Published online May 26, 2013. doi: 10.13105/wjma.v1.i1.8
Revised: February 22, 2013
Accepted: March 6, 2013
Published online: May 26, 2013
Processing time: 113 Days and 18 Hours
Tuberculosis (TB) is an infection caused by Mycobacterium tuberculosis and is one of the world’s deadliest diseases. Multidrug resistant TB (MDR-TB) is a serious form of TB and it implies resistance for at least two essential first-line agents like, Isoniazid and Rifampicin. The US Food and Drug Administration (FDA) granted accelerated approval to Janseen Therapeutics “Sirturo (Bedaquiline)”, a diarylquinoline anti mycobacterial drug on December 28, 2012 as part of combination therapy in adults (≥ 18 years) to treat MDR-TB when other alternatives are not available. The FDA also granted Sirturo fast track designation, priority review and orphan-product designation. Bedaquiline inhibits mycobacterial ATP (adenosine 5’-triphosphate) synthase, an enzyme that is essential for the generation of energy in Mycobacterium tuberculosis.
Core tip: The US Food and Drug Administration granted accelerated approval to Janseen Therapeutics “Sirturo (Bedaquiline)”, a diarylquinoline anti mycobacterial drug on December 28, 2012 as part of combination therapy in adults (≥ 18 years) to treat multidrug resistant tuberculosis when other alternatives are not available.
- Citation: Undela K. Sirturo (Bedaquiline): The first new anti tubercular drug in decades. World J Meta-Anal 2013; 1(1): 8-9
- URL: https://www.wjgnet.com/2308-3840/full/v1/i1/8.htm
- DOI: https://dx.doi.org/10.13105/wjma.v1.i1.8
Tuberculosis (TB) is an infection caused by Mycobacterium tuberculosis and is one of the world’s deadliest diseases. According to the Centers for Disease Control and Prevention, nearly 9 million people around the world and 10528 people in the United States became sick with TB in 2011.
Multidrug resistant TB (MDR-TB) is a serious form of TB and it implies resistance for at least two essential first-line agents, like Isoniazid and Rifampicin. MDR-TB is a possibly fatal disease that affects as many as 630000 people worldwide who cannot be cured with existing therapies alone and it is considered an orphan disease in the US, with 98 reported patients in 2011. The World Health Organisation estimates more than two million people will develop MDR-TB between 2011 and 2015.
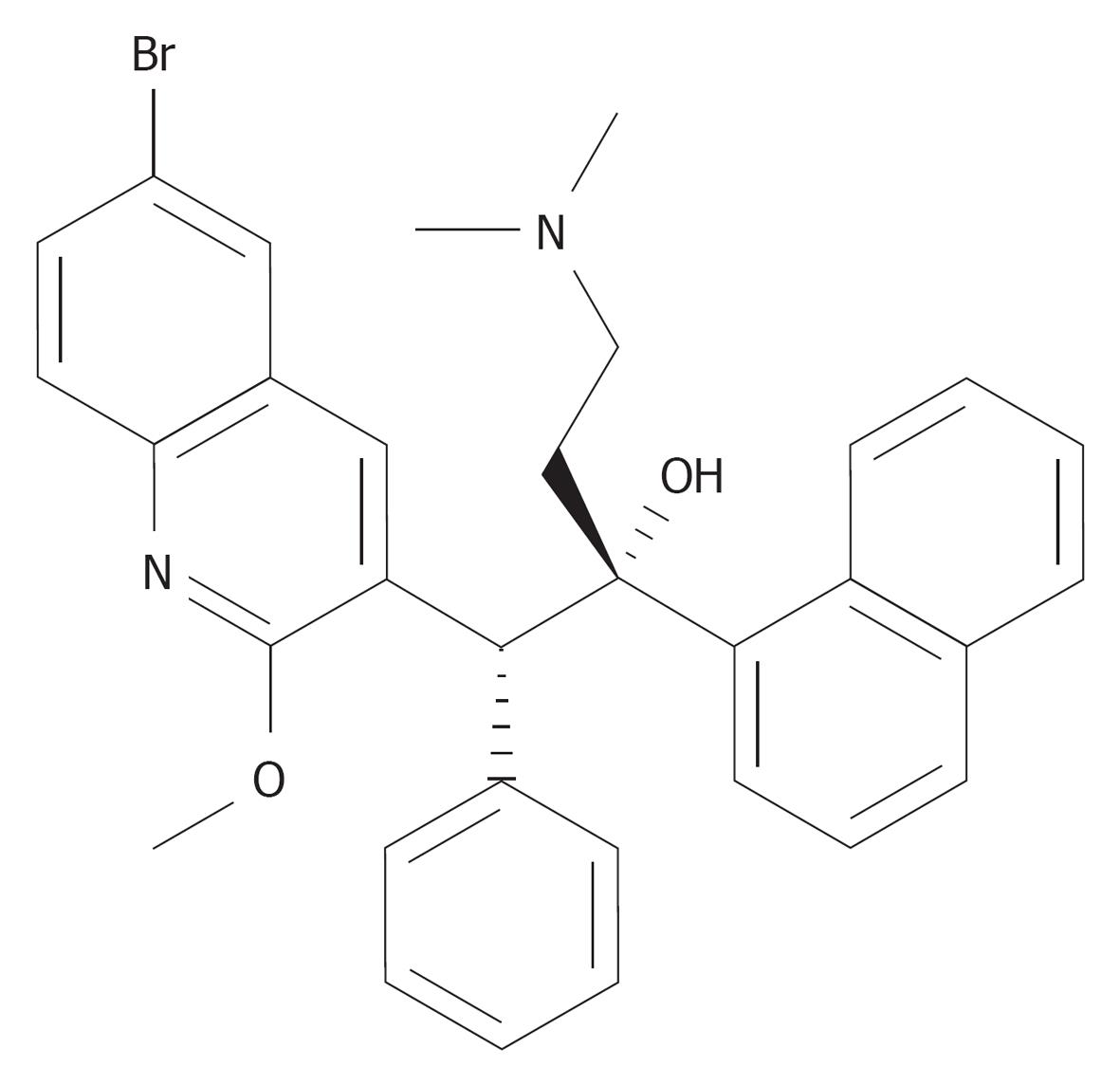
The US Food and Drug Administration (FDA) granted accelerated approval to Janseen Therapeutics “Sirturo (Bedaquiline)”[1], a diarylquinoline anti mycobacterial drug on December 28, 2012 as part of combination therapy in adults (≥ 18 years) to treat MDR-TB when other alternatives are not available and it leads to the approval of the first TB therapy in 40 years with a new mechanism of action. The FDA also granted Sirturo fast track designation, priority review and orphan-product designation (Figure 1)[2].
