Published online Apr 28, 2015. doi: 10.3748/wjg.v21.i16.4969
Peer-review started: October 28, 2014
First decision: December 11, 2014
Revised: January 9, 2015
Accepted: February 11, 2015
Article in press: February 11, 2015
Published online: April 28, 2015
AIM: To assess laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions.
METHODS: From March 2010 to June 2014, 30 patients (14 men and 16 women, aged 36-78 years, mean age 59.8 years) underwent laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through anus-preserving transanal resection. The tumors were 5-7 cm away from the anal margin in 24 cases, and 4 cm in six cases. In preoperative assessment, there were 21 cases of T1N0M0 and nine of T2N0M0. Through the middle approach, the sigmoid mesentery was freed at the root with an ultrasonic scalpel and the roots of the inferior mesenteric artery and vein were dissected, clamped and cut. Following the total mesorectal excision principle, the rectum was separated until the anorectal ring reached 3-5 cm from the distal end of the tumor. For perineal surgery, a ring incision was made 2 cm above the dentate line, and sharp dissection was performed submucosally towards the superior direction, until the plane of the levator ani muscle, to transect the rectum. The rectum and distal sigmoid colon were removed together from the anus, followed by a telescopic anastomosis between the full thickness of the proximal colon and the mucosa and submucosal tissue of the rectum.
RESULTS: For the present cohort of 30 cases, the mean operative time was 178 min, with an average of 13 positive lymph nodes detected. One case of postoperative anastomotic leak was observed, requiring temporary colostomy, which was closed and recovered 3 mo later. The postoperative pathology showed T1-T2N0M0 in 19 cases and T2N1M0 in 11 cases. Twelve months after surgery, 94.4% patients achieved anal function Kirwan grade 1, indicating that their anal function returned to normal. The patients were followed up for 1-36 mo, with an average of 23 mo. There was no local recurrence, and 17 patients survived for > 3 years (with a survival rate of 100%).
CONCLUSION: Laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions is safe and feasible.
Core tip: This study assesses the laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions. Thirty cases of lower rectal cancer have been treated using this procedure with satisfactory outcomes in follow-up observation. We concluded that laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions is safe and feasible.
- Citation: Li SY, Chen G, Du JF, Chen G, Wei XJ, Cui W, Zuo FY, Yu B, Dong X, Ji XQ, Yuan Q. Laparoscopic resection of lower rectal cancer with telescopic anastomosis without abdominal incisions. World J Gastroenterol 2015; 21(16): 4969-4974
- URL: https://www.wjgnet.com/1007-9327/full/v21/i16/4969.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i16.4969
Procedures for anus-preserving radical resection for lower rectal cancer are of current research interest[1-5]. In recent years, laparoscopic radical surgery of rectal cancer has been widely carried out[6-8], but it generally requires an assisting abdominal incision for removal of tumor specimens, which prevents it from being completely minimally invasive[9-11]. We have completed 420 cases of telescopic anastomosis for anal preservation in radical resection of lower rectal cancer[3]. We first reported laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions in 2011[12,13], which is an abdominal incision-free and scar-free completely minimally invasive technique. So far, 30 cases of lower rectal cancer have been treated using this procedure with satisfactory outcomes in follow-up observation.
Thirty patients, including 14 men and 16 women, were recruited. The ages ranged from 36 to 78 years (mean: 59.8 years). The tumors were 5-7 cm away from the anal margin in 24 cases, and 4 cm in six cases. They were all confirmed as high-grade rectal adenocarcinoma by preoperative pathology. The diagnoses were confirmed by colonoscopy biopsies in all cases. Barium enema, digital rectal examination, and rectal endoscopy were used to determine the distance between the lower tumor edge and the anal margin. Pelvic and liver magnetic resonance imaging or computed tomography (CT) examination, as well as transrectal ultrasonography, was carried out to assess the depth of tumor invasion, presence of liver metastasis and lymph node enlargement. Preoperative assessment was T1N0M0 in 21 cases and T2N0M0 in nine.
