Published online Apr 7, 2015. doi: 10.3748/wjg.v21.i13.4020
Peer-review started: September 13, 2014
First decision: October 14, 2014
Revised: October 22, 2014
Accepted: November 7, 2014
Article in press: November 11, 2014
Published online: April 7, 2015
AIM: To check the efficacy of the PERFACT procedure in highly complex fistula-in-ano.
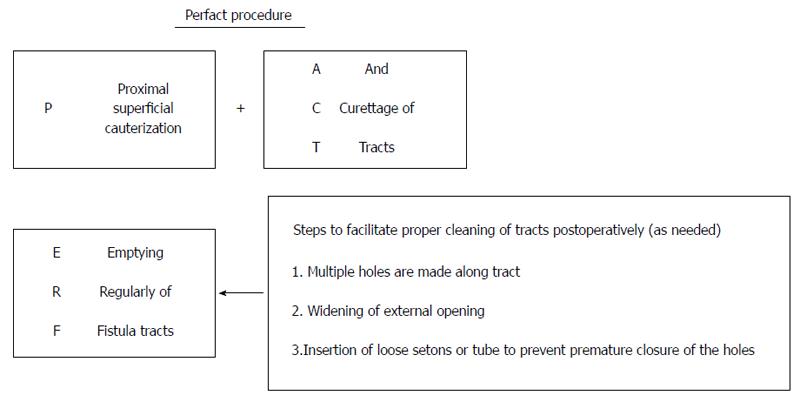
METHODS: The PERFACT procedure (proximal superficial cauterization, emptying regularly fistula tracts and curettage of tracts) entails two steps: superficial cauterization of mucosa at and around the internal opening and keeping all the tracts clean. The principle is to permanently close the internal opening by granulation tissue. This is achieved by superficial electrocauterization at and around the internal opening and subsequently allowing the wound to heal by secondary intention. Along with this, all the tracts are curetted and it is ensured that they remain empty and clean in the postoperative period until they heal completely. The latter step also facilitates the closure of the internal opening by preventing collected fluid in the tracts from entering the internal opening and thus not letting it close. Objective incontinence scoring was done preoperatively and 3 mo after the operation.
RESULTS: Fifty-one patients with complex fistula-in-ano were prospectively enrolled. The median follow-up was 9 mo (5-14 mo). The mean age was 42.7 ± 11.3 years. Male:female ratio was 43:8. Fistula was recurrent in 76.5% (39/51), horseshoe in 50.1% (26/51), had multiple tracts in 52.9% (27/51), had an associated abscess in 41.2% (21/51), was anterior in 33.3% (17/51), the internal opening was not found in 15.7% (8/51) and 9.8% (5/51) of fistulas had a supralevator extension. Seven patients were excluded (5 lost to follow up, 2 with tuberculosis leading to/associated with fistula-in-ano). The success rate was 79.5% (35/44) and the recurrence rate was 20.5% (9/44). Out of these recurrences, three underwent reoperation (2 PERFACT procedure, 1 fistulotomy) and all three were successful. Thus, the overall success rate was 86.4%. The only complication was a non-healing tract in 9.1% (4/44) of patients. There was no significant change in objective incontinence scores three months after the operation. The pain was minimal, with all patients resuming their normal activities within 72 h of the operation.
CONCLUSION: The PERFACT procedure is a new effective method for complex fistula-in-ano, effective even in fistula associated with abscess, supralevator fistula-in-ano and where the internal opening is non-localizable.
Core tip: The PERFACT procedure is a simple, economical and novel method to cure complex fistula-in-ano. It is associated with little pain, low morbidity and minimal risk of incontinence as both the anal sphincters are completely preserved. It is quite effective in complex fistula cases where other methods do not have a high success rate, like in horseshoe fistula, fistula with multiple tracts, recurrent fistula and fistula with supralevator extension. The PERFACT procedure is also quite successful in cases where the internal opening cannot be localized and in patients presenting with perianal/ischiorectal abscess where it can be done as a definitive procedure at the initial presentation.
