Published online Jun 7, 2013. doi: 10.3748/wjg.v19.i21.3291
Revised: March 9, 2013
Accepted: April 13, 2013
Published online: June 7, 2013
AIM: To investigate gastric antisecretory and gastroprotective activity of bovine hemoglobin (B-Hb) in rats.
METHODS: Adult Albino-Wistar rats were divided into groups of 6 animals each. B-Hb in doses of 100, 300 and 900 mg/kg body weight was tested for gastric acid secretion and antiulcer activity. Gastric secretions were measured 6 h after pylorus ligation in rats pretreated with B-Hb. The acidity was measured by titrating gastric contents against 0.01 mol/L NaOH to pH 7. Indomethacin ulcers were produced by oral administration of 30 mg/kg bw in the rats pretreated with B-Hb one hour before indomethacin. Six hours after indomethacin stomach removed and ulcer index was recorded. Ethanol ulcer were produced by 1 mL of ethanol in the rats pretreated with B-Hb 30 min before the ethanol. One hour after ethanol stomach were cut open to score ulcers. Histological examination and analysis of gastric wall mucus, non-protein sulfhydryl groups (NP-SH), and myeloperoxidase (MPO) were carried in gastric tissue following ethanol administration.
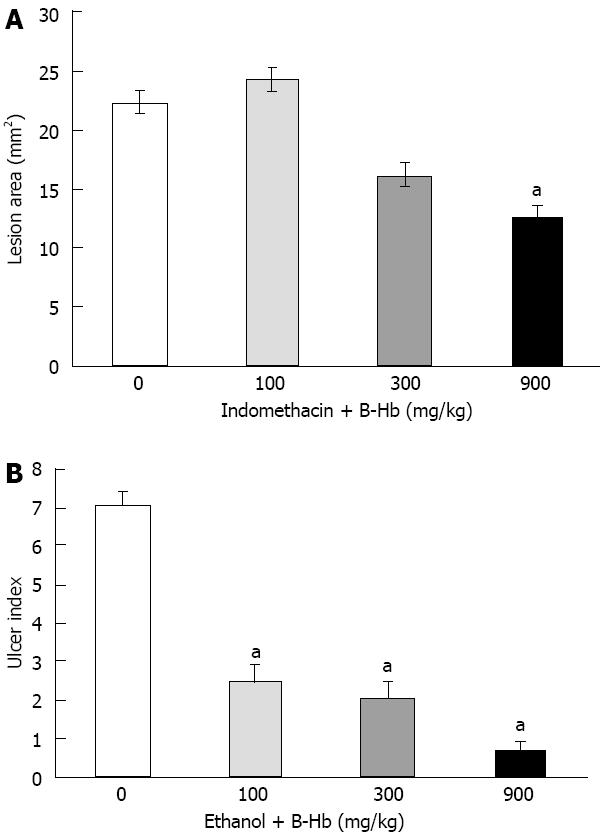
RESULTS: In control rats pylorus ligation for 6 h resulted in the accumulation of 8.1 ± 0.61 mL of gastric secretion. The treatment of the rats with 100, 300 and 900 mg/kg of B-Hb produced a significant decrease in the volume of gastric secretion 5.6 ± 0.63, 5.5 ± 0.75 and 4.7 ± 0.58 mL respectively as compared to the control group [analysis of variance (ANOVA) F = 4.77, P < 0.05]. The lesion area in the control group was found to be 22.4 ± 3.2 mm2 six hours after the administration of indomethacin. Treatment of rats with B-Hb at doses of 100 mg/kg (24.3 ± 3.29 mm2), 300 mg/kg (16.2 ± 1.45 mm2) and 900 mg/kg (12.6 ± 1.85 mm2) produced a dose dependent decreased the lesion scores (ANOVA F = 4.50, P < 0.05). The ulcer index following one hour after 1 mL ethanol was 7.1 ± 0.31. Pretreatment of rats with B-Hb at the doses of 100 mg/kg (2.5 ± 0.42), 300 mg/kg (2.1 ± 0.4) and 900 mg/kg (0.7 ± 0.21) significantly inhibited the formation of gastric lesions (ANOVA F = 63.26, P < 0.0001). Histological examination of gastric mucosa following ethanol showed significant lesions in the form of gastric pits with detachment of the surface epithelium; vacuolation of epithelial cells and elongation of microvessels. The changes were dose-dependently attenuated by B-Hb. The treatment of rats with ethanol significantly decreased the Alcian blue binding capacity of gastric wall mucus (480 ± 25.6 μg Alcian blue/g of tissue) as compared to control rats (667 ± 25.8 μg). Pretreatment of rats with B-Hb at the doses of 100 mg/kg (516 ± 31.6 μg/g), 300 mg/kg (558 ± 28.8 μg/g) and 900 mg/kg (654 ± 33.8 μg/g) significantly attenuated ethanol induced depletion of gastric wall mucus (ANOVA F = 8.05, P < 0.005). A significant and dose dependent increase of gastric mucosal NP-SH (ANOVA F = 19.62, P < 0.001) and decrease in MPO activity (ANOVA F = 3.1, P < 0.05) was observed in B-Hb treated rats.
CONCLUSION: B-Hb possesses significant gastric antisecretory and gastroprotective activity against experimentally induced gastric lesion. The gastroprotective effects of B-Hb are accompanied by inhibition of neutrophils activity, reduction of oxidative stress and maintenance of mucosal integrity.
Core tip: In the recent years the treatment strategies for gastric ulcer diseases have significantly changed, mirroring the revolution in the understanding of its pathogenesis. Improved oxygenation in critically ischemic gastric mucosa has emerged as a method of choice to accelerate epithelization of erosive and ulcerative defects. Bovine hemoglobin (B-Hb) has been used in a wide range of applications including restoration of tissue oxygenation in ischemic condition. Our data show that B-Hb has significant anti-gastric acid secretory and gastroprotective activity. Further studies are warranted to determine the role of B-Hb in prophylaxis/treatment of gastric ulcer disease.