Bedaquiline inhibits mycobacterial ATP (adenosine 5’-triphosphate) synthase, an enzyme that is essential for the generation of energy in Mycobacterium tuberculosis.
Mycobacterial resistance mechanisms that affect Bedaquiline include modification of the atpE target gene. Not all isolates with increased minimum inhibitory concentrations have atpE mutations, suggesting the existence of at least one other mechanism of resistance.
Bedaquiline has been shown to be active against most isolates of Mycobacterium tuberculosis.
Bedaquiline’s safety and effectiveness were established in 440 patients in two phase 2 clinical trials. Patients in the first trial were randomly assigned to be treated with Sirturo plus other drugs used to treat MDR-TB (Sirturo treatment group) (n = 79), or a placebo plus other drugs used to treat MDR-TB (placebo treatment group) (n = 81); the other drugs used to treat MDR-TB consisted of a combination of five other antimycobacterial drugs (ethionamide, kanamycin, pyrazinamide, ofloxacin and cycloserine/terizidone or available alternative). Sirturo was administered as 400 mg once daily for the first 2 wk and as 200 mg three times per week for the following 22 wk. After the 24 wk study drug (Sirturo or placebo) treatment phase, patients continued to receive their other drugs used to treat MDR-TB until total treatment duration of 18 to 24 mo was achieved, or at least 12 mo after the first confirmed negative culture. All patients in the second trial, which is ongoing, received Sirturo plus other MDR-TB drugs. In both studies, the primary endpoint was time to sputum culture conversion (SCC), defined as the interval in days between the first dose of the study drug and the date of the first of two consecutive negative sputum cultures collected at least 25 d apart during treatment.
Results from the first trial showed that patients treated with Sirturo combination therapy achieved SCC in a median time of 83 d, compared with 125 d in patients treated with placebo combination therapy. According to these results, 77.6% of patients in the treatment group reached treatment success after 24 wk compared with 57.6% of those in the placebo group. Results from the second trial showed the median time to SCC was 57 d, supporting the efficacy findings of the first trial.
Sirturo carries a boxed warning, alerting patients and health care professionals that the drug can affect the heart’s electrical activity (QT prolongation) and also notes that an increased risk of death was seen in the Sirturo treatment group (9/79, 11.4%) compared to the placebo treatment group (2/81, 2.5%) in one placebo-controlled trial. Sirturo should only be used when an effective treatment regimen cannot otherwise be provided.
The most common adverse reactions reported in > 10% of patients treated with Sirturo are nausea, arthralgia and headache. Additional adverse events reported in ≥ 10% of patients treated with Sirturo and with a higher frequency than the placebo treatment group are hemoptysis and chest pain. More hepatic-related adverse drug reactions were reported with the use of Sirturo plus other drugs used to treat TB compared to other drugs used to treat TB without the addition of Sirturo.
The safety and efficacy of Sirturo for the treatment of drug-sensitive TB has not been established. In addition, there is no data on the treatment with Sirturo of extra-pulmonary TB (e.g., central nervous system).
Sirturo was discovered by researchers at “Janssen” and is currently under review by three regulatory bodies, including the European Medicines Agency (European Union), State Food and Drug Administration (China) and Medicines Control Council (South Africa).
P- Reviewer Ray S S- Editor Gou SX L- Editor Roemmele A E- Editor Zheng XM
| 1. | Diacon AH, Donald PR, Pym A, Grobusch M, Patientia RF, Mahanyele R, Bantubani N, Narasimooloo R, De Marez T, van Heeswijk R. Randomized pilot trial of eight weeks of bedaquiline (TMC207) treatment for multidrug-resistant tuberculosis: long-term outcome, tolerability, and effect on emergence of drug resistance. Antimicrob Agents Chemother. 2012;56:3271-3276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 285] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 2. | US Food Drug Administration. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/204384s000lbl.pdf. |