- Citation: Garg P, Garg M. PERFACT procedure: A new concept to treat highly complex anal fistula. World J Gastroenterol 2015; 21(13): 4020-4029
- URL: https://www.wjgnet.com/1007-9327/full/v21/i13/4020.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i13.4020
There is no satisfactory treatment of complex fistula-in-ano to date. A fistula-in-ano is termed “complex” when the track crosses > 30%-50% of the external sphincter (high-transsphincteric, suprasphincteric and extrasphincteric), is anterior in a female, is recurrent, has multiple tracks, or the patient has preexisting incontinence, local irradiation or Crohn’s disease[1-4]. In spite of several new procedures, such as anal fistula plug[5,6], ligation of intersphincteric fistula tract (LIFT)[7], video assisted anal fistula treatment (VAAFT)[8], laser-FiLaC[9] and the OTSC proctology procedure[10] tried in the last decade, the challenge of successfully treating complex anal fistula remains intact. The two main issues in managing such fistulas are to minimize the recurrence rate and prevent any deterioration in continence levels.
Proximal superficial cauterization, emptying regularly fistula tracts and curettage of tracts (PERFACT procedure) is a novel concept in the management of complex fistula-in-ano. In this procedure, the fistula healing entails two components closure of the internal opening and healing of the tract/tracts. The aim is to use body’s natural healing tissue (granulation tissue) to close the internal opening. This is done by electrocauterizing the internal opening and the area around it in the anal canal. The tract/tracts are thoroughly curetted and the infected tract lining (epithelium) of the tracts is taken out. To ensure proper healing, it is important to keep the anal canal wound clean and the tracts empty in the postoperative period.
