Copyright
©The Author(s) 2015.
World J Pharmacol. Mar 9, 2015; 4(1): 96-116
Published online Mar 9, 2015. doi: 10.5497/wjp.v4.i1.96
Published online Mar 9, 2015. doi: 10.5497/wjp.v4.i1.96
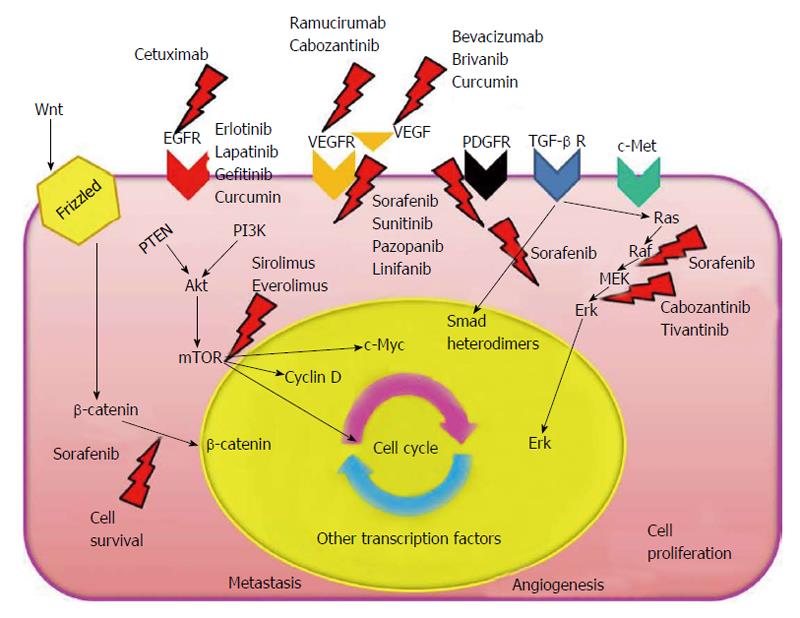
Figure 1 Hepatocellular carcinoma pathogenetic pathways.
Main molecular targets of the major anti-tumoral drugs are indicated. VEGF: Vascular endothelial growth factor; VEGFR: Vascular endothelial growth factor receptors; TGF-β: Transforming growth factor-β; Erk: Extracellular signal-regulated kinase; EGFR: Epidermal growth factor receptors; PDGFR: Platelet-derived growth factor receptors; TGF-β R: TGF-β receptor; RAS: Rat Sarcoma; RAF: Rapidly accelerated fibrosarcoma; MEK: Mitogen-activated protein kinase kinase; c-Myc: Myelocytomatosis cellular oncogene; PTEN: Phosphatase and tensin homology; PI3K: Phosphoinositide 3-kinase.
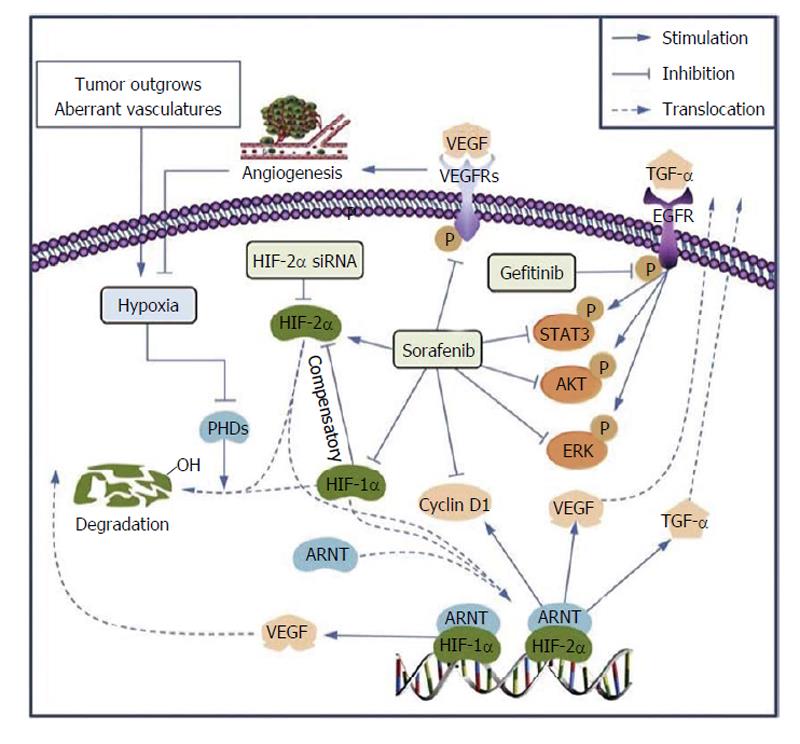
Figure 2 Proposed mechanisms by which upregulation of hypoxia-inducible factor-2α induced by sorafenib contributes to the resistance by activating the transforming growth factor-α/epidermal growth factor receptors pathway in hepatocellular carcinoma cells.
ARNT: Aryl hydrocarbon receptor nuclear translocator; EGFR: Epidermal growth factor receptor; ERK: Extracellular signal-regulated kinase; HIF-1α: Hypoxia-inducible factor-1α; HIF-2α: Hypoxia-inducible factor-2α; PHD: Prolyl hydroxylase; STAT3: Signal transducer and activator of transcription 3; TGF-α: Transforming growth factor-α; VEGF: Vascular endothelial growth factor; VEGFR: Vascular endothelial growth factor receptor. Reprinted from ref. [100] with permission from Elsevier.