Inclusion criteria were: (1) lower rectal cancer with the lower edge 5-7 cm from the anal margin; (2) T1/T2N0M0 highly differentiated small adenocarcinomas; (3) early rectal cancer confined to the bowel wall, tumor diameter ≤ 3 cm, invasion less than or equal to half the circle of the intestinal wall; and (4) tubular adenomas, which are villous tubular and glandular cancerous tumors for which the resection margin is > 1 cm; highly differentiated adenocarcinomas with resection of the lower edge > 2 cm; and poorly differentiated adenocarcinomas with resection of the lower edge > 3 cm.
Exclusion criteria were: (1) the lower edge of tumor < 5 cm from the anal margin; (2) the preoperative stage of tumor > T1/T2N0M0; (3) tumor diameter > 3 cm or invasion more than half the circle of the intestinal wall; and (4) overweight patient with BMI > 30 or with narrow pelvis.
Abdominal surgical procedures: After successful anesthesia, the patient was placed in a bladder lithotomy position. Following the four-port trocar operation, the umbilical camera system was placed in the observation port, and the working port was created at the right lower quadrant. A trocar was placed at each incision of the right middle and left lower quadrants of the abdomen. With the patient’s head facing down, the surgical field was revealed. Through the middle approach, the sigmoid mesentery was freed at the root with an ultrasonic scalpel, the adipose tissue and lymph nodes around the roots of the inferior mesenteric artery and vein were dissected, and the vascular root was clamped and cut. Bilateral ureteral tracts were protected. Following the total mesorectal excision (TME) principle, the rectum was dissected along the connective tissue between the visceral and parietal layers of the presacral space posterior to the rectum, to the anorectal ring and 3-5 cm from the distal end of the tumor. Caution was exercised to protect the pelvic autonomic nerve plexus. The cutting margin was 10 cm superior to the tumor. The corresponding mesentery was dissected using an ultrasonic scalpel. After completion of the perineal surgery, a large amount of warm distilled water was used to rinse the surgical field and a port was made to the right lower abdomen for placement of pelvic tube drainage. The trocars were removed and all ports closed. As a result, no auxiliary abdominal incision was made, leaving only four 0.5-1.0-cm small holes.
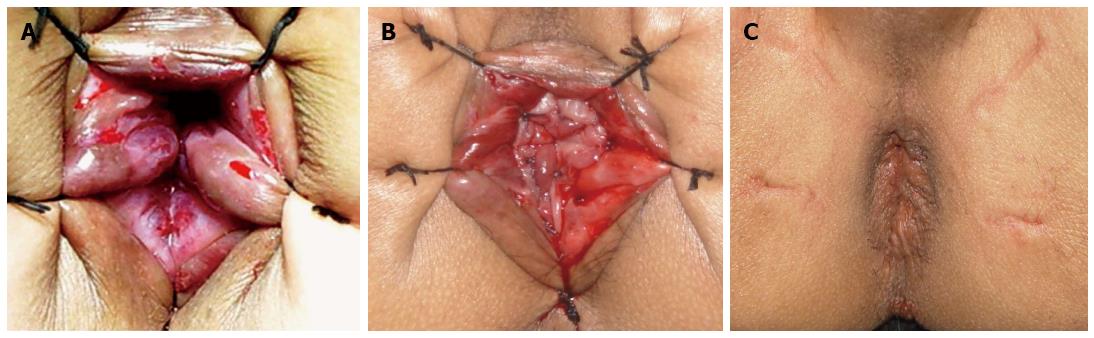
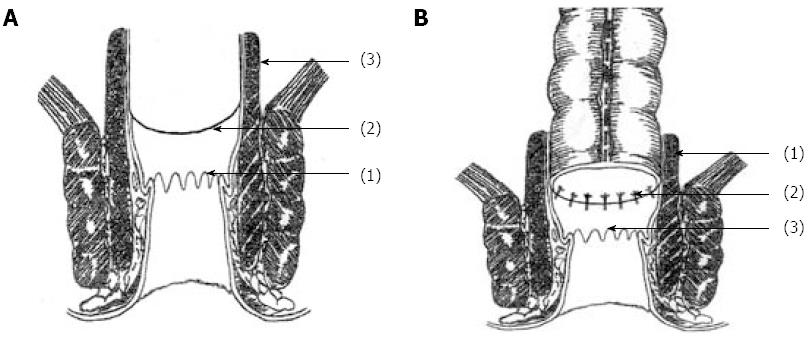
Anal operation: After extraepidural administration to fully relax the anal sphincter, the anus was dilated up to 4-6 fingers. Using the five-stitch suspension method[3,14] to reveal the field of the anal canal above the dentate line (Figure 1A), the anorectal tract was exposed using a double-leaf anal retractor. After submucosal circular injection of 1:10000 adrenaline saline 1.0 cm above the dentate line, to significantly elevate the submucosal tissue, an electric knife was used to cut open the mucosa 1.5-2.0 cm above the dentate line. Sharp dissection was performed along the rectal mucosa, upwards, to peel off the rectal mucosa for 2-4 cm, to reach the levator ani muscles, and the rectum was cut circularly[3]. The rectal tumor and distal sigmoid colon were removed from the anus together, and the sigmoid colon was cut proximally about 10 cm from the tumor, and the proximal colon was dragged out of the anus through the rectum. The distal rectal margin was sent for frozen section examination. The intact rectal muscular sheath of 2-4 cm was preserved about 2 cm above the dentate line, as well as the entire internal and external anal sphincter (Figure 2A). The distal colon was pulled out of the anus through the rectal muscular sheath, and at 2.0 cm above the dentate line set between the distal colon and rectal muscle sheath and fixed using the four-pin fixation method, and sutured intermittently at 12, 3, 6 and 9 points, respectively[5], to reduce tension and fix the connection. The full thickness of the proximal colon and the rectal and intestinal mucosa above the dentate line were connected using absorbable sutures with 8-12 stitches (Figure 1B and Figure 2B). After confirmation that the anastomosis had a satisfactory blood supply in a tension-free state, a piece of Vaseline gauze was inserted into the anal canal for support. The suspension sutures were removed, and the anastomotic portion was gently returned into the anus to complete the anastomosis between the full-thickness colon and rectal mucosa and submucosa (Figure 1C). The perineum was then covered with sterile dressing. Double-lumen presacral drainage was placed as routine, penetrating the anal skin, fixed on the skin, and connected with suction or a sterile bag, which was usually removed after 2-5 d.
According to the 2011 National Comprehensive Cancer Network guidelines for postoperative monitoring and follow-up, a medical history was taken and a physical examination was conducted once every 3 mo for 2 years, then once every 6 mo for 3 years, and once every 12 mo afterwards. Carcinoembryonic antigen assessment was carried out for tumors at T2 or above once every 3-6 mo after surgery for 2 years, and once every 6 mo until 5 years after surgery. Colonoscopy or proctoscopy of the anastomoses was performed once every 6 mo for 5 years for early detection of local recurrence. At the first 2-5 years after surgery, patients at Stages II or III received thoracic, abdominal, and pelvic CT scans each year for early detection of lung and liver metastases. The endpoint of follow-up was death or the end of the study.
A postoperative questionnaire survey was conducted for the Kirwan anal function assessment.
Surgery was completed successfully in all 30 patients, with an average length of operation of 178 min, including about 127 min for abdominal surgery and about 51 min for anal anastomosis. Mean intraoperative blood loss was 76 mL, and 13 positive lymph nodes were detected on average. Postoperative bowel movement occurred 3 d after surgery. There were no postoperative complications related to the surgery. The patients were discharged 12 d after surgery on average. The postoperative pathology showed T1-T2N0M0 in 19 cases and T2N1M0 in 11. In the present study, no patient received preoperative radiotherapy, and patients with greater than T2 stage received 7-12 cycles of postoperative systemic chemotherapy with the mFOLFOX6 protocol (oxaliplatin, 5-fluorouracil and calcium folinate). Eleven patients with T2N1M0 stage were given postoperative pelvic radiotherapy at a total dosage of 10-20 Gy before adjuvant chemotherapy. No abdominal incision was made, thereby achieving completely minimally invasive scar-free cosmetic outcomes. All of the 30 patients underwent a radical resection without positive circumferential resection of the margin and without positive distal resection margin (resection of the lower edge > 2 cm). The patients were followed up for 1-36 mo, with a mean of 23 mo. Early after surgery, defecation was 2-6 times/d, and the patients received two compound diphenoxylate tablets orally daily. Twelve months after surgery, 91.3% (21/23) of patients achieved anal function Kirwan grade 1, indicating that their anal function returned to normal. No patient received intraoperative diverting stoma, and one case of postoperative anastomotic leak was observed, requiring temporary colostomy, which was closed and recovered 3 mo later. No anastomotic stenosis or local tumor recurrence occurred. The quality of life was good for all patients, and 17 of them survived for > 3 years (with a survival rate of 100%). The patient data are shown in Table 1.