Patients with complex fistula-in-ano were enrolled in a prospective study over a period of one and a half years. The institutional ethics committee reviewed and approved the study. Informed written consent was taken from every patient.
All types of complex fistula-in-ano including: (1) fistula associated with multiple tracts; (2) horse shoe fistulas; (3) recurrent fistulas; (4) anterior fistula in females; (5) fistula with long tracts (any tract length > 10 cm); (6) fistula with supralevator blind extension (not with high rectal opening); (7) fistula where internal opening cannot be localized; and (8) fistula associated with abscess/pus collections. It was used as a first line definitive procedure in patients with anal fistulas presenting with ischiorectal or perianal abscess.
(1) Simple low fistula; and (2) fistula with supralevator rectal opening (on MRI and/or examination on the operating table).
Vaizey objective incontinence scoring was done preoperatively and at 3 mo after the operation[11]. On a scale of 0-24, a score 0 implied perfect continence and a score of 24 meant total incontinence.
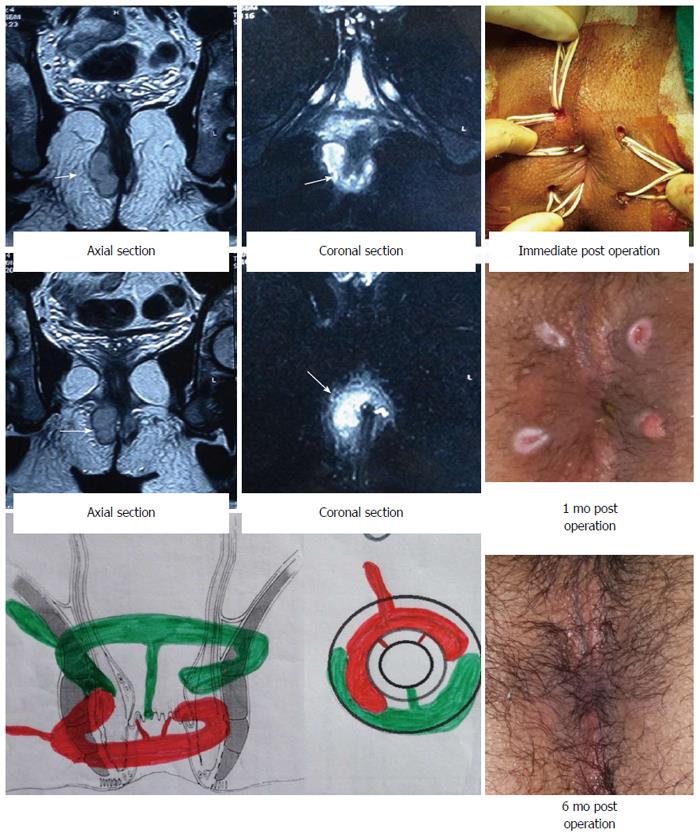
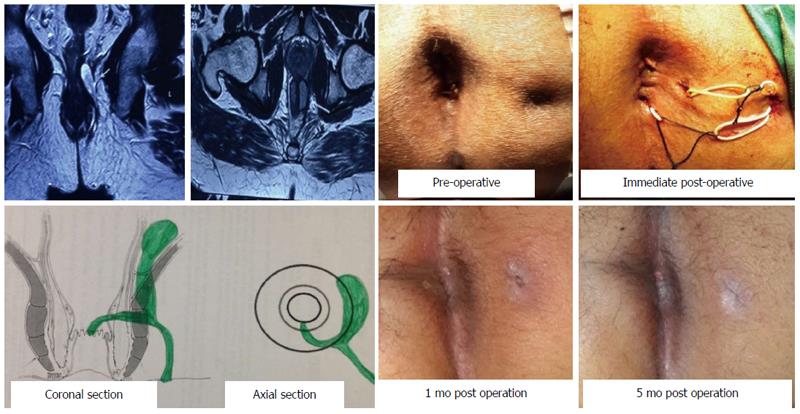
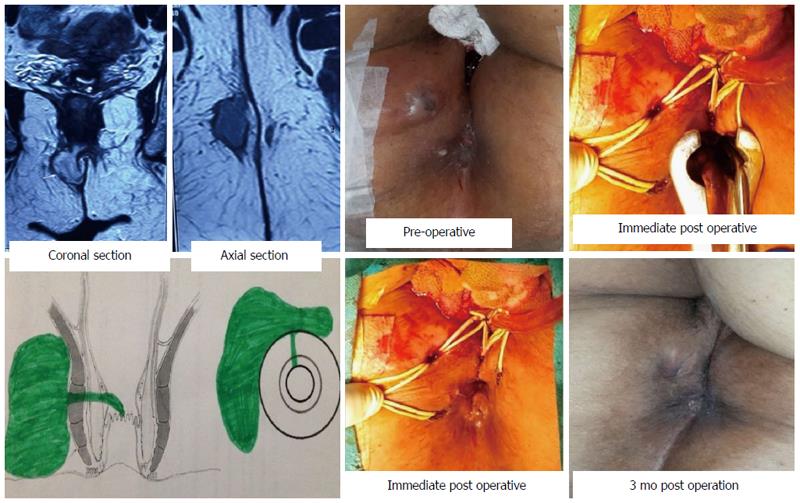
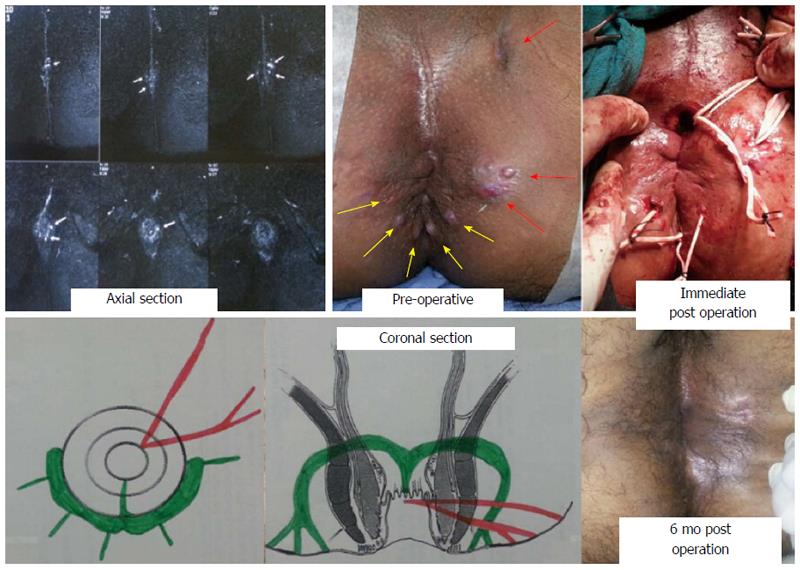
A pre-operative MRI scan was done in every case to accurately map all the fistula tracts (Figure 1). A schematic diagram consisting of coronal and transverse sections (Figure 1) was made based on the MRI.