- Citation: Al Asmari AK, Al Omani S, Elfaki I, Tariq M, Al Malki A, Al Asmary S. Gastric antisecretory and antiulcer activity of bovine hemoglobin. World J Gastroenterol 2013; 19(21): 3291-3299
- URL: https://www.wjgnet.com/1007-9327/full/v19/i21/3291.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i21.3291
A variety of noxious factors and substances like alcohol, drugs, psychological stress, smoking and bacterial infection by Helicobacter pylori, to which the man is exposed in the present day life are known to have deleterious effect on gastric mucosa[1]. Organized at several levels the mucosal defense system comprise the pre-epithelial mucosal layer, the epithelial cell barrier, the mucosal microvasculature, the supply of the mucosa by enteric, extrinsic sensory and extrinsic autonomic neurons and mucosal immune system[2]. Maintenance and repair of gastric mucosa is a dynamic process associated with proliferation and migration of epithelial cells and connective tissue to maintain/regain mucosal architecture[3]. It involves complex host of mechanisms which work in tandem to protect gastric mucosa from damage as well as trigger the mechanism to repair mucosal defects by proliferating and migrating epithelial cells and connective tissue resulting in reconstruction of mucosal architecture[4]. Numerous studies have demonstrated the importance of gastric mucosal haemo-dynamics as a defensive factor of the gastric mucosa against injury[5-7]. Treatment with some prostaglandin derivatives such as prostaglandin E2 have been shown to increase mucosal blood flow and protect gastric mucosa against indomethacin and ethanol induced gastropathy by improving mucosal haemodynamics[8,9]. Oxygen delivery to the gastric mucosa is not only a function of blood flow but also depends on oxygen content in the arterial inflow. A possible strategy would be to supplement oxygen using hyperbaric oxygen (HBO) to overcome ischemic injury[10]. The use of HBO in the treatment of peptic ulcer raised the efficacy of the multimodality therapy and accelerated the epithelization of erosive and ulcerative defects[11,12]. An alternative method to improve oxygenation in critically ischemic tissue has emerged, which consists of using oxygen carriers, such as hemoglobin (Hb) or Hb based products[13]. These biomaterials have been initially developed to avoid the drawbacks of blood transfusions including immunologic reactions, blood-borne transmitted infections, limited availability and restricted storage time[14].
Hb is the iron-containing oxygen-transport metalloprotein in the red blood cells of all vertebrates. In blood Hb carries oxygen from the respiratory organs to the rest of the body where it releases the oxygen to burn nutrients to provide energy to power the functions of the organism, and collects the resultant carbon dioxide to bring it back to the respiratory organs to be dispensed from the organism. In mammals, Hb makes up about 97% of the red blood cells dry content, and around 35% of the total content including water[15]. Hemoglobin has an oxygen binding capacity of 1.34 mL per gram of hemoglobin[16], which increases the total blood oxygen capacity seventy-fold compared to dissolved oxygen in blood. A single mammalian hemoglobin molecule can bind (carry) up to four oxygen molecules[17]. Based on these properties cell free hemoglobin (CF-Hb) products have been successfully used in a variety of ischemic/hypoxic conditions[18,19].
Bovine hemoglobin (B-Hb) has been used for a wide range of applications, including their use to enhance oxygen delivery to tissues during conditions of ischemia or hypoxia[20,21]. Strate et al[13] reported that B-Hb is much more potent than autologous red blood cells in restoring tissue oxygenation in ischemic conditions. In view of the superiority of CF-Hb compared to erythrocyte and whole blood we studied the efficiency of B-Hb against experimentally induced gastric mucosal injury.
Adult Albino Wistar rats of either sex, weighing 150-200 g and fed on standard chow diet were used. They were divided into groups of 6 animals each. The distribution of animals into groups and the treatment allotted to each group were randomized. All the experiments were started between 8:00 and 10:00 in the morning. The protocol of the study was approved by the Institutional Research and Ethical Committee.
The aqueous solution of ulcerogens and B-Hb were freshly prepared before administration. The concentrations of drug were prepared in such a way that each rat received 0.5 mL of drug solution/100 g body weight.
Pylorus ligated (Shay) rats: The animals were fasted for 36 h with access to water ad libitum before the pylorus was ligated under ether anesthesia, care being taken not to cause bleeding or to occlude blood vessels[22]. B-Hb in doses of 100, 300 and 900 mg/kg body weight was given by gavage (ig) half an hour before pylorus ligation by oral route. The animals were sacrificed at 6 h after the pylorus ligation. The stomachs were removed, contents collected, volume measured, centrifuged and subjected to analysis for titratable acidity against 0.01 mol/L NaOH to pH 7 using a pH meter and total acid output was calculated.
Indomethacin-induced gastric lesion: Indomethacin was suspended in 1% carboxymethylcellulose in water and administered by gavage at the dose of 30 mg/kg body weight[23]. B-Hb in the doses of 100, 300 and 900 mg/kg body weight was administered by gavage 1 h before indomethacin. The animals were sacrificed 6 h using ether after indomethacin administration. The stomach were removed and opened along the greater curvature. After washing with saline the gastric lesions were quantified by a person unaware of the treatment protocol. The ulcer were scored according to the method of Valcavi et al[24]. The circular ulcer induced by indomethacin were assessed on the basis of their diameter: deep circular ulcers more than 8 mm diameter = 10; 7-8 mm = 8; 6-7 mm = 7; 5-6 mm = 6; 4-5 mm= 5; 3-4 mm= 4; 2-3 mm= 3; 1-2 mm= 2; and < 1 mm = 1. Deep linear ulcers 10 mm or more in length were scored 6, and linear ucers less than 10 mm in length were scored 3. The scores of each single lesion were then summed up for determination of the ulcer index.
Gastric lesions induced by ethanol (cytoprotection studies): The animals were administered (ig) with 1 mL of absolute ethanol[25]. B-Hb in the doses of 100, 300 and 900 mg/kg body weight was given (ig) 30 min before the administration of ethanol. One hour after the administration of ethanol the animals were sacrificed and examined for the lesions in stomachs. The patcheal lesions of stomach induced by ethanol were scored according to the method described by Schiantarelli et al[26] using the following scale: 0 = normal mucosa; 1 = hyperemic mucosa or up to 3 small patches; 2 = from 4 to 10 small patches; 3 = more than 10 small or up to 3 medium-sized patches; 4= from 4 to 6 medium-sized patches; 5 = more than 6 medium-sized or up to 3 large patches; 6 = from 4 to 6 large patches; 7 = from 7 to 10 large patches; 8 = more than 10 large patches or extensive necrotic zones. “small” was defined as up to 2 mm across (max diameter), “medium-sized” as between 2 and 4 mm across and “large” as more than 4 mm across.