| No. of patients (n = 30) | |
| Age (yr) | 36-78 (mean 59.8) |
| Sex | |
| Male | 14 |
| Female | 16 |
| Distance from lower tumor edge to anal margin (cm) | |
| 5-7 | 24 |
| 4 | 6 |
| Preoperative tumor stage (n) | |
| I | 28 |
| II | 2 |
| III | 0 |
| IV | 0 |
| Postoperative tumor stage (n) | |
| I | 19 |
| II | 0 |
| III | 11 |
| IV | 0 |
| Postoperative diagnosis of rectal cancer (n) | |
| Intermediately to highly differentiated | 18 |
| Intermediately differentiated | 8 |
| Poorly differentiated | 2 |
| Adenoma | 2 |
| Preventive colostomy (n) | |
| No preventive colostomy | 29 |
| Preventive colostomy | 1 |
| Operative time (min) | 178 (range: 150-210) |
| Blood loss (mL) | 60 (range: 30-300) |
| Hospital stay (d) | 12 (range: 7-21) |
Kirwan classification[15] includes the following five grades: 1: normal; 2: occasionally needs an enema, with gas incontinence; 3: needs drug control, daily enema, needs to wear panty liner with a small amount of leakage or occasionally mild leakage of excrement; 4: underwear is often contaminated; and 5: requires colostomy. In this cohort, 6-9 bowel movements per day were observed after early intake after surgery. After administration of two compound diphenoxylate tablets orally 3 times daily for 2-3 d, the defecation was controlled at 3-6 times daily. Self-control bowel movements were significantly improved 2-3 mo after surgery. Twelve months after surgery, 91.3% (21/23) patients achieved anal function Kirwan grade 1, indicating that their anal function returned to normal (Table 2).
| Time | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | Total |
| 6 mo after surgery | 17 (65.4) | 8 (30.8) | 1 (3.8) | 0 | 0 | 26 |
| 12 mo after surgery | 21 (91.3) | 2 (8.7) | 0 | 0 | 0 | 23 |
Laparoscopic anus-preserving radical resection of rectal cancer has been widely carried out in recent years[16,17], but an abdominal incision is always required to remove the specimens, regardless of transumbilical single-port or assisted laparoscopic surgery[18,19], undoubtedly making it difficult to achieve the optimal goal of completely minimally invasive, incision-free, scar-free surgery. Based on the experience of open telescopic anastomosis for anal preservation in radical resection of lower rectal cancer[3,14], we have established laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, which enables incision-free, scar-free, cosmetic and minimally invasive treatment[12,13]. This innovative surgery is a major innovation for rectal cancer surgery, which has not been reported previously.
Telescopic anastomosis for anal preservation in radical resection of lower rectal cancer[12] preserves the anus and bowel movement control for most patients with lower or ultralow rectal cancer. The innovations of this surgery include the following: (1) the critical technique in the telescopic anastomosis is the four-stitch suture between the full-thickness colon and the residual rectal muscle sheath, which plays a role in reducing tension and reinforcing the fixation. This is the key to preventing the occurrence of anastomotic leakage, effectively reducing the incidence of anastomotic complications; (2) the anorectal ring and the entire internal and external sphincters are retained intact, so bowel control is preserved at 3-6 mo after surgery, improving postoperative physiological and quality of life; (3) under laparoscopy, sigmoid and rectal dissection is completed with an ultrasonic scalpel to 3-5 cm from the distal end of the tumor. The specimen is removed through and from the anus, which enables incision-free, scar-free, cosmetic and minimally invasive treatment; and (4) due to the minimal invasiveness, patients experience less postoperative pain, and can achieve earlier ambulation and faster recovery. Laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, is safe and feasible, which achieves the goal of minimally invasive and function-preserving surgery. This technique may be used for anus-preserving laparoscopic surgical treatment of lower rectal cancer.
Laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, includes the following features: (1) when using the scalpel to dissect the lymph nodes and fat tissue at the root of the mesenteric vessels, caution should be taken to avoid damage to the autonomic nervous bundle; (2) when dividing the inferior mesenteric artery and vein, attention should be paid to retain the mesenteric vascular bow, and ensure an adequate blood supply and length of the distal bowel segments, so that the anastomosis can be connected after the tumor is removed from the anus; (3) according to TME principles, the rectum should be dissected along the connective tissue between the visceral and parietal layers of the presacral space, posterior to the rectum, to the anorectal ring and 3-5 cm from the distal end of the tumor, to ensure complete tumor resection and lymph node dissection; (4) perineal surgery should be performed under adequate anesthesia[3,12], so that the anal sphincter achieves complete relaxation. For this, we use the five-stitch suspension method, which fully exposes the field above the dentate line, conducive to the surgical procedure. However, the suspension suture must only be closed when the sphincter is completely relaxed, to avoid damage to the anal skin and structure, thus affecting postoperative recovery of bowel function[12]; (5) to remove the mucosa completely while avoiding damage to internal and external sphincters, scissors can be used for sharp dissection along the superficial surface of the internal sphincter, otherwise it will damage the sphincter; (6) to ensure no fat residue along the colonic anastomosis, but a good blood supply, the colon ends should be trimmed to 0.5 cm, so that there is no residual fat tissue, which is conducive to anastomotic healing; (7) the telescopic full-thickness colon should be connected and fixed with the residual rectal sheath using interrupted four-stitch sutures[5], for reinforcement and reduced tension, which is the key to prevention of anastomotic fistula; and (8) the telescopic anastomosis should be closed with 8-12 stitches without too dense sutures in case of anastomotic stenosis.
Laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, is indicated for the same conditions as open telescopic anastomosis[3,13]. The TME principles should be strictly followed in the selection of personalized anus-preserving surgery according to the specific circumstances of the patient.
The lack of a control group is the main limitation of this study. More cases and longer follow-up will be included for the observation of oncological outcome, and we will carry out randomized controlled trials in future studies.
In conclusion, laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, is safe and feasible, which enables incision-free, scar-free, cosmetic and minimally invasive treatment. This technique may become an option for anus-preserving laparoscopic surgical treatment of low colorectal cancer.
Procedures for anus-preserving radical resection for lower rectal cancer are of current research interest. Although laparoscopic radical surgery of rectal cancer has been widely carried out recently, it generally requires an assisting abdominal incision for removal of tumor specimens, which prevents it from being completely minimally invasive.
The authors have completed 420 cases of telescopic anastomosis for anal preservation in radical resection of lower rectal cancer. They first reported laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions, which is an abdominal incision-free and scar-free completely minimally invasive technique, in 2011. So far, they have treated 30 cases of lower rectal cancer using this procedure with satisfactory outcomes in follow-up observation.
This study assesses the laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions. Thirty cases of lower rectal cancer have been treated using this procedure with satisfactory outcomes in follow-up observation. The authors concluded that laparoscopic radical resection of lower rectal cancer with telescopic anastomosis through transanal resection without abdominal incisions is safe and feasible.
Laparoscopic radical resection of lower rectal cancer with telescopic anastomosis, through transanal resection without abdominal incisions, is safe and feasible, which enables incision-free, scar-free, cosmetic and minimally invasive treatment. This technique may become an option for anus-preserving laparoscopic surgical treatment of low colorectal cancer.
Telescopic anastomosis for anal preservation in radical resection of lower rectal cancer preserves the anus and bowel movement control for most patients with lower or ultralow rectal cancer.
This is an interesting study regarding incision free laparoscopic rectal resection for rectal cancer.