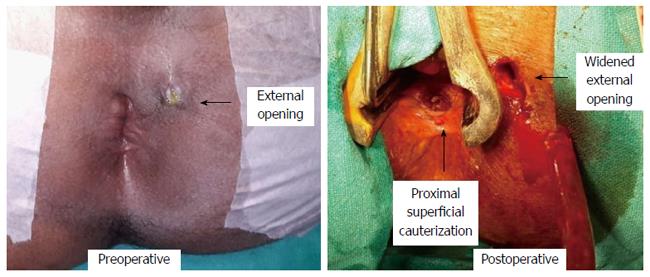
The PERFACT procedure had three steps (Figure 2): (1) proximal superficial cauterization: the area around the internal opening was freshened and de-epithelized by electrocautery (Figure 3) and the wound was encouraged to heal by secondary intention (granulation tissue). This usually closed the internal opening in about 10-12 d; (2) curettage of tracts: all the tracts were thoroughly curetted and debrided of their lining with a curette; and (3) emptying regularly fistula tracts: the curetted tracts were kept clean and empty of any serous fluid so as to ensure that the tracts healed (closed) by granulation tissue. Keeping all the tracts clean until they healed completely was a challenging task and the most demanding step of the procedure. It took 4-8 wk (occasionally even longer) for all the tracts to heal fully. Until that time, regular cleaning of the tracts was done.
To ensure proper cleaning of the tracts, the following steps (one or multiple depending upon the requirement and fistula characteristics) could be done in a patient: (1) multiple holes were made along the straight or the horseshoe tract (Figures 4, 5, 6, 7 and 8) in such a way that the farthest corner of the tract could be cleaned with ease; (2) the external opening was widened and the scarred puckered skin (if present) was excised. The aim was to make the opening bigger than 1 cm × 1 cm (Figure 3). This facilitated cleaning of the tracts for a longer duration; and (3) loose seton or tube were put in the tracts to prevent the premature closure of the external opening. These were removed 10-12 d after the operation (Figures 4, 5, 6, 7 and 8).
A saddle block (spinal anesthesia) or a short general anesthesia was given. The patient was positioned in a lithotomy or a prone jack-knife position. The internal opening was localized. This was facilitated by injecting saline, povidine iodine or hydrogen peroxide through the external opening.
Proximal superficial cauterization (Figure 3) was carried out with electrocautery around the internal opening, cauterizing only the mucosa and superficial part of the internal sphincter. The crypt glands, the internal opening and the tissue around it were cauterized. This usually resulted in an oval area, approximately 1 cm (wide) and 2 cm (long), with the internal opening at the center of the wound (Figure 3). After cauterization, the wound was left as such and no attempt was made to close the internal opening with any suture, stapler, glue or plug.
After this, the tracts were curetted in accordance with the MRI diagram and the tract lining was scraped out as much as possible with a blunt curette. While doing so, a finger was kept in the rectum so as to ensure that the curette did not accidentally perforate the rectum.
The patient was discharged on the operation day (if done under short general anesthesia) or the first postoperative day (if done under saddle or spinal anesthesia). He/she could resume all his/her normal activities on the same day. The patient was encouraged to walk briskly for 5 km every day. This helped to keep the tracts empty.
Postoperative cleaning aimed at healing two areas: the cauterized wound in the anal canal (around the internal opening) and the curetted tracts. The former was pivotal as the closure of the internal opening depended upon it and generally took about 10-12 d to heal. The latter was also needed for the complete closure of the fistula and took a variable time (4-8 wk) depending on the fistula characteristics (number, length and complexity of the tracts) and the patient co-morbidities (diabetes, anemia, hypoproteinemia etc.).
The cleaning process entailed cleaning the cauterized wound in the anal canal and regular cleaning and emptying of the curetted tracts. The former was done by gentle rubbing of the wound by doing a per rectal finger insertion. The latter was done by a cotton swab mounted on an artery forceps. No povidine iodine, hydrogen peroxide or any liquid was injected in to the tract during the cleaning process as this would have prevented the internal opening from closing. The cleaning was done by a trained nurse, a medical attendant or a relative. In our setting, teaching a relative was an economical and preferred option.
The cleaning process was done four times a day. For the first 10 d, the patient was called to the outpatient clinic for supervised cleaning once or twice a day depending upon the complexity of the fistula. After this, the patient could do the cleaning process at home.
Comparison of categorical variables was performed by χ2 analysis or Fisher’s exact test where appropriate. The significant cut off point was set at P < 0.05.
Fifty-one patients with complex fistula-in-ano were prospectively enrolled. The median follow-up was 9 mo (5-14 mo). The mean age was 42.7 ± 11.3 years. Male:female ratio was 43:8. The fistula characteristics were recurrent in 76.5% (39/51), horseshoe in 50.1% (26/51), multiple tracts in 52.9% (27/51), associated abscess in 41.2% (21/51) and anterior fistula in 33.3% (17/51). The internal opening could not be definitely traced intraoperatively in 15.7% (8/51) and there was associated supralevator extension in 9.8% (5/51) (Table 1). Seven patients were excluded from the analysis (5 lost to follow-up, 2 had biopsy proven mycobacterium tuberculosis). The fistula and all the associated tracts healed completely in 79.5% (35/44) of patients and there was recurrence of symptoms in 20.5% (9/44) of patients. Out of these, three underwent reoperation (two PERFACT procedure, one fistulotomy) and all three were successful (Table 2). The subgroup analysis showed that although the presence of multiple tracts and an abscess reduced the cure rate, it was not statistically significant (Fisher exact test P > 0.05) (Table 2). The only complication was a non-healing tract in 9.1% (4/44) of patients. There was no significant change in objective incontinence scores after the operation. The pain was minimal, with all patients resuming their normal activities within 72 h of the operation.
| Fistula characteristics | n = 51 |
| Recurrent | 39 (76.5) |
| Multiple tracts | 27 (52.9) |
| Horseshoe fistula | 26 (50.1) |
| Associated/presented with an abscess | 21 (41.2) |
| Anterior tract | 17 (33.3) |
| Internal opening not found | 8 (15.7) |
| Supralevator extension (blind) | 5 (9.8) |
| Parameter | Number (n = 44) | Healed | P value (Fisher’s exact test) | |
| Recurrent | Recurrent | 33 | 26 (78.8) | 0.2 (Not sig.) |
| Non-recurrent (primary) | 11 | 9 (81.8) | ||
| Multiple tracts | Multiple tracts | 21 | 15 (71.4) | 0.16 (Not sig.) |
| Single tract | 23 | 20 (86.9) | ||
| Horseshoe fistula | Horseshoe | 21 | 16 (76.2) | 0.17 (Not sig.) |
| Non-horseshoe | 23 | 19 (82.6) | ||
| Associated/presented with abscess | Abscess | 18 | 13 (72.2) | 0.17 (Not sig.) |
| No abscess | 26 | 22 (84.6) | ||
| Anterior tract | Anterior | 15 | 13 (86.6) | 0.18 (Not sig.) |
| Non-anterior | 29 | 22 (75.8) | ||
| Internal opening not found | 8 | 7 (87.5) | ||
| Supralevator extension (blind) | 4 | 3 (75) | ||
| Overall | After 1 procedure | 44 | 35 (79.5) | |
| After 2nd procedure in 3 patients | 44 | 38 (86.4) |
The PERFACT procedure is a novel concept to treat complex fistula-in-ano. It is simple to perform and easy to reproduce. The results (initial 79.5%, overall 86%) are quite impressive considering that all these patients had highly complicated fistula-in-ano (Table 1).
The concept behind the PERFACT procedure was very simple. It aimed to close the internal opening by proximal superficial cauterization in the anal canal (Figure 3). In the postoperative period, it was ensured that the wound healed by secondary intention so that the internal opening was sealed by granulation tissue.
The second step was curettage of the tracts. This ensured that the infected epithelium was removed and the freshened raw wound in the tracts led to the generation of the granulation tissue which would facilitate the closure of the tracts. However, the serous discharge of the granulation tissue needed to be thoroughly cleaned/removed from the tracts as otherwise the stagnant discharge would become infected, leading to a collection. The latter would not only lead to the rapid re-epithelialization of the tracts but would also flow into internal opening, preventing its closure.
The postoperative management was quite significant. It had two components: to keep the cauterized anal wound clean and to keep the tracts clean and empty. Any inadequacy in this care was detrimental to the final outcome.