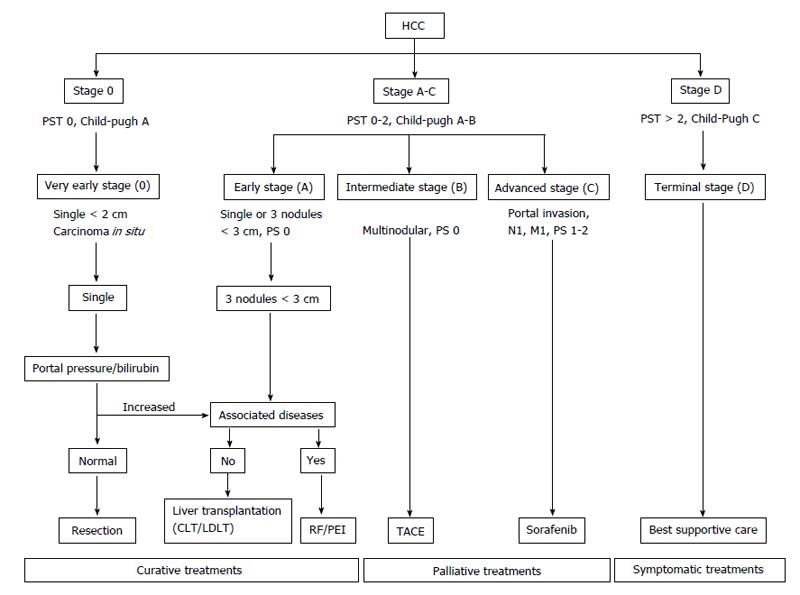
Figure 3 Barcelona Clinic Liver Cancer staging system and treatment strategy (2011).
HCC: Hepatocellular carcinoma; CLT: Cadaveric liver tansplantation; LDLT: Living donor transplantation; RF: Radiofrequency; PEI: Percutaneous ethanol injection; TACE: Transarterial chemoembolization; PST: Performance status test; PS: Performance status.
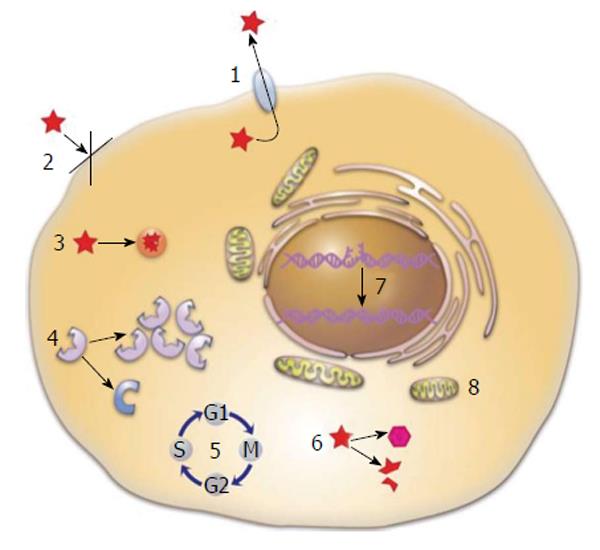
Figure 4 Mechanisms of multidrug resistance in cancer cells.
(1) Active drug efflux by drug transporters, such as Pgp, multidrug resistance-associated protein, and breast cancer resistance protein; (2) Loss of cell surface receptors and/or drug transporters or alterations in membrane lipid composition; (3) Compartmentalization of the drug in cellular vesicles; (4) Altered/increased drug targets; (5) Alterations in cell cycle; (6) Increased drug metabolism/enzymatic inactivation; (7) Active damage repair; and (8) Inhibition of apoptosis. Reprinted with permission from ref. [181].
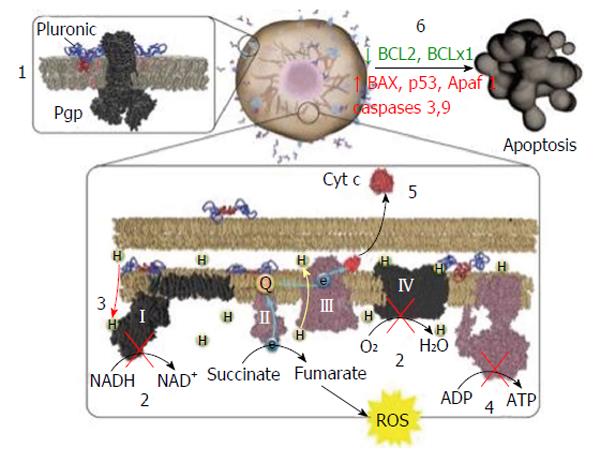
Figure 5 Summary of Pluronic effects in cancer cells.
Pluronic binding with plasma membrane of multidrug resistance (MDR) cancer cells (1) induces membrane fluidization, disruption of membrane microdomains, and inhibition of drug efflux transporters’ activity (Pgp shown as an example). Pluronic also reaches mitochondria where it (2, 3) inhibits complexes I and IV of mitochondria respiratory chain and (3) induces inner mitochondrial membrane depolarization. This (4) results in ATP depletion and (5) promotes cytochrome c release and ROS generation in MDR cells. Altogether, the MDR cells respond to a Dox/Pluronic combination by (6) an increased proapoptotic signaling and decreased antiapoptotic defense. Reprinted with permission from ref. [181]. ROS: Reactive oxygen species.
- Citation: Cuestas ML, Oubiña JR, Mathet VL. Hepatocellular carcinoma and multidrug resistance: Past, present and new challenges for therapy improvement. World J Pharmacol 2015; 4(1): 96-116
- URL: https://www.wjgnet.com/2220-3192/full/v4/i1/96.htm
- DOI: https://dx.doi.org/10.5497/wjp.v4.i1.96