P- Reviewer: Liu H, Nedrebo BS, Suzuki S, Zuo XL S- Editor: Ma YJ L- Editor: O’Neill M E- Editor: Wang CH
| 1. | Chin CC, Huang WS, Yeh CH, Wang JY. Performing handsewn coloanal anastomosis with the pursestring suture anoscope. Dis Colon Rectum. 2008;51:1430-1431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Kishimoto Y, Araki Y, Sato Y, Ogata Y, Shirouzu K. Functional outcome after sphincter excision for ultralow rectal cancer. Int Surg. 2007;92:46-53. [PubMed] [Cited in This Article: ] |
| 3. | Li SY, Chen G, Bai X, Zuo FY, Chen G, Du JF, Wei XJ, Cui W. Anus-preserving rectectomy via telescopic colorectal mucosal anastomosis for low rectal cancer: experience from a Chinese cohort. World J Gastroenterol. 2013;19:3841-3846. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Zhuang CP, Cai GY, Li TH, Wang YQ, Chen WR. [Efficacy evaluation of intersphincteric resection during anus-preserving operation for ultralow rectal carcinoma]. Zhonghua Wei Chang Wai Ke Zazhi. 2009;12:364-367. [PubMed] [Cited in This Article: ] |
| 5. | Tai JD, Liu YS, Wang GY. [Risk factors and the management of anastomotic leakage after anus-preserving operation for rectal cancer]. Zhonghua Wei Chang Wai Ke Zazhi. 2007;10:153-156. [PubMed] [Cited in This Article: ] |
| 6. | Hisada M, Katsumata K, Ishizaki T, Enomoto M, Matsudo T, Kasuya K, Tsuchida A. Complete laparoscopic resection of the rectum using natural orifice specimen extraction. World J Gastroenterol. 2014;20:16707-16713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 7. | Krane MK, Fichera A. Laparoscopic rectal cancer surgery: where do we stand? World J Gastroenterol. 2012;18:6747-6755. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Qu H, Du YF, Li MZ, Zhang YD, Shen J. Laparoscopy-assisted posterior low anterior resection of rectal cancer. BMC Gastroenterol. 2014;14:158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Bianchi PP, Rosati R, Bona S, Rottoli M, Elmore U, Ceriani C, Malesci A, Montorsi M. Laparoscopic surgery in rectal cancer: a prospective analysis of patient survival and outcomes. Dis Colon Rectum. 2007;50:2047-2053. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Maglio R, Meucci M, Muzi MG, Maglio M, Masoni L. Laparoscopic total mesorectal excision for ultralow rectal cancer with transanal intersphincteric dissection as a first step: a single-surgeon experience. Am Surg. 2014;80:26-30. [PubMed] [Cited in This Article: ] |
| 11. | Orsenigo E, Di Palo S, Vignali A, Staudacher C. Laparoscopic intersphincteric resection for low rectal cancer. Surg Oncol. 2007;16 Suppl 1:S117-S120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Li S, Chen G, Chen G. Transanal telescopic anastomosis after laparoscopicanterior resection of low rectal cancer: Report of one case. Zhonghua Puwaike Shoushuxue Zazhi (Electronic Version). 2011;151-155. [Cited in This Article: ] |
| 13. | Li SY, Chen G, Chen G, Zuo FY, Wei XJ, Yuan Q, DU JF. [Clinical study of laparoscopic sphincter-preserving proctectomy for low rectal cancer using transanal telescopic anastomosis]. Zhonghua Wei Chang Wai Ke Zazhi. 2011;14:532-534. [PubMed] [Cited in This Article: ] |
| 14. | Li SY, Liang ZJ, Yuan SJ, Yu B, Chen G, Zuo FY, Bai X, Chen G, Wei XJ, Xu YS. [Clinical experience of 371 cases of sphincter-preservation with telescopic anastomosis after radical excision for low-middle rectal cancer]. Zhonghua Wei Chang Wai Ke Zazhi. 2010;13:263-265. [PubMed] [Cited in This Article: ] |
| 15. | Kirwan WO, Turnbull RB, Fazio VW, Weakley FL. Pullthrough operation with delayed anastomosis for rectal cancer. Br J Surg. 1978;65:695-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 114] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Rajput A, Bullard Dunn K. Surgical management of rectal cancer. Semin Oncol. 2007;34:241-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Velez PM. Laparoscopic colonic and rectal resection. Baillieres Clin Gastroenterol. 1993;7:867-878. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 18. | Qiu XF, Lin L, Yuan SB, Yan F, Ding ZJ, Bai LP, Ye ZJ, Lin WJ, Qi ZQ, Liu ZC. [Transumbilical single-port access laparoscopic surgery for colorectal cancer]. Zhonghua Wei Chang Wai Ke Zazhi. 2011;14:34-36. [PubMed] [Cited in This Article: ] |
| 19. | Yu Y, Wang C, Zhou Z. Laparospcopic total mesorectal excision and anal sphincter preservation for patients with rectal cancer: a single center experience with 611 cases. Zhonghua Puwaike Shoushuxue Zazhi (Electronic Version). 2009;493-497. [Cited in This Article: ] |