Two separate batches of ethanol treated rats were used for biochemical and histological studies. The assay of gastric wall mucus, non-protein sulfhydryl group (NP-SH), and myeloperoxidase (MPO) in the rats 1 h after ethanol exposure has been described below:
Determination of gastric wall mucus: Gastric wall mucus was determined according to the modified procedure of Corne et al[27]. The glandular segment of the stomach was separated from the lumen of the stomach, weighed, and transferred immediately to 10 mL of 0.1% w/v Alcian blue solution (in 0.16 mol/L sucrose solution buffered with 0.05 mL sodium acetate at pH 5). Tissue was stained for two hours in Alcian blue, excess dye was removed by two successive rinses with 10 mL of 0.25 mol/L sucrose, first for 15 min and then for 45 min. Dye complexed with the gastric wall mucus was extracted with 10 mL of 0.5 mol/L magnesium chloride which was intermittently shaken for 1 min at 30 min intervals for 2 h. Four milliliters of blue extract was then vigorously shaken with an equal volume of diethyl ether. The resulting emulsion was centrifuged at 3600 g for 10 min and the absorbance of aqueous layer was recorded at 580 nm. The quantity of Alcian blue extracted per gram of wet glandular tissue was then calculated.
Estimation of NP-SH: Gastric mucosal NP-SH was measured according to the method of Sedlak and Lindsay[28]. The glandular part of stomach was homogenized in ice-cold 0.02 mmol/L ethylenediaminetetraacetic acid. Aliquots of 5 mL of the homogenates were mixed in 15 mL test tubes with 4 mL of distilled water and 1 mL of 50% trichloroacetic acid. The tubes were shaken intermittently for 10-15 min and centrifuged at 3000 g. Two milliliters of supernatant were mixed with 4 mL of 0.4 mol/L Tris buffer at pH 8.9; 0.1 mL of 5,5’-dithio-bis-(2-nitrobenzoic acid) (DTNB) was added and the sample was shaken. The absorbance was read within 5 min of addition of DTNB at 412 nm against a reagent blank with no homogenates.
Determination of MPO: MPO activity in the gastric mucosa was measured according to the methods described earlier[29]. Preweighed tissue was homogenized (1:10 wt/vol) in 0.5% hexadecyltrimethyl ammonium bromide in 50 mmol potassium phosphate buffer (pH 6.0) before sonication in an ice bath for 20 s. Three freeze/thaw cycles were performed followed by sonication (20 s in ice bath). The samples were centrifuged at 17000 g (5 min, 4 °C) and MPO in the supernatant was assayed by mixing of 0.1 mL of supernatant with 2.9 mL of 50 mmol/potassium phosphate buffer (pH 6.0) containing 0.167 g/L O-dianasidine dihydrochloride and 0.0005% hydrogen peroxide. The change in absorbance at 460 nm was measured for 4 min using ultraviolet (UV)-visible spectrophotometer (UV-160A, Shimadzu, Kyoto, Japan).
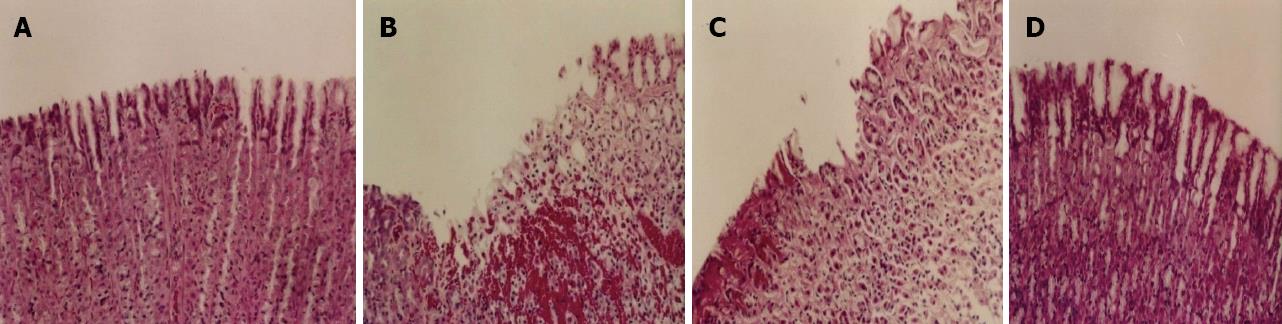
Histology of ethanol-induced gastric lesions: The stomach was opened along the greater curvature, washed with saline and fixed in 10% neutral buffered formalin for 24 h. The specimens were then processed overnight for dehydration and clearing steps, using an automatic tissue processor (Shandon Processor MKП; Runcorn. Cheshire, United Kingdom). The specimens were embedded in paraffin blocks and sections of 5 μm thickness were stained with hematoxylin-eosin for light microscopy observations.
Data were analyzed by one-way analysis of variance (ANOVA) followed by Dunnett’s multiple comparison test. Differences with P < 0.05 were considered as statistically significant.
In control rats pylorus ligation for 6 h resulted in the accumulation of 8.1 ± 0.61 mL of gastric secretion and total acid output of 498.7 ± 31.8 mEq (Table 1). The treatment of the rats with 100, 300 and 900 mg/kg of B-Hb produced a significant decrease in the volume of gastric secretion 5.6 ± 0.63, 5.5 ± 0.75 and 4.7 ± 0.58 mL respectively as compared to the control group. Treatment with B-Hb also dose dependently reduced total acid output in the rats treated with 100 mg/kg (471.1 ± 75 mEq) and 300 mg/kg (438.4 ± 65.6 mEq). However a significant reduction in total acid output was observed in a dose of 900 mg/kg (287.6 ± 24.6 mEq) of B-Hb.
The administration of indomethacin resulted in production of gastric lesions mainly in the glandular stomach of all the animals. The lesion area in the control group was found to be 22.4 ± 3.2 mm2. Pretreatment of rats with B-Hb at doses of 100 mg/kg (24.3 ± 3.29 mm2), 300 mg/kg (16.2 ± 1.45 mm2) and 900 mg/kg (12.6 ± 1.85 mm2) produced a dose dependent decrease of the lesion area (ANOVA F = 4.50, P < 0.05, Figure 1A).
The treatment of rats with absolute ethanol produced extensive gastric lesion in the glandular mucosa of the stomach. These lesions were characterized by multiple hemorrhagic red bands (patches) of different sizes along the axis of the glandular stomach. The ulcer index in the control group 1 h after ethanol administration was 7.1 ± 0.31. Pretreatment of rats with B-Hb at the doses of 100 mg/kg (ulcer index = 2.5 ± 0.42), 300 mg/kg (2.1 ± 0.4) and 900 mg/kg (0.7 ± 0.21) significantly inhibited the formation of gastric lesions (ANOVA F = 63.26, P < 0.0001, Figure 1B). Histological examination of gastric mucosa showed the appearance of these lesions in the form of gastric pits with detachment of the surface epithelium; vacuolation of epithelial cells and elongation of microvessels. Pretreatment with B-Hb dose-dependently prevented ethanol-induced mucosal damage (Figure 1).