The cauterization of the internal opening had been tried earlier without much success. The reason for the success of the same step in the PERFACT procedure needs explanation. Undoubtedly, the internal opening is the prime culprit in a fistula-in-ano by allowing ingress of the bacteria from the anal canal into the fistula tracts. However, once the tracts are formed and are lined by the infected epithelium, then it is a mutually propagating situation. The patent internal opening keeps the tracts infected and the infected collection in the tracts keep the internal opening patent. Therefore, an isolated attempt to close the internal opening would fail until it is accompanied by the meticulous cleaning, emptying and healing of all the associated tracts. This perhaps explains the rigorous need for regular tract cleaning in the postoperative period.
The concept behind this procedure was undoubtedly simple but to achieve good results in complex anal fistulas, it required detailed analysis of the MRI scan, careful planning and mapping of the tracts (preoperatively), meticulous curettage and cleaning of all the tracts (intraoperatively), and disciplined postoperative care (postoperatively). The main benefit of this procedure was minimal morbidity and the least risk of incontinence. The morbidity was minimal as no extensive tissue cutting was done. Apart from a small superficial wound in the anal canal, the external opening was widened (Figure 3) or a few holes were made in the perianal region (to drain accessory tracts) (Figures 4, 5, 6, 7 and 8). The anal wound was usually small and low as the internal opening was located mostly at the dentate line (Figure 3). So, the resultant wound was usually about 2 cm long and 1 cm wide. Due to the small wound and little pain, the patients were able to resume all their normal daily activities from the first postoperative day. The patients were encouraged to walk briskly for 4-5 kilometers from the first postoperative day as it facilitated keeping the tracts empty. Second major advantage was that as the external sphincter was completely spared, the negative impact on incontinence was minimal.
The procedure worked quite well in all types of complex fistula: fistula associated with multiple tracts, horse shoe fistulas, recurrent fistulas, anterior fistula in females, fistula with long tracts, fistula with supralevator blind extension (not with high rectal opening), fistula associated with abscess/pus collections and fistula where no definite internal opening could be localized intraoperatively (Figures 4, 5, 6, 7 and 8).
The PERFACT procedure was quite effective in horseshoe fistula and fistula with multiple tracts. About half of the fistula (50.1%) in our series had a horseshoe fistula and the cure rate was 76.2% (16/21) (Table 2) (Figures 4 and 5). In fact, one of the patients presented with a double horseshoe intersphincteric abscess which encircled the rectum circumferentially. This patient was also cured by this procedure (Figure 5). About 53% of patients had multiple tracts and the success rate in this subgroup was 71.4% (15/21). One of the patients had eight external openings and he underwent this procedure successfully (Figure 8).
In fistula with an associated abscess, the abscess was drained and the PERFACT procedure was carried out as described. There was no need to make a large incision as the setons and regular cleaning of the cavity in the postoperative period ensured that there was no recollection and good healing ensued. In our series, 41.2% patients presented with an abscess or had an associated significant abscess (Table 1). The PERFACT procedure was done as the definitive first line procedure and the cure rate was 72% (Table 2; Figures 4, 5 and 7).
The PERFACT procedure was effective in fistula cases where no definite internal opening could be localized intraoperatively. Failure to identify the internal opening during the operation perhaps happens because of the temporary closure of the internal opening due to debris or the oblique course of the collapsible tract through the sphincters. As in the literature, this can happen in up to 15-20% of cases[8]. In our series, this happened in 15.7% (8/44) of cases (Table 1). This procedure worked quite successfully in 87.5% (7/8) of such cases in our series (Figure 5) (Table 2). As the MRI was done preoperatively in every case, it helped to localize the tracts in the majority of cases and gave a reasonable idea of where the tract was coursing towards the rectum. This information along with the intraoperative examination findings (induration of the sphincter complex in the region of internal opening) helped to determine the possible site of the internal opening. At that place, the superficial cauterization was done. In two patients, the MRI picture created doubt that the tracts could be going both anteriorly and posteriorly and hence superficial cauterization was done at both places (Figure 5). Superficial cauterization was a safe step to do. Although it created a wound, it was not associated with any risk of incontinence as the wound was quite superficial. Therefore, in case of confusion/doubt, superficial cauterization can be done at two places.
This procedure was also effective in fistula with supralevator extension (blind). The procedure was carried out as described. The position of the supralevator tract was carefully assessed on MRI and intraoperatively this tract was carefully curetted while keeping a finger in the rectum (to avoid injuring the rectal wall). During the postoperative dressings, the supralevator tract was regularly cleaned for at least 2-3 wk (or as needed). While doing so, a finger was inserted in the rectum to avoid any injury. In our series, it was effective in providing cure in 75% of patients (3/4) with supralevator extension (Figure 6).
With careful postoperative management, most of the fistulas healed between 4-10 wk. In 9 (20.5%) patients, the procedure failed. The internal opening did not close and one or multiple tracts failed to heal. The likely reason was inability to regularly clean all the tracts postoperatively, leading to a collection in one of the tracts. This perhaps prevented the tracts as well as the internal opening from healing. Four (9%) of the patients had persistent serous/watery discharge for a prolonged period (10-16 wk). This happened in cases with long fistula tracts. The cauterized wound in the anal canal and the internal opening healed quite well in these cases, leading to the cessation of pus formation. However, the serous drainage was perhaps due to the re-epithelialization of the outer portion of the tract. We did gentle curettage of the tract in the office under topical anesthesia (lidocaine gel) and it helped to close the recalcitrant tract. However, multiple curettings were needed in two cases.
There are certain patients in whom the internal opening is enlarged/widened due to previous surgical interventions (like tightening setons). In these patients, proximal superficial cauterization fails or takes much longer to heal. In this subgroup, an advancement flap plus the intensified mechanical cleaning of the fistula tract could be a better option.
The PERFACT procedure adds a potentially useful treatment option to our armamentarium against complex fistula-in-ano. It complements the mucosal advancement flap, anal fistula plug, OTSC proctology, LIFT, VAAFT and glue procedures. The PERFACT procedure is simple and associated with lower morbidity and minimal risk of incontinence. Compared to a mucosal advancement flap, the PERFACT procedure is technically less demanding. Unlike an anal fistula plug, laser-FiLaC and OTSC proctology procedure[9,10], the PERFACT procedure can be done as a definitive procedure in fistula patients presenting with an acute abscess or collection. Unlike other existing procedures, the PERFACT procedure can be done in patients where the internal opening cannot be definitely localized. Lastly, unlike fistulotomy and cutting tightening setons, the PERFACT procedure is associated with a minimal risk of incontinence.
The PERFACT procedure has certain distinct advantages. It is associated with the least risk of incontinence, morbidity is minimal, pain is not much and the patient is able to resume normal activities within 1-2 d of the operation. It has a high success rate in all types of complex fistula-in-ano, including horseshoe fistula, recurrent fistula and fistula with multiple tracts. It is effective in highly complicated cases where the other procedures do not work well, such as fistula with supralevator extension, fistula with associated abscess and fistulas where the internal opening cannot be localized. Moreover, the PERFACT procedure can be done as the first line definitive procedure in fistulas presenting with an anorectal or ischiorectal abscess (rather than doing an incision and drainage initially and a definitive procedure later). Another advantage of this procedure is its cost effectiveness. No expensive equipment/gadget is required, operation duration is 15-30 min and hospital stay is only 12-24 h (can be done as a day care procedure). As there is minimal incision/cutting, there is very little scarring and distortion of the anatomy. Last but not the least, this procedure is quite simple to do and reproduce.
The procedure has its limitations. The PERFACT procedure is not effective in cases where a supralevator tract has a high rectal opening. It is also not indicated in low fistula where there is no sphincter involvement. Secondly, meticulous postoperative care is required, especially for the first two weeks. Although most of the patients are back to their normal routine the first day after the operation, they need to come for twice daily follow-up for at least ten days. Active participation/cooperation is needed from a relative/acquaintance. In our country, teaching a relative (spouse in the majority of cases) was an economically viable and acceptable option. Thirdly, the problem of prolonged serous discharge adds to the morbidity in few patients. Lastly, the long term follow-up (> 3 years) results are awaited.
To conclude, the PERFACT procedure is a simple novel method to treat complex and highly complex anal fistula. This includes fistula-in-ano with multiple tracts, horse shoe fistulas, recurrent fistulas, anterior fistula in females, supralevator fistula, fistula where internal opening cannot be localized and as a first line definitive procedure in patients with fistula-in-ano presenting with ischiorectal or perianal abscess. However, long term multicenter trials are needed with larger numbers of patients to substantiate these findings.
Complex anal fistula is difficult to treat because of the high risk of recurrence of the disease and the danger of incontinence (losing control over the bowel motions). Apart from regular pus discharge and pain, a complex anal fistula on a long term basis also increases the risk of ano-rectal cancer.
Apart from several existing methods, many new procedures have been developed to cure this dreaded illness. However, achieving a high success rate (low recurrence) and a low incontinence rate at the same time remains a challenge. The procedures which have a low recurrence rate (high cure rate) have a high incidence of incontinence and the procedures which have a low risk of incontinence have high recurrence rates.
The PERFACT procedure is a new procedure that involves no cutting of anal sphincters (muscles which control bowel motions). Hence, the risk of incontinence is negligible after this procedure. At the same time, this procedure is associated with a high success rate (low recurrence rate). The morbidity of this procedure is also quite low as the patient can resume his/her normal activities within 1-2 d of the operation.
The medium term follow-up results are quite encouraging. If these results are replicated on a larger scale, then this method has the potential to become the procedure of choice for complex anal fistulas.
“PERFACT” in the PERFACT procedure does not mean perfect (ideal). Here, PERFACT is a mnemonic which stands for proximal superficial cauterization, emptying regularly fistula tracts and curettage of tracts. In proximal superficial cauterization, proximal implies that only the lower part of the anal canal is cauterized (as the internal opening is usually located at the dentate line) and superficial implies that only the mucosa and few medial fibers of the internal sphincter are cauterized, leaving the majority of the internal sphincter and complete external sphincter intact.
This is an interesting description of a novel method of anal fistula closure, including cauterization of the internal opening, curettage of the fistula tract and mechanical debridement of the tract.
P- Reviewer: Mennigen R S- Editor: Qi Y L- Editor: Roemmele A E- Editor: Liu XM
| 1. | Whiteford MH, Kilkenny J, Hyman N, Buie WD, Cohen J, Orsay C, Dunn G, Perry WB, Ellis CN, Rakinic J. Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised). Dis Colon Rectum. 2005;48:1337-1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 237] [Cited by in F6Publishing: 191] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 2. | Parks AG, Stitz RW. The treatment of high fistula-in-ano. Dis Colon Rectum. 1976;19:487-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 89] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Mizrahi N, Wexner SD, Zmora O, Da Silva G, Efron J, Weiss EG, Vernava AM, Nogueras JJ. Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum. 2002;45:1616-1621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 266] [Cited by in F6Publishing: 211] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 4. | Kodner IJ, Mazor A, Shemesh EI, Fry RD, Fleshman JW, Birnbaum EH. Endorectal advancement flap repair of rectovaginal and other complicated anorectal fistulas. Surgery. 1993;114:682-689; discussion 689-690. [PubMed] [Cited in This Article: ] |
| 5. | Johnson EK, Gaw JU, Armstrong DN. Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Dis Colon Rectum. 2006;49:371-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 240] [Cited by in F6Publishing: 247] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 6. | Garg P, Song J, Bhatia A, Kalia H, Menon GR. The efficacy of anal fistula plug in fistula-in-ano: a systematic review. Colorectal Dis. 2010;12:965-970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Rojanasakul A. LIFT procedure: a simplified technique for fistula-in-ano. Tech Coloproctol. 2009;13:237-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 8. | Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol. 2011;15:417-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 167] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 9. | Giamundo P, Geraci M, Tibaldi L, Valente M. Closure of fistula-in-ano with laser--FiLaC™: an effective novel sphincter-saving procedure for complex disease. Colorectal Dis. 2014;16:110-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 10. | Prosst RL, Joos AK, Ehni W, Bussen D, Herold A. Prospective pilot study of anorectal fistula closure with the OTSC Proctology. Colorectal Dis. 2015;17:81-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Vaizey CJ, Carapeti E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44:77-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 963] [Cited by in F6Publishing: 908] [Article Influence: 36.3] [Reference Citation Analysis (0)] |