Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5341
Peer-review started: May 12, 2020
First decision: September 14, 2020
Revised: September 27, 2020
Accepted: October 12, 2020
Article in press: October 12, 2020
Published online: November 6, 2020
Donepezil is an acetylcholinesterase inhibitor used to improve cognition and delay disease progression in dementia patients by increasing acetylcholine levels. This drug may potentially interact with neuromuscular blocking agents (NMBAs) that act on muscular acetylcholine receptors during general anesthesia. Herein, we present a case of inadequate neuromuscular blockade with rocuronium, a nondepolarizing NMBA, in a dementia patient who had taken donepezil.