The treatment of rats with ethanol significantly decreased the Alcian blue binding capacity of gastric wall mucus (480 ± 25.6 μg Alcian blue/g of tissue) as compared to control rats (667 ± 25.8 μg. Pretreatment of rats with B-Hb at the doses of 100 mg/kg (516 ± 31.6 μg/g), 300 mg/kg (558 ± 28.8 μg/g) and 900 mg/kg (654 ± 33.8 μg/g) significantly enhanced the binding capacity of Alcian blue to gastric mucosa (ANOVA F = 8.05, P < 0.005, Table 2).
| Treatment | Dose of B-Hb (mg/kg) | Alcian blue binding (mg/g tissue) | Non-protein sulfhydryl (mmol/g tissue) | Myeloperoxidase activity (DA/g tissue) |
| Control | 0 | 667 ± 25.8 | 4.59 ± 0.29 | 15.94 ± 1.6 |
| EtOH alone | 1 mL/animal | 480 ± 25.6b | 1.60 ± 0.12b | 24.54 ± 1.9b |
| EtOH ± B-Hb | 100 | 516 ± 31.6 | 3.11 ± 0.35d | 24.30 ± 4.2 |
| EtOH ± B-Hb | 300 | 558 ± 28.8d | 3.73 ± 0.42d | 14.25 ± 2.6c |
| EtOH ± B-Hb | 900 | 654 ± 33.8d | 5.36 ± 0.34d | 17.21 ± 0.98c |
The level of NP-SH in the gastric mucosa of control rats was 4.59 ± 0.29 μmol/g of tissue, which was significantly decreased to 1.60 ± 0.12 μmol/g of tissue following the administration of ethanol. A significant and dose dependent reversal of NP-SH was observed following administration of B-Hb in low (3.11 ± 0.35 mmol/g of tissue), medium (3.73 ± 0.42 mmol/g of tissue) and high dose (5.36 ± 0.34 mmol/g of tissue) (ANOVA F = 19.62, P < 0.001, Table 2).
The MPO activity in the normal gastric mucosa was 15.96 ± 1.9 mmol/g of wet tissue which increased significantly to 24.54 ± 1.9 mmol/g following ethanol administration. The MPO activity was slightly reduced to 24.30 ± 4.2 mmol/g in the rats treated with low dose of B-Hb prior to ethanol administration. However medium and high dose of B-Hb significantly reversed ethanol induced increase in MPO the value of MPO in these two groups being 14.25 ± 2.6 mmol/g and 17.21 ± 0.98 mmol/g respectively (ANOVA F = 3.21, P < 0.05, Table 2).
The result of this study showed a dose dependent reduction in the volume and acidity of gastric secretions following intra-gastric administration of B-Hb (Table 1). Our findings are supported by several earlier investigators who showed that gastric hemorrhage or intra-gastric administration of blood or blood products exerts inhibitory effect on gastric acid secretions[30-32]. As early as 1953, Chandler et al[33] reported that gastro-duodenal hemorrhage leads to a temporary absence of hydrochloric acid (achlorhydria) causing a significant decrease in gastric acid secretions. Fullarton et al[34] also showed that gastro-duodenal blood infusion significantly inhibits pentagastrin stimulated gastric acid and pepsin secretion. Paradoxically, intra-gastric blood/blood products including hemoglobin which constitute a protein meal instead of stimulating gastric secretions result in gastric antisecretory activity[35,36]. Gastric acid secretion is an elaborate and dynamic process that is regulated by neural (efferent and afferent), hormonal (e.g., gastrin), and paracrine (e.g., histamine, ghrelin, somatostatin) pathways as well as mechanical (e.g., distention) and chemical (e.g., amino acids) stimuli[31]. It has been suggested that intra-gastric blood induced increase in plasma gastric inhibitory polypeptide, secretin or glucogen may modulate gastric acid secretion in animals[32,34,37,38]. These mediators inhibit gastric acid secretions through somatostatin release[39-41]. However this hypothesis has been challenged by some other investigators[42].
Pretreatment of rats with B-Hb dose dependently ameliorated indomethacin-induced gastric mucosal damage (Figure 1). Protective effect of cell free hemoglobin has been reported against a variety of experimentally induced disease models including cardiac ischemic reperfusion injury[18,43,44], pancreatitis[45], renal injury[46] and neuronal injury[18,19,47-49]. The mechanism by which B-Hb exerts its protective effect against indomethacin induced gastropathy is far from clear. Indomethacin causes gastric mucosal damage via several mechanisms, including the impairment of the barrier properties of the mucosa, suppression of gastric prostaglandin synthesis, reduction of gastric mucosal blood flow and interference with the tissue repair mechanism[50]. The ability of non-steroidal anti-inflammatory drugs (NSAIDs) to reduce gastric mucosal blood flow has been recognized for several decades[9]. Prostaglandins (PGs) of the E and I series are potent vasodilators that are continuously produced by the vascular endothelium, inhibition of PG synthesis by NSAIDs lead to a reduced vascular tone and hypoxic injury[51]. Cell free hemoglobin is able to readily diffuse in the microcirculation and transport O2 to hypoxic tissue because of its high O2 affinity, low viscosity and small mean diameter as compared to red blood cells[52]. Once in microcirculation Hb offloads oxygen to the ischemic tissue, which is unlike the vasoconstrictive effect of Hb on large vessels[53-56]. Hence the mitigation of pathogen induced ischemic injury by CF-Hb may be attributed to its ability to transient oxygen delivery[13,57] and preservation of energy metabolism[58]. Moreover, the presence of acid in the lumen of the stomach also contributes to the pathogenesis of indomethacin -induced ulcers and bleeding, by impairing the restitution process, interfering with hemostasis and inactivating several growth factors that are important in mucosal defense and repair[9]. Our experiments using Shay rats model clearly showed an inhibition of gastric acid secretion following B-Hb administration (Table 1). Thus the reduction of acid content in stomach by B-Hb may to some extent contribute to its gastroprotective effect against indomethacin induced ulcers.
The oral administration of absolute ethanol produced significant ulcers in glandular part of gastric mucosa of rats (Figure 2). Our histopathological studies of gastric mucosa showed a significant loss of glandular cells, disruption of epithelium, sub mucosal edema and infiltration of neutrophils following ethanol administration (Figure 2). A significant decrease in Alcian blue binding capacity of gastric mucosa following exposure to ethanol (Table 2) clearly suggests depletion of mucosal gel lining adhering to the gastric surface which is considered the first line of defense in stomach against endogenous and exogenous ulcerogens[59]. Numerous mechanisms have been proposed to explain necrotizing agent induced gastropathy[60]. Besides the direct deleterious effect of ethanol on gastric tissues, disruption of mucosal barrier also results from mucosal capillary necrosis, vascular congestion and thrombosis in the sub-epithelial microvasculature[61]. Oral administration of ethanol results in low or no blood flow to the stomach leading to transient hypoxic mucosal damage[62]. It is well accepted that gastric mucosal protective mechanism largely depend on appropriate microcirculation which help to orchestrate the defense mechanism at various levels of gastric mucosa[63]. Pre-treatment of animal with B-Hb dose dependently attenuated ethanol induced gastric ulcer with almost complete protection in higher dose of 900 mg/kg body weight (Figure 2). The gastroprotective effect of B-Hb against ethanol induced ulcers may to some extent be attributed to its ability to inhibit gastric acid secretions and enhanced oxygen delivery as discussed earlier. Moreover the cytoprotective effect of B-Hb was accompanied by attenuation of ethanol-induced increase in MPO (a marker of neutrophil activity) in glandular tissue of stomach (Table 2). Neutrophils are the major inflammatory cell type infiltrating the injured mucosa following exposure to ethanol[64]. Strategies to counteract the infiltration and/or activation of neutrophils have been shown to protect animals against gastric ulcers[65,66]. Activated neutrophils injure the microvasculature via the release of oxygen derived free radicals (ODFR) and proteases[67,68]. We observed a significant decrease in gastric NP-SH following ethanol administration clearly suggesting a massive generation of ODFR in stomach (Table 2). Our findings are in agreement with earlier reports showing depletion of sulfhydryls in ethanol-induced gastric lesions[69,70]. The treatment of rats with glutathione depletors has been shown to significantly potentiate ulcerogen-induced gastric mucosal injury[71], whereas increase in mucosal NP-SH exerts a gastroprotective effect[72,73]. These findings suggest that gastroprotective effects of B-Hb may to extent be attributed to its antioxidant activity. Dual effect of Hb as prooxidant and antioxidant has been reported earlier[74,75]. In fact, more than 100 years ago Hb was shown to readily react with H2O2[76] and peroxidase activity of Hb has been reported as early as by Wu[77]. Thus the active site of hemeprotein in Hb share peroxide cleavage properties of peroxidase to present antioxidant activity[78]. On the other hand the oxidation of Hb generates potentially cytotoxic products such as ferryl heme intermediate (Fe4+), methemoglobin (Fe3+), hemichromes and free heme or iron[79,80]. Comproportionation of cytotoxic ferryl hemoglobin with oxyhemoglobin has been shown to result in antioxidant function in which ferryl heme intermediate is quenched and resultant methemoglobin is re-reduced by methemoglobin reductase[81]. Moreover there is strong evidence to suggest that Hb exerts its cytoprotective effect through adaptive cytoprotection. The presence of Hb in the tissue has been shown to induce heme oxygenase-1 (HO-1) the enzyme responsible for heme degradation[82]. Studies with HO-1 knock out mice have demonstrated that HO-1 ameliorates NSAIDs induced gastric tissue damage[83,84]. It has been shown that HO-1 exerts its cytoprotective action against necrotizing agents by scavenging the prooxidant heme which is a major hemoglobin degradation product[84,85]. To sum up it may be suggested that cytoprotective effect of B-Hb is complex and involve multiple mechanisms.
In conclusion our data show that B-Hb has significant anti-gastric acid secretory and gastroprotective activity. Further studies are warranted to determine the role of B-Hb in prophylaxis/treatment of gastric ulcer disease.
The authors are thankful to the Prince Sultan Military Medical City and the Medical Services Department of Ministry of Defense for their encouragement and support.
In the recent years, the treatment strategies for gastric ulcer diseases have significantly changed, mirroring the revolution in the understanding of its pathogenesis. Improved oxygenation in critically ischemic gastric mucosa has emerged as a method of choice to accelerate epithelization of erosive and ulcerative defects. Bovine hemoglobin (B-Hb) has been used in a wide range of applications including restoration of tissue oxygenation in ischemic condition.
Strategies to improve oxygen delivery to ischemic tissues could potentially protect gastric mucosa and other tissues from hypoxic injury. Cell free hemoglobin is able to readily diffuse in the microcirculation and transport O2 to hypoxic tissue because of its high O2 affinity, low viscosity and small diameter.
Recent studies showed protective effect of cell free hemoglobin against disease models of ischemic reperfusion injury including neuronal injury, nephropathy, pancreatitis and myocardial infarction. This study first time demonstrated anti-secretory and gastric antiulcer activity of B-Hb. The gastroprotective effect could be attributed to the ability of B-Hb to improve oxygenation, reduction of oxidative stress and lowering of neutrophil activity.
The result of this study suggests that bovine hemoglobin besides having significant anti-gastric acid secretory activity protects rats against ethanol and indomethamine induced gastric ulcers. B-Hb being animal protein can be safely explored clinically for the oral treatment of hyperacidity and gastric ulcer diseases.
Hb is the iron-containing oxygen-transport metalloprotein in red blood cells of all vertebrates. Hemoglobin is autonomous; it binds oxygen and release it without the need for any cofactor. Cell free Hb has been used for wide range of applications including enhanced oxygen delivery to ischemic tissue. Bovine hemoglobin is superior to autologous red blood cells in restoring tissue oxygen in ischemic conditions.
This is the first study showing antisecretory and gastric anti-ulcer activity of bovine hemoglobin. Reduction of oxidative stress and lowering of neutrophil activity might contribute to B-Hb induced gastroprotective effects. The results are valuable to explore pharmacological potential of B-Hb in a variety of ischemic/hypoxic conditions.
P- Reviewer Vorobjova T S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Valle JD. Peptic ulcer disease and related disorders. Harrison’s Principal of Internal Medicine. 17th ed. New York: McGraw Hill 2008; 1746-1762. [Cited in This Article: ] |
| 2. | Pai R, Ohta M, Itani RM, Sarfeh IJ, Tarnawski AS. Induction of mitogen-activated protein kinase signal transduction pathway during gastric ulcer healing in rats. Gastroenterology. 1998;114:706-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Johnson LR. Regulation of gastrointestinal mucosal growth. World J Surg. 1979;3:477-486. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Holzer P. Gastroduodenal mucosal defense: coordination by a network of messengers and mediators. Curr Opin Gastroenterol. 2001;17:489-496. [PubMed] [Cited in This Article: ] |
| 5. | Cheung LY, Chang N. The role of gastric mucosal blood flow and H+ back-diffusion in the pathogenesis of acute gastric erosions. J Surg Res. 1977;22:357-361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Ritchie WP, Shearburn EW. Influence of isoproterenol and cholestyramine on acute gastric mucosal ulcerogenesis. Gastroenterology. 1977;73:62-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 7. | Whittle BJ. Mechanisms underlying gastric mucosal damage induced by indomethacin and bile-salts, and the actions of prostaglandins. Br J Pharmacol. 1977;60:455-460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 8. | Konturek SJ, Konturek PC, Brzozowski T. Prostaglandins and ulcer healing. J Physiol Pharmacol. 2005;56 Suppl 5:5-31. [PubMed] [Cited in This Article: ] |
| 9. | Wallace JL. How do NSAIDs cause ulcer disease? Baillieres Best Pract Res Clin Gastroenterol. 2000;14:147-159. [PubMed] [Cited in This Article: ] |
| 10. | Rachmilewitz D, Karmeli F, Okon E, Rubenstein I, Better OS. Hyperbaric oxygen: a novel modality to ameliorate experimental colitis. Gut. 1998;43:512-518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Elizavetina GA, Vinnitskiĭ LI, Vorob’eva NT, Chorbinskaia SA, Izmalkova NM. Evaluation of the therapeutic effect of hyperbaric oxygenation and anginin in peptic ulcer. Ter Arkh. 1989;61:46-48. [PubMed] [Cited in This Article: ] |
| 12. | Guerrin F, Robin H, Gosselin B, Laspeyres M. Effects of oxygen and hyperbaric conditions on various types of experimental ulcers. Lille Med. 1976;21:662-667. [PubMed] [Cited in This Article: ] |
| 13. | Strate T, Mann O, Kleinhans H, Rusani S, Schneider C, Yekebas E, Freitag M, Standl T, Bloechle C, Izbicki JR. Microcirculatory function and tissue damage is improved after therapeutic injection of bovine hemoglobin in severe acute rodent pancreatitis. Pancreas. 2005;30:254-259. [PubMed] [Cited in This Article: ] |
| 14. | Chang TM. Artificial cells for cell and organ replacements. Artif Organs. 2004;28:265-270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 15. | Weed RI, REED CF, BERG G. Is hemoglobin an essential structural component of human erythrocyte membranes? J Clin Invest. 1963;42:581-588. [PubMed] [Cited in This Article: ] |
| 16. | Dominguez de Villota ED, Ruiz Carmona MT, Rubio JJ, de Andrés S. Equality of the in vivo and in vitro oxygen-binding capacity of haemoglobin in patients with severe respiratory disease. Br J Anaesth. 1981;53:1325-1328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Costanzo LS. Physiology. 4th ed. Hagerstown, MD, USA: Lippincott Williams and Wilkins 2007; . [Cited in This Article: ] |
| 18. | Wei L, Wu RB, Yang CM, Zheng SY, Yu XY. Cardioprotective effect of a hemoglobin-based oxygen carrier on cold ischemia/reperfusion injury. Cardiology. 2011;120:73-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 19. | Mito T, Nemoto M, Kwansa H, Sampei K, Habeeb M, Murphy SJ, Bucci E, Koehler RC. Decreased damage from transient focal cerebral ischemia by transfusion of zero-link hemoglobin polymers in mouse. Stroke. 2009;40:278-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Standl T, Horn P, Wilhelm S, Greim C, Freitag M, Freitag U, Sputtek A, Jacobs E, Schulte am Esch J. Bovine hemoglobin is more potent than autologous red blood cells in restoring muscular tissue oxygenation after profound isovolemic hemodilution in dogs. Can J Anesthesiol. 1996;43:714-723. [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 95] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Harringer W, Hodakowski GT, Svizzero T, Jacobs EE, Vlahakes GJ. Acute effects of massive transfusion of a bovine hemoglobin blood substitute in a canine model of hemorrhagic shock. Eur J Cardiothorac Surg. 1992;6:649-654; discussion 654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Shay H, Komarov SA, Fels SE, Merze D, Gruenstein H, Siplet H. A simple method for the uniform production of gastric ulceration in the rat. Gastroenterology. 1945;5:43-61. [Cited in This Article: ] |
| 23. | Bhargava KP, Gupta MB, Tangri KK. Mechanism of ulcerogenic activity of indomethacin and oxyphenbutazone. Eur J Pharmacol. 1973;22:191-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 87] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Valcavi U, Caponi R, Brambilla A, Palmira M, Minoja F, Bernini F, Musanti R, Fumagalli R. Gastric antisecretory, antiulcer and cytoprotective properties of 9-hydroxy-19,20-bis-nor-prostanoic acid in experimental animals. Arzneimittelforschung. 1982;32:657-663. [PubMed] [Cited in This Article: ] |
| 25. | Natale G, Lazzeri G, Blandizzi C, Gherardi G, Lenzi P, Pellegrini A, Del Tacca M. Seriate histomorphometry of whole rat stomach: an accurate and reliable method for quantitative analysis of mucosal damage. Toxicol Appl Pharmacol. 2001;174:17-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Schiantarelli P, Cadel S, Folco GC. Gastroprotective effects of morniflumate, an esterified anti-inflammatory drug. Arzneimittelforschung. 1984;34:885-890. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 27. | Corne SJ, Morrissey SM, Woods RJ. Proceedings: A method for the quantitative estimation of gastric barrier mucus. J Physiol. 1974;242:116P-117P. [PubMed] [Cited in This Article: ] |
| 28. | Chien CP. Clinical trial of SK& amp; F 14336 concentrate for chronic psychotics. Curr Ther Res Clin Exp. 1969;11:15-21. [PubMed] [Cited in This Article: ] |
| 29. | Bradley PP, Priebat DA, Christensen RD, Rothstein G. Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol. 1982;78:206-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2502] [Cited by in F6Publishing: 2598] [Article Influence: 61.9] [Reference Citation Analysis (0)] |
| 30. | Zebrowska T, Low AG, Zebrowska H. Studies on gastric digestion of protein and carbohydrate, gastric secretion and exocrine pancreatic secretion in the growing pig. Br J Nutr. 1983;49:401-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 130] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Schubert ML. Gastric secretion. Curr Opin Gastroenterol. 2007;23:595-601. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Fullarton GM, Boyd EJ, Crean GP, Hilditch TE, McColl KE. Effect of simulated intragastric haemorrhage on gastric acid secretion, gastric motility, and serum gastrin. Gut. 1990;31:518-521. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Chandler GN, Watkinson G. Gastric aspiration in haematemesis. Lancet. 1953;265:1170-1175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Fullarton GM, Boyd EJ, Crean GP, Buchanan K, McColl KE. Inhibition of gastric secretion and motility by simulated upper gastrointestinal haemorrhage: a response to facilitate haemostasis? Gut. 1989;30:156-160. [PubMed] [Cited in This Article: ] |
| 35. | Schubert ML. Gastric secretion. Curr Opin Gastroenterol. 2011;27:536-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Ramsay PT, Carr A. Gastric acid and digestive physiology. Surg Clin North Am. 2011;91:977-982. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Bell FR, Webber DE, Wass JA, Rees LH, Evans J, Morgan LM, Marks V, Lewis J. Correlation of endogenous somatostatin, gastric inhibitory polypeptide, glucagon and insulin with gastric function in the conscious calf. J Endocrinol. 1981;89:451-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Allison MC, Fullarton GM, Brown IL, Crean GP, McColl KE. Enhanced gastric mucosal haemostasis after upper gastrointestinal haemorrhage. Gut. 1991;32:735-739. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Chiba T, Taminato T, Kadowaki S, Abe H, Chihara K, Seino Y, Matsukura S, Fujita T. Effects of glucagon, secretin, and vasoactive intestinal polypeptide on gastric somatostatin and gastrin release from isolated perfused rat stomach. Gastroenterology. 1980;79:67-71. [PubMed] [Cited in This Article: ] |
| 40. | McIntosh CH, Pederson RA, Koop H, Brown JC. Gastric inhibitory polypeptide stimulated secretion of somatostatinlike immunoreactivity from the stomach: inhibition by acetylcholine or vagal stimulation. Can J Physiol Pharmacol. 1981;59:468-472. [PubMed] [Cited in This Article: ] |
| 41. | Wolfe MM, Reel GM, McGuigan JE. Inhibition of gastrin release by secretin is mediated by somatostatin in cultured rat antral mucosa. J Clin Invest. 1983;72:1586-1593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 42. | Konturek SJ, Tasler J, Cieszkowski M, Coy DH, Schally AV. Effect of growth hormone release-inhibiting hormone on gastric secretion, mucosal blood flow, and serum gastrin. Gastroenterology. 1976;70:737-741. [PubMed] [Cited in This Article: ] |
| 43. | Li T, Li J, Liu J, Zhang P, Wu W, Zhou R, Li G, Zhang W, Yi M, Huang H. Polymerized placenta hemoglobin attenuates ischemia/reperfusion injury and restores the nitroso-redox balance in isolated rat heart. Free Radic Biol Med. 2009;46:397-405. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Rempf C, Standl T, Schenke K, Chammas K, Gottschalk A, Burmeister MA, Gottschalk A. Administration of bovine polymerized haemoglobin before and during coronary occlusion reduces infarct size in rabbits. Br J Anaesth. 2009;103:496-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 45. | Strate T, Mann O, Kleinhans H, Schneider C, Knoefel WT, Yekebas E, Standl T, Bloechle C, Izbicki JR. Systemic intravenous infusion of bovine hemoglobin significantly reduces microcirculatory dysfunction in experimentally induced pancreatitis in the rat. Ann Surg. 2003;238:765-771. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Whitley D, Patterson R, Greenburg AG. Cell-free hemoglobin preserves renal function during normothermic ischemia. J Surg Res. 1998;77:187-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Burmeister MA, Rempf C, Standl TG, Rehberg S, Bartsch-Zwemke S, Krause T, Tuszynski S, Gottschalk A, Schulte am Esch J. Effects of prophylactic or therapeutic application of bovine haemoglobin HBOC-200 on ischaemia-reperfusion injury following acute coronary ligature in rats. Br J Anaesth. 2005;95:737-745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 48. | Caswell JE, Strange MB, Rimmer DM, Gibson MF, Cole P, Lefer DJ. A novel hemoglobin-based blood substitute protects against myocardial reperfusion injury. Am J Physiol Heart Circ Physiol. 2005;288:H1796-H1801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 49. | Nemoto M, Mito T, Brinigar WS, Fronticelli C, Koehler RC. Salvage of focal cerebral ischemic damage by transfusion of high O2-affinity recombinant hemoglobin polymers in mouse. J Appl Physiol. 2006;100:1688-1691. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Fromm D. How do non-steroidal anti-inflammatory drugs affect gastric mucosal defenses? Clin Invest Med. 1987;10:251-258. [PubMed] [Cited in This Article: ] |
| 51. | Rainsford KD. Microvascular injury during gastric mucosal damage by anti-inflammatory drugs in pigs and rats. Agents Actions. 1983;13:457-460. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Creteur J, Vincent JL. Potential uses of hemoglobin-based oxygen carriers in critical care medicine. Crit Care Clin. 2009;25:311-324, Table of Contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Gulati A, Sharma AC, Burhop KE. Effect of stroma-free hemoglobin and diaspirin cross-linked hemoglobin on the regional circulation and systemic hemodynamics. Life Sci. 1994;55:827-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 60] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 54. | Federspiel WJ. Pulmonary diffusing capacity: implications of two-phase blood flow in capillaries. Respir Physiol. 1989;77:119-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | Page TC, Light WR, McKay CB, Hellums JD. Oxygen transport by erythrocyte/hemoglobin solution mixtures in an in vitro capillary as a model of hemoglobin-based oxygen carrier performance. Microvasc Res. 1998;55:54-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 115] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 56. | George I, Yi GH, Schulman AR, Morrow BT, Cheng Y, Gu A, Zhang G, Oz MC, Burkhoff D, Wang J. A polymerized bovine hemoglobin oxygen carrier preserves regional myocardial function and reduces infarct size after acute myocardial ischemia. Am J Physiol Heart Circ Physiol. 2006;291:H1126-H1137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 57. | Plock JA, Rafatmehr N, Sinovcic D, Schnider J, Sakai H, Tsuchida E, Banic A, Erni D. Hemoglobin vesicles improve wound healing and tissue survival in critically ischemic skin in mice. Am J Physiol Heart Circ Physiol. 2009;297:H905-H910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 58. | Carlucci F, Miraldi F, Barretta A, Marullo AG, Marinello E, Tabucchi A. Preservation of myocardial energy status by bovine hemoglobin solutions during ischemia. Biomed Pharmacother. 2002;56:247-253. [PubMed] [Cited in This Article: ] |
| 59. | Slomiany BL, Piasek A, Sarosiek J, Slomiany A. The role of surface and intracellular mucus in gastric mucosal protection against hydrogen ion. Compositional differences. Scand J Gastroenterol. 1985;20:1191-1196. [PubMed] [Cited in This Article: ] |
| 60. | Amandeep K, Robin S, Ramica S, Sunil K. Peptic ulcer: A review on etiology and pathogenesis. IRJP. 2012;3:34-38. [Cited in This Article: ] |
| 61. | Konturek SJ, Stachura J, Konturek JW. Gastric cytoprotection and adaptation to ethanol. Alcohol and the gastrointestinal tract. New York: CRC Press 1996; 123-141. [Cited in This Article: ] |
| 62. | Saeki T, Takahashi N, Kanamoto R, Iwami K. Characterization of cloned mouse Na+/taurocholate cotransporting polypeptide by transient expression in COS-7 cells. Biosci Biotechnol Biochem. 2002;66:1116-1118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Holzer P, Lippe IT. Stimulation of afferent nerve endings by intragastric capsaicin protects against ethanol-induced damage of gastric mucosa. Neuroscience. 1988;27:981-987. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 173] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 64. | Laine L, Weinstein WM. Histology of alcoholic hemorrhagic “gastritis”: a prospective evaluation. Gastroenterology. 1988;94:1254-1262. [PubMed] [Cited in This Article: ] |
| 65. | Shimizu N, Watanabe T, Arakawa T, Fujiwara Y, Higuchi K, Kuroki T. Pentoxifylline accelerates gastric ulcer healing in rats: roles of tumor necrosis factor alpha and neutrophils during the early phase of ulcer healing. Digestion. 2000;61:157-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 66. | Kvietys PR, Twohig B, Danzell J, Specian RD. Ethanol-induced injury to the rat gastric mucosa. Role of neutrophils and xanthine oxidase-derived radicals. Gastroenterology. 1990;98:909-920. [PubMed] [Cited in This Article: ] |
| 67. | Elsbach P, Weiss J. Phagocytosis of bacteria and phospholipid degradation. Biochim Biophys Acta. 1988;947:29-52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 50] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 68. | Hernandez LA, Grisham MB, Twohig B. Arfors KE, Harlan JM, Granger DN. Role of neutrophils in ischemia-reperfusion induced microvascular injury. Am J Physiol. 1987;253:H699-H703. [Cited in This Article: ] |
| 69. | Miller TA, Li D, Kuo YJ, Schmidt KL, Shanbour LL. Nonprotein sulfhydryl compounds in canine gastric mucosa: effects of PGE2 and ethanol. Am J Physiol. 1985;249:G137-G144. [PubMed] [Cited in This Article: ] |
| 70. | La Casa C, Villegas I, Alarcón de la Lastra C, Motilva V, Martín Calero MJ. Evidence for protective and antioxidant properties of rutin, a natural flavone, against ethanol induced gastric lesions. J Ethnopharmacol. 2000;71:45-53. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 370] [Cited by in F6Publishing: 350] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 71. | Hiraishi H, Terano A, Ota S, Mutoh H, Sugimoto T, Harada T, Razandi M, Ivey KJ. Protection of cultured rat gastric cells against oxidant-induced damage by exogenous glutathione. Gastroenterology. 1994;106:1199-1207. [PubMed] [Cited in This Article: ] |
| 72. | Sener-Muratoğlu G, Paskaloğlu K, Arbak S, Hürdağ C, Ayanoğlu-Dülger G. Protective effect of famotidine, omeprazole, and melatonin against acetylsalicylic acid-induced gastric damage in rats. Dig Dis Sci. 2001;46:318-330. [PubMed] [Cited in This Article: ] |
| 73. | Hernández-Muñoz R, Montiel-Ruíz C, Vázquez-Martínez O. Gastric mucosal cell proliferation in ethanol-induced chronic mucosal injury is related to oxidative stress and lipid peroxidation in rats. Lab Invest. 2000;80:1161-1169. [PubMed] [Cited in This Article: ] |
| 74. | Lu N, Chen W, Peng YY. Effects of glutathione, Trolox and desferrioxamine on hemoglobin-induced protein oxidative damage: anti-oxidant or pro-oxidant? Eur J Pharmacol. 2011;659:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 75. | Alayash AI. Oxidative mechanisms of hemoglobin-based blood substitutes. Artif Cells Blood Substit Immobil Biotechnol. 2001;29:415-425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 76. | Kobert R. Beitrage zur Kenntniss der Methamoglobine. Pflugers Arch. Gesamte Physiol. Menschen Tiere. 1900;82:603-630. [Cited in This Article: ] |
| 77. | Wu H. Studies on hemoglobin. III. An ultra-micro-method for the determination of hemoglobin as a peroxidase. J Biochem. 1923;2:189-194. [Cited in This Article: ] |
| 78. | Allentoff AJ, Bolton JL, Wils A, Thompson JA, Ortiz de Montellano PR. Heterolytic versus hemolytic peroxide bond cleavage by sperm whale myoglobin and myoglobin mutants. J Am Chem Soc. 1992;114:9744-9749. [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 79. | Gutteridge JM. Iron promoters of the Fenton reaction and lipid peroxidation can be released from haemoglobin by peroxides. FEBS Lett. 1986;201:291-295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 475] [Cited by in F6Publishing: 501] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 80. | Giulivi C, Cadenas E. Heme protein radicals: formation, fate, and biological consequences. Free Radic Biol Med. 1998;24:269-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 102] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 81. | Giulivi C, Davies KJ. A novel antioxidant role for hemoglobin. The comproportionation of ferrylhemoglobin with oxyhemoglobin. J Biol Chem. 1990;265:19453-19460. [PubMed] [Cited in This Article: ] |
| 82. | D’Agnillo F, Alayash AI. Interactions of hemoglobin with hydrogen peroxide alters thiol levels and course of endothelial cell death. Am J Physiol Heart Circ Physiol. 2000;279:H1880-H1889. [PubMed] [Cited in This Article: ] |
| 83. | Kapturczak MH, Wasserfall C, Brusko T, Campbell-Thompson M, Ellis TM, Atkinson MA, Agarwal A. Heme oxygenase-1 modulates early inflammatory responses: evidence from the heme oxygenase-1-deficient mouse. Am J Pathol. 2004;165:1045-1053. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 327] [Cited by in F6Publishing: 341] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 84. | Nath KA, Haggard JJ, Croatt AJ, Grande JP, Poss KD, Alam J. The indispensability of heme oxygenase-1 in protecting against acute heme protein-induced toxicity in vivo. Am J Pathol. 2000;156:1527-1535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 219] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 85. | Ueda K, Ueyama T, Yoshida K, Kimura H, Ito T, Shimizu Y, Oka M, Tsuruo Y, Ichinose M. Adaptive HNE-Nrf2-HO-1 pathway against oxidative stress is associated with acute gastric mucosal lesions. Am J Physiol Gastrointest Liver Physiol. 2008;295:G460-G469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 234] [Article Influence: 14.6] [Reference Citation Analysis (0)] |