Copyright
©The Author(s) 2016.
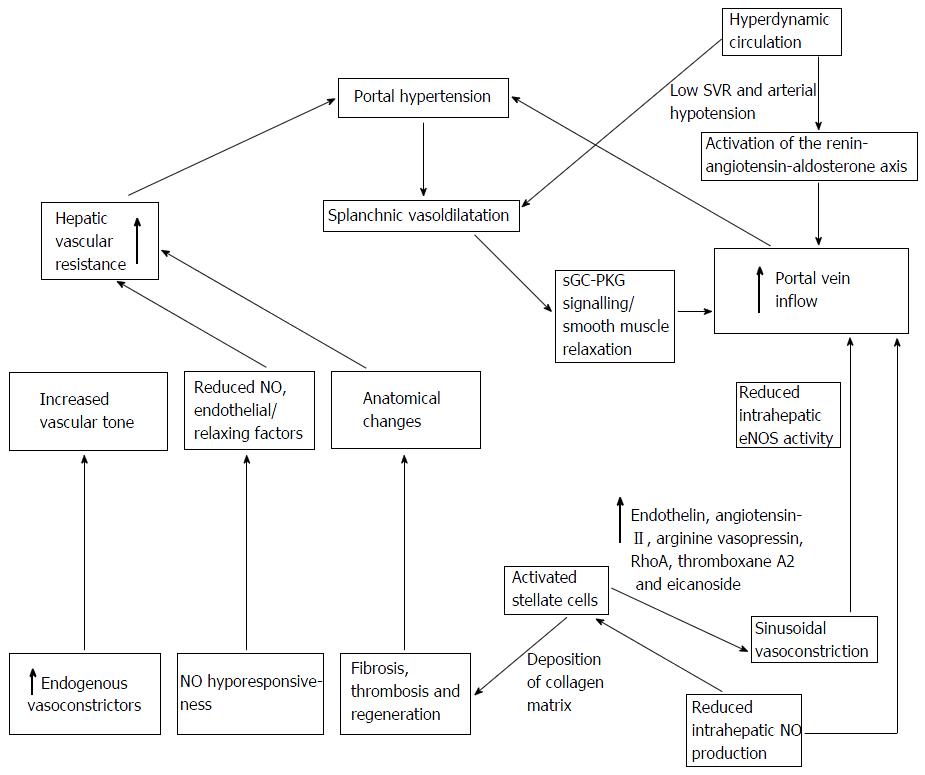
Figure 1 Factors involved in the pathogenesis of portal hypertension.
A mechanical obstruction due to fibrosis or regenerative nodules results increased resistance to flow and a rise in hepatic vascular resistance. Contraction of sinusoidal and extra sinusoidal contractile cells (stellate cells) with intrahepatic imbalance between vasoconstrictors (such as endothelin-1 and angiotensin) and vasodilators (e.g., NO) leads to reduced intrahepatic eNOS activity leading to an increase resistance to portal inflow. Portosystemic collaterals develop with the aim of decompressing the portal circulation. However, the opposite occurs, with splanchnic vasodilatation in response to a relatively ischaemic liver or extrahepatic excess of NO, with sGC-PKG signalling and smooth muscle cell relaxation. The increased portal blood flow maintains portal hypertension. A hyperdynamic circulation results due to these haemodynamic changes in cirrhosis and portal hypertension. eNOS: Endothelial nitric oxide synthase; NO: Nitric oxide; SVR: Systemic vascular resistance; sGC-PKG: Soluble guanylyl cyclase-cGMP-dependent protein kinase.
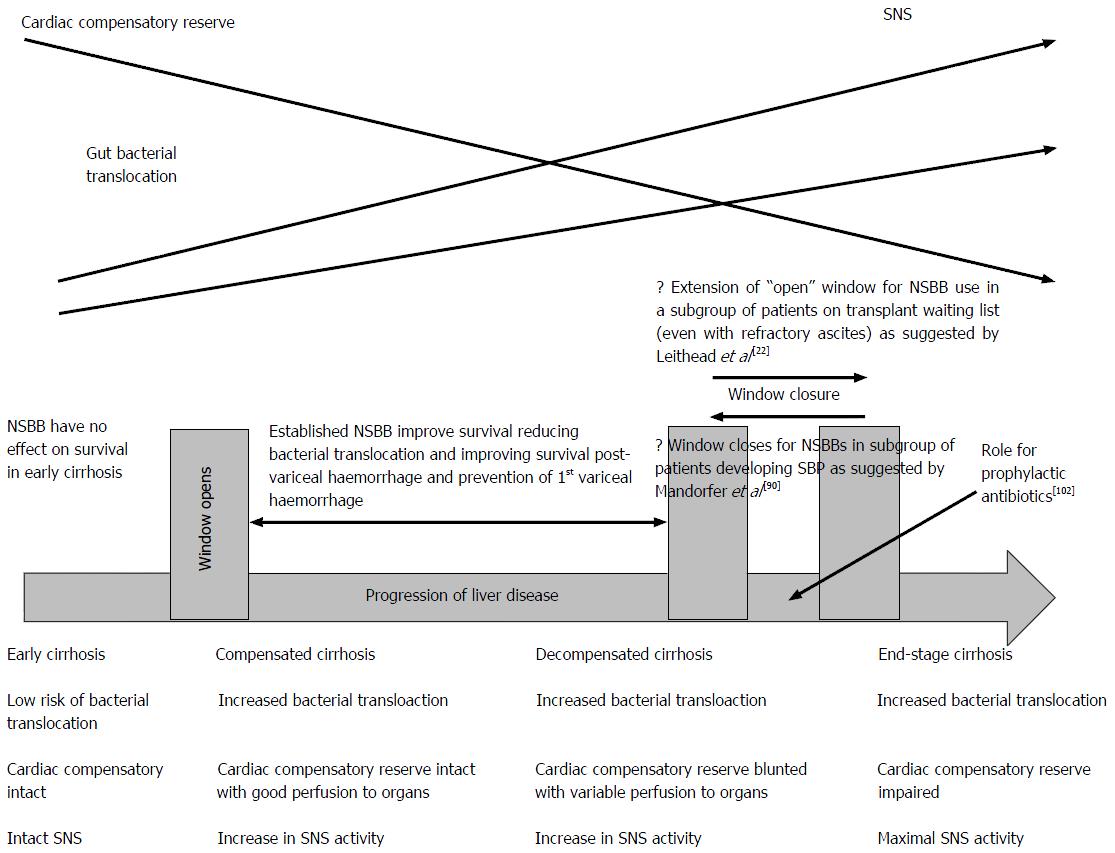
Figure 2 Extended - “window hypothesis” adapted and revised from Krag et al[21].
The window hypothesis illustrates that in early portal hypertension when low risk of bacterial translocation and adequate cardiac compensatory reserve, NSBBs have no effect on survival[25,67]. As disease progresses and varices enlarge there is clear benefit of NSBB in primary and secondary prophylaxis in improving mortality and also reducing rebleeding rates. The original widow hypothesis[21] commented that the window for benefit of NSBBs then may indeed close in decompensated cirrhosis (e.g., patients with refractory ascites[20]) however the data from Leithead et al[22] would suggest the window may indeed remain open even in such patients for a period of time. This window however may indeed close once patients have developed an episode of SBP[90]. SNS: Sympathetic nervous system activity; NSBB: Non-selective beta-blocker; SBP: Spontaneous bacterial peritonitis.
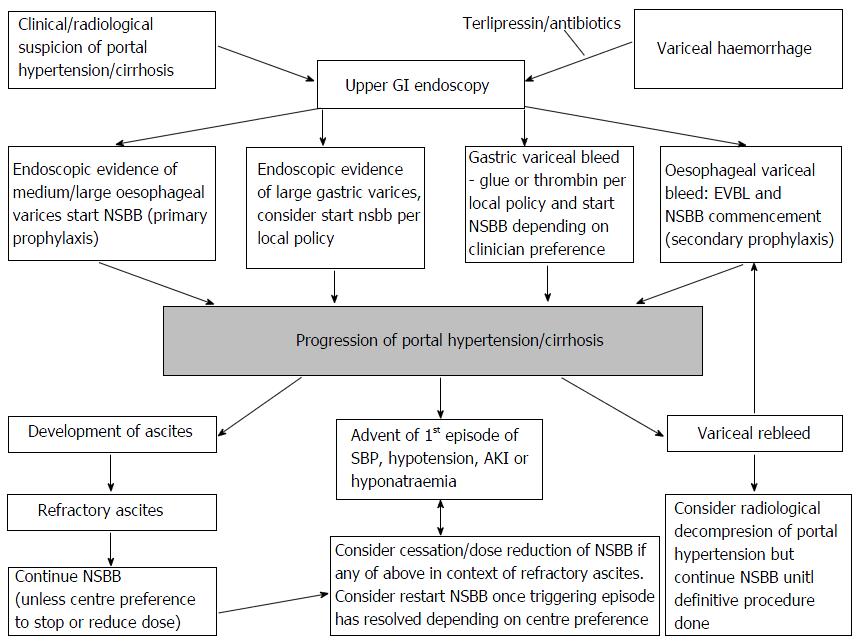
Figure 3 Proposed algorithm of Non-selective beta-blocker usage based on current guidelines and recent papers.
NSBB: Non-selective beta-blocker; GI: Gastrointestinal; SBP: Spontaneous bacterial peritonitis.
- Citation: Rajoriya N, Tripathi D. Non-selective beta-blockers in cirrhosis: Current concepts and controversies. World J Pharmacol 2016; 5(1): 15-31
- URL: https://www.wjgnet.com/2220-3192/full/v5/i1/15.htm
- DOI: https://dx.doi.org/10.5497/wjp.v5.i1.15