudodiverticulosis, remained (Figure 4C). Consequently, the patient was discharged. At the latest follow-up, the patient was symptom-free and pseudodiverticulosis remained in the residual esophagus without signs of stricture or inflammation.
EIPD is related to the submucosal esophageal glands, involving cystic dilation of the excretory ducts; as a result, it is not true diverticulosis. The etiology and pathogenesis of EIPD need to be further clarified, but they are thought to involve obstruction of the esophageal mucous glands by chronic inflammation or submucosal fibrosis[4]. EIPD has been reported to be associated with various risk factors, including diabetes mellitus, esophageal candidiasis, alcohol consumption, gastroesophageal reflux disease, and cancer[4-6].
The main clinical symptom of EIPD is intermittent dysphagia, which is often accompanied by esophageal stricture. The possibility of severe complications, such as esophageal perforation, has also been reported[7]. Radiographically, EIPD is characterized by multiple, small, flask-shaped outpouchings in the wall of the esophagus. The upper gastrointestinal endoscopic findings show the presence of many tiny pseudodiverticular openings with white plaques.
Benign anastomotic strictures after esophagectomy are reportedly observed within a median of 5 mo after esophagectomy (mean, 7 mo; range: 8 d to 36 mo) and are preferably treated by endoscopic balloon dilatation. In one study, the overall clinical success rate was 99% in patients undergoing single or multiple balloon dilatations[8]. For EIPD, when esophageal candidiasis or reflux esophagitis is present, medical treatment alone is often sufficient to relieve the symptoms and reduce EIPD[9]. However, when there is a stricture, endoscopic dilatation should be considered. Treatment of a stricture with endoscopic dilatation is effective for resolving dysphagia, but repeated dilatation may be necessary[5].
In our case, the cause of the stricture was thought to be inflammation from EIPD, and the patient’s EIPD itself did not improve with the combination of dilatation and oral anti-fungal therapy. Although the anastomotic stricture and dysphagia initially improved, the remaining endoscopic findings, including redness, erosion, edema, bleeding, friability, and exudate with numerous white plaques, were considered to be risk factors for recurrence. Upon recurrence, we restarted the anti-fungal therapy by intravenous administration until these endoscopic inflammatory findings improved. In other words, we observed worsening of the mucosal inflammation and recognized the necessity of criteria regarding the therapeutic period and effects. As in many of the reported cases[10], the pseudodiverticulosis itself did not disappear in the present case. To prevent the recurrence of EIPD and severe complications, such as esophageal perforation, it is important to control the background esophageal inflammation. Therefore, it is necessary to perform regular follow-ups of both the symptoms and endoscopic findings of the esophageal mucosa.
Although the presence of cancer has been reported as a potential risk factor for EIPD, in the present case, the patient’s esophageal cancer had been cured 11 years before EIPD was observed. As a result, we speculate that the main cause of EIPD in this case was esophageal candidiasis, although alcohol consumption, malnutrition, and susceptibility to infection due to advanced age may also have played roles. However, if possible, any modifiable risk factors should be removed.
In conclusion, we described an extremely rare case of EIPD of the residual esophagus after esophagectomy. EIPD itself is a very rare disease, and we have now reported the first case of EIPD occurring in the residual esophagus after esophagectomy. Furthermore, to our knowledge, no previous reports have described EIPD as a cause of benign stricture in an esophagogastric anastomosis.
A 91-year-old man was referred to the hospital because of intermittent dysphagia after having undergone esophagectomy to treat esophageal cancer 11 years earlier.
Esophageal intramural pseudodiverticulosis of the residual esophagus.
Recurrence of esophageal cancer.
Endoscopy revealed an anastomotic stricture and multiple diverticula. Radiological examination revealed numerous fine, gastrografin-filled projections and an anastomotic stricture.
Biopsy specimens of the mucosa taken from the area of the stricture showed desquamative squamous epithelium without evidence of neoplasm. Candida glabrata was revealed with a culture test of the biopsy specimens.
Anti-fungal therapy was administered and endoscopic dilatation was performed.
No previous reports have described esophageal intramural pseudodiverticulosis (EIPD) as a cause of benign stricture found in an esophagogastric anastomosis. This is the first reported case of EIPD showing an anastomosis stricture 11 years after esophagectomy was performed to treat esophageal cancer.
EIPD is a rare disease that is characterized by multiple small, flask-shaped outpouchings of the esophageal wall. To date, only approximately 200-300 cases of EIPD have been reported worldwide.
This case report describes a rare case of EIPD found in the residual esophagus after esophagectomy. To prevent recurrence of EIPD and severe complications, it is important to control the background esophageal inflammation. Hence, it is necessary to perform regular follow-ups to evaluate both the symptoms and endoscopic findings of the esophageal mucosa.
This is the first reported case of EIPD showing anastomosis stricture 11 years after esophagectomy was performed to treat esophageal cancer.
P- Reviewer: Bonavina L, Hoff dal, Lorenzo-Zuniga V S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
| 1. | Mendl K, McKay JM, Tanner CH. Intramural diverticulosis of the oesophagus and Rokitansky-Aschoff sinuses in the gall-bladder. Br J Radiol. 1960;33:496-501. [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 88] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hahne M, Schilling D, Arnold JC, Riemann JF. Esophageal intramural pseudodiverticulosis: review of symptoms including upper gastrointestinal bleeding. J Clin Gastroenterol. 2001;33:378-382. [PubMed] [Cited in This Article: ] |
| 3. | Ose T, Okita K, Takahashi Y, Moriyama I, Kazumori H, Ishihara S, Amano Y, Adachi K, Kinoshita Y. Esophageal intramural pseudodiverticulosis improved by endoscopic dilatation. Esophagus. 2006;3:71-74. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Chon YE, Hwang S, Jung KS, Lee HJ, Lee SG, Shin SK, Lee YC. A case of esophageal intramural pseudodiverticulosis. Gut Liver. 2011;5:93-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Halm U, Lamberts R, Knigge I, Mössner J, Zachäus M. Esophageal intramural pseudodiverticulosis: endoscopic diagnosis and therapy. Dis Esophagus. 2014;27:230-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Plavsic BM, Chen MY, Gelfand DW, Drnovsek VH, Williams JP, Kogutt MS, Terry JA, Plenkovich D. Intramural pseudodiverticulosis of the esophagus detected on barium esophagograms: increased prevalence in patients with esophageal carcinoma. AJR Am J Roentgenol. 1995;165:1381-1385. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Murakami M, Tsuchiya K, Ichikawa H, Kawaguchi K, Sugiyama A, Ishida K, Chisuwa H, Kawasaki S. Esophageal intramural pseudodiverticulosis associated with esophageal perforation. J Gastroenterol. 2000;35:702-705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Park JY, Song HY, Kim JH, Park JH, Na HK, Kim YH, Park SI. Benign anastomotic strictures after esophagectomy: long-term effectiveness of balloon dilation and factors affecting recurrence in 155 patients. AJR Am J Roentgenol. 2012;198:1208-1213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Bender MD, Haddad JK. Disappearance of multiple esophageal diverticula following treatment of esophagitis: serial endoscopic, manometric, and radiologic observations. Gastrointest Endosc. 1973;20:19-22. [PubMed] [Cited in This Article: ] |
| 10. | Chiba T, Iijima K, Koike T, Uno K, Asano N, Shimosegawa T. A case of severe esophageal intramural pseudodiverticulosis whose symptoms were ameliorated by oral administration of anti-fungal medicine. Case Rep Gastroenterol. 2012;6:103-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |