Published online Jun 28, 2013. doi: 10.3748/wjg.v19.i24.3911
Revised: March 26, 2013
Accepted: April 10, 2013
Published online: June 28, 2013
Choledochal cyst (CC) is a rare, congenital anomaly of the bile ducts. We describe a 26-year-old male patient who was transferred to our hospital with a reported traumatic rupture of cystic liver lesions following a fall. At the time of injury, the patient experienced severe abdominal pain. He was found to have peritonitis and abdominal hemorrhage, which is quite rare. Laparotomy revealed 3000 mL fluid consisting of a mixture of blood, bile and inflammatory effusion in the peritoneal cavity. The liver, gallbladder, spleen, stomach, duodenum, small intestine, and colon appeared normal. A large cystic mass was discovered near the porta hepatis. This mass, which connected to the hepatic bifurcation and gallbladder had a 5 cm rupture in the right wall with active arterial bleeding. Abdominal computed tomography (CT) and emergency laparotomy revealed rupture of a huge type IVa CC. The patient was successfully managed by primary cyst excision, cholecystectomy, and Roux-en-Y end-to-side hepaticojejunostomy reconstruction. The postoperative course was uneventful and the patient was discharged on the 12th day of hospitalization. Four weeks after surgery, abdominal CT scan showed pneumatosis in the intrahepatic bile duct, and intrahepatic dilatation which decreased following adequate biliary drainage. The patient has remained well in the close follow-up period for 9 mo.
Core tip: Choledochal cyst (CC) is a rare, congenital anomaly of the bile ducts. We describe a young man who was transferred to our hospital with a reported traumatic rupture of liver cystic lesions. The patient was found to have peritonitis and abdominal hemorrhage, which is quite rare. Abdominal computed tomography and emergency laparotomy revealed rupture of a huge type IVa CC. The patient was successfully managed by primary cyst excision, cholecystectomy, and Roux-en-Y end-to-side hepaticojejunostomy reconstruction.
- Citation: Duan YF, Yang B, Zhu F. Traumatic rupture of a type IVa choledochal cyst in an adult male. World J Gastroenterol 2013; 19(24): 3911-3914
- URL: https://www.wjgnet.com/1007-9327/full/v19/i24/3911.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i24.3911
Choledochal cyst (CC) is a rare congenital disease characterized by single or multiple dilatations of the intra and/or extrahepatic biliary tree. There is a higher incidence of CC in females. In CC, spontaneous perforation is observed in 1.8%-7% of all cases. Nevertheless, reports of traumatic rupture of CC are extremely rare. Herein, we describe a young man who was transferred to our hospital with a reported traumatic rupture of liver cystic lesions. The patient was found to have peritonitis and abdominal hemorrhage. Abdominal computed tomography (CT) and emergency laparotomy revealed rupture of a huge type IVa choledochal cyst. The patient was successfully managed by primary cyst excision, cholecystectomy, and Roux-en-Y end-to-side hepaticojejunostomy reconstruction.
A 26-year-old male patient fell in a bathroom and suffered an impact to the abdomen. At the time of injury, the patient experienced severe abdominal pain. He was immediately admitted to a local hospital. On ultrasound examination, there was moderate free fluid in the peritoneal cavity, especially around the liver, and multiple cystic lesions in the liver. A plain radiograph of the chest was normal, and a plain radiograph of the abdomen revealed no gastrointestinal perforation. Abdominal paracentesis was performed with bloody fluid aspirated from the peritoneal cavity.
Two hours after injury, he was transferred to our hospital with a reported traumatic rupture of liver lesions. The patient’s past medical history was unremarkable with the exception of transient and recurrent mild abdominal pain in childhood. His blood pressure was 100/65 mmHg and heart rate was 126 beats/min. Physical examination revealed tenderness and guarding of the whole abdomen. The results of laboratory examination were as follows: white blood cells: 9.88 × 109/L, neutrophils: 69.4%, hemoglobin: 105 g/L, and hematocrit: 0.31.
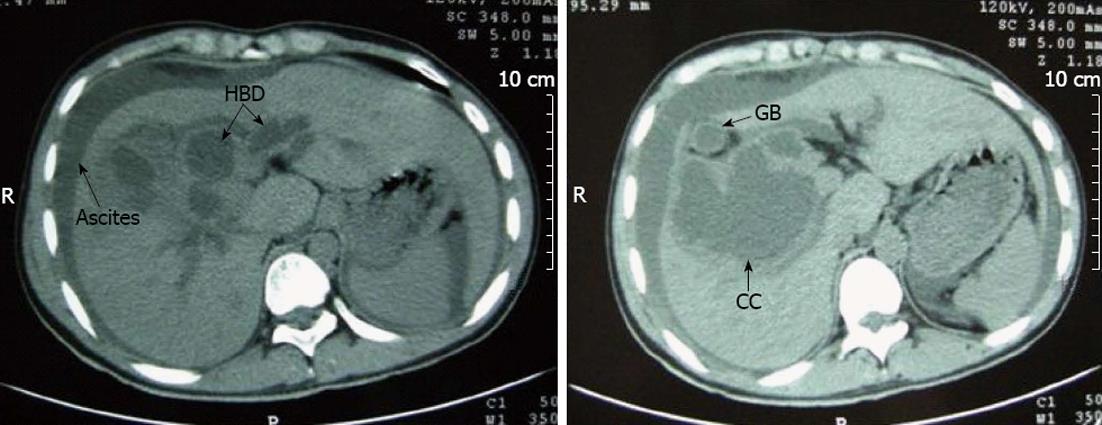
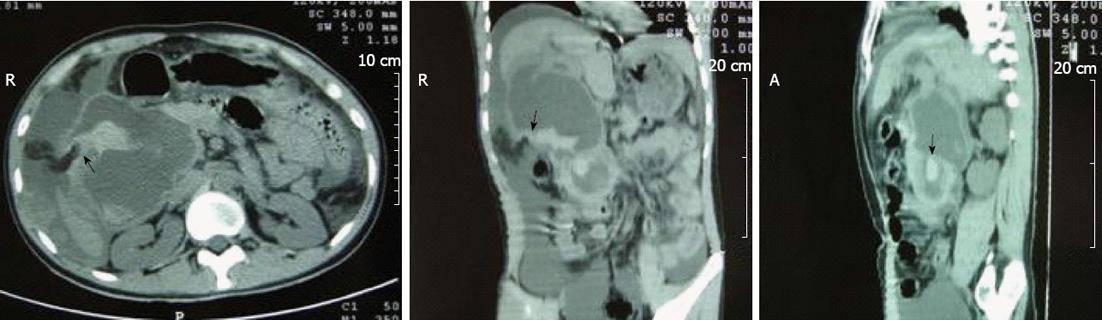
An urgent abdominal CT scan revealed ascites and a normal-sized gallbladder, dilatation of the intrahepatic bile duct, and a 13 cm × 10 cm × 9 cm cyst with hemorrhage in the common bile duct region, extending from the porta hepatis down to the level of the pancreatic head (Figures 1 and 2). He was taken emergently to the operating room with a presumed diagnosis of CC rupture.
Laparotomy revealed 3000 mL fluid consisting of a mixture of blood, bile and inflammatory effusion in the peritoneal cavity. The liver, gallbladder, spleen, stomach, duodenum, small intestine, and colon appeared normal. A large cystic mass was discovered near the porta hepatis and was dissected circumferentially. This mass, which connected to the hepatic bifurcation and gallbladder had a 5 cm rupture in the right wall with active arterial bleeding. It was confirmed to be a congenital CC, type IVa, according to Todani’s classification[1].
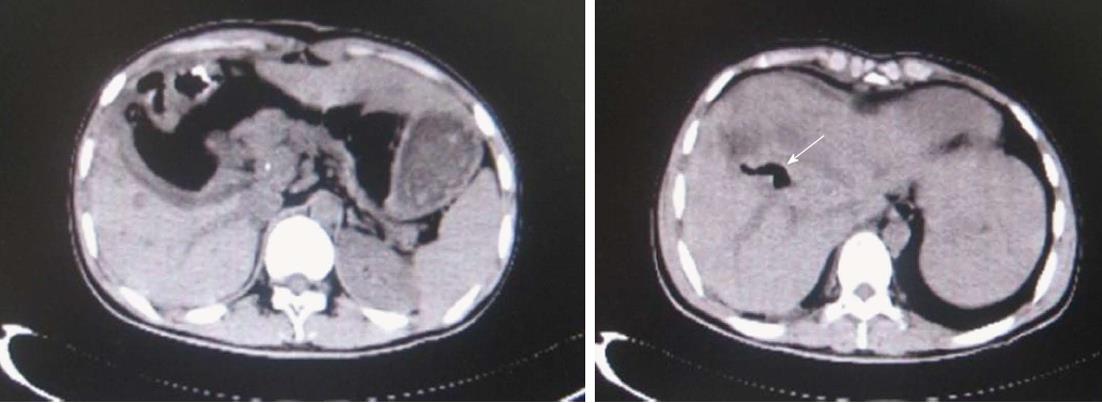
Because intraperitoneal inflammation was moderate, a complete cyst excision with cholecystectomy and Roux-en-Y end-to-side hepaticojejunostomy reconstruction were performed. The postoperative course was uneventful and the patient was discharged on the 12th day of hospitalization. Histological sections of the surgical margins and the operative specimen did not reveal malignancy. The patient has remained well in the close follow-up period for 9 mo. Four weeks after surgery, abdominal CT scan showed pneumatosis in the intrahepatic bile duct, and intrahepatic ductal dilatation, which was reduced following adequate biliary drainage (Figure 3).
Choledochal cyst is a rare congenital disease characterized by single or multiple dilatations of the intra and/or extrahepatic biliary tree. Although the incidence in the Western population is 1 in 100000-150000 live births, it is remarkably higher in Asian countries, particularly in Japan, where these cysts can be found in up to 1 in 1000 live births[2]. The incidence is higher in females, with a male/female ratio of 1:3[3]. These cysts are typically a surgical problem of infancy and childhood, however, the diagnosis is delayed until adulthood in nearly 20% of patients[4]. In CC, spontaneous perforation is observed in 1.8%-7% of all cases[5]. Nevertheless, reports of traumatic rupture of CC are extremely rare. As far as we know, only a few cases have been described in the literature[6-13].
The classical triad of jaundice, right upper quadrant mass, and abdominal pain is present in only a minority of patients[14]. Other presenting features of CC are cholangitis, pancreatitis, and biliary peritonitis from cyst rupture[5]. However, our patient was found to have peritonitis and abdominal hemorrhage, which is quite rare.
Ultrasound is the initial examination of choice in suspected CC[15]. Nevertheless, inherent limitations (e.g., gas in the bowel, intraperitoneal inflammation, etc.) and the radiologist’s skill may affect diagnosis. CT is required when the distal common bile duct is not visualized due to bowel gas. This imaging technique is excellent for detecting cystic lesions in the right upper abdomen, assessing their range and providing information regarding the impact of CC on the surrounding structures. Magnetic resonance cholangiopancreatography (MRCP) is the noninvasive imaging modality of choice for biliary pathology, and may offer as much as endoscopic retrograde cholangiopancreatography. However, MRCP is not suitable in patients who are unable to hold their breath for a few seconds, a requisite for breath-hold MRCP sequences.
Surgical treatment of CC should be recommended to reduce the risk of serious complications, such as cholangitis, pancreatitis, rupture, portal hypertension, cirrhosis, and cholangiocarcinoma[15]. In patients with type IV cysts without preoperative or intraoperative evidence of liver cirrhosis or biliary malignancy, resection of the entire portion of the extrahepatic cystic dilatation is currently recommended[16,17]. Reconstruction at the hepatic duct bifurcation is indicated. In rare cases where cyst rupture occurs, previous reports have speculated that a portal dissection and biliary reconstruction may be hazardous in the presence of bile peritonitis. These reports recommended primary management with temporary external drainage, by percutaneous transhepatic cholangiodrainage or by open placement of a T-tube[18,19]. Once the patient has recovered and has been thoroughly evaluated, a complete cyst excision, cholecystectomy, and hepaticojejunos- tomy can be performed[20]. However, this requires long-term maintenance of a T-tube and a second laparotomy. Furthermore, complications may occur in the interim. However, bile is aseptic, and even if bile drains into the abdominal cavity from a CC rupture, the possibility of this condition developing into generalized peritonitis is slight because such peritonitis will be chemical. In our patient, chronic inflammation induced thickening of the CC and fibrous adhesion with adjacent tissues, thus no shrinkage of the cyst cavity was observed following rupture of the CC which was excised. In recent years, due to progress in imaging diagnosis, it has become possible to diagnose the condition early. Therefore, in our opinion, treatment methods must also change. The case reported here demonstrated the feasibility of primary cyst excision and biliary reconstruction.
In conclusion, traumatic rupture of type IVa CC in an adult male is rare. A thorough preoperative diagnostic workup, with CT and/or MRCP, will guide surgeons to an appropriate operative strategy. Primary complete cyst excision, cholecystectomy and Roux-en-Y hepaticojejunostomy reconstruction are the preferred management options.
The authors thank Dr. Xiao-Dong Li and Dr. Yan Tan for their technical support.
P- Reviewers Kozarek R, Lee HC, Melek M, Moralioglu S S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Todani T, Watanabe Y, Toki A, Morotomi Y. Classification of congenital biliary cystic disease: special reference to type Ic and IVA cysts with primary ductal stricture. J Hepatobiliary Pancreat Surg. 2003;10:340-344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 148] [Article Influence: 7.4] [Reference Citation Analysis (1)] |
| 2. | Congo K, Lopes MF, Oliveira PH, Matos H, Basso S, Reis A. Outcomes of choledochal cysts with or without intrahepatic involvement in children after extrahepatic cyst excision and Roux-en-Y hepaticojejunostomy. Ann Hepatol. 2012;11:536-543. [PubMed] [Cited in This Article: ] |
| 3. | Shah OJ, Shera AH, Zargar SA, Shah P, Robbani I, Dhar S, Khan AB. Choledochal cysts in children and adults with contrasting profiles: 11-year experience at a tertiary care center in Kashmir. World J Surg. 2009;33:2403-2411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Khandelwal C, Anand U, Kumar B, Priyadarshi RN. Diagnosis and management of choledochal cysts. Indian J Surg. 2012;74:29-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Ando K, Miyano T, Kohno S, Takamizawa S, Lane G. Spontaneous perforation of choledochal cyst: a study of 13 cases. Eur J Pediatr Surg. 1998;8:23-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Ellis H, Cronin K. Bile peritonitis. Br J Surg. 1961;48:166-171. [PubMed] [Cited in This Article: ] |
| 7. | Chen W, Chang C, Hung W. Congenital choledochal cyst: with observations on rupture of the cyst and intrahepatic ductal dilatation. J Pediatr Surg. 1973;8:529-538. [PubMed] [Cited in This Article: ] |
| 8. | Battersby C. Ruptured choledochal cyst: recognition and management. Aust N Z J Surg. 1978;48:515-517. [PubMed] [Cited in This Article: ] |
| 9. | Shibata T, Hayakawa T, Kondo T, Kitagawa M, Sakai Y, Ono H, Kiriyama S, Nimura Y, Hayakawa N, Kamiya J. Analysis of pancreatic enzymes in the bile of congenital choledochal cyst with anomalous pancreaticobiliary ductal union. Nihon Shokakibyo Gakkai Zasshi. 1989;86:1513-1518. [PubMed] [Cited in This Article: ] |
| 10. | Sándor L, Bali I, Bozo A, Farkas G. Ruptured retroperitoneal bile duct cyst. An extremely rare injury after blunt abdominal trauma. Unfallchirurg. 1991;94:360-362. [PubMed] [Cited in This Article: ] |
| 11. | Raj JP, Walsh M. Choledochal cyst and blunt trauma--case report. Injury. 2002;33:644-646. [PubMed] [Cited in This Article: ] |
| 12. | Nagae I, Tsuchida A, Tanabe Y, Takahashi S, Minato S, Koyanagi Y, Aoki T. Traumatic rupture of choledochal cyst in a child. J Pediatr Surg. 2005;40:E7-E8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Garrison AP, Weiner T, Lange P. Traumatic rupture of a choledochal cyst masking as a duodenal hematoma. Pediatr Surg Int. 2008;24:1247-1249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Rattan KN, Khurana P, Budhiraja S, Malik V, Pandit SK. Choledochal cyst: a 10-year experience. Indian J Pediatr. 2000;67:657-659. [PubMed] [Cited in This Article: ] |
| 15. | Stipsanelli E, Valsamaki P, Tsiouris S, Arka A, Papathanasiou G, Ptohis N, Lahanis S, Papantoniou V, Zerva C. Spontaneous rupture of a type IVA choledochal cyst in a young adult during radiological imaging. World J Gastroenterol. 2006;12:982-986. [PubMed] [Cited in This Article: ] |
| 16. | Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003;10:352-359. [PubMed] [Cited in This Article: ] |
| 17. | Lal R, Agarwal S, Shivhare R, Kumar A, Sikora SS, Saxena R, Kapoor VK. Type IV-A choledochal cysts: a challenge. J Hepatobiliary Pancreat Surg. 2005;12:129-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Söreide K, Körner H, Havnen J, Söreide JA. Bile duct cysts in adults. Br J Surg. 2004;91:1538-1548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 113] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Fragulidis GP, Marinis AD, Anastasopoulos GV, Vasilikostas GK, Koutoulidis V. Management of a ruptured bile duct cyst. J Hepatobiliary Pancreat Surg. 2007;14:194-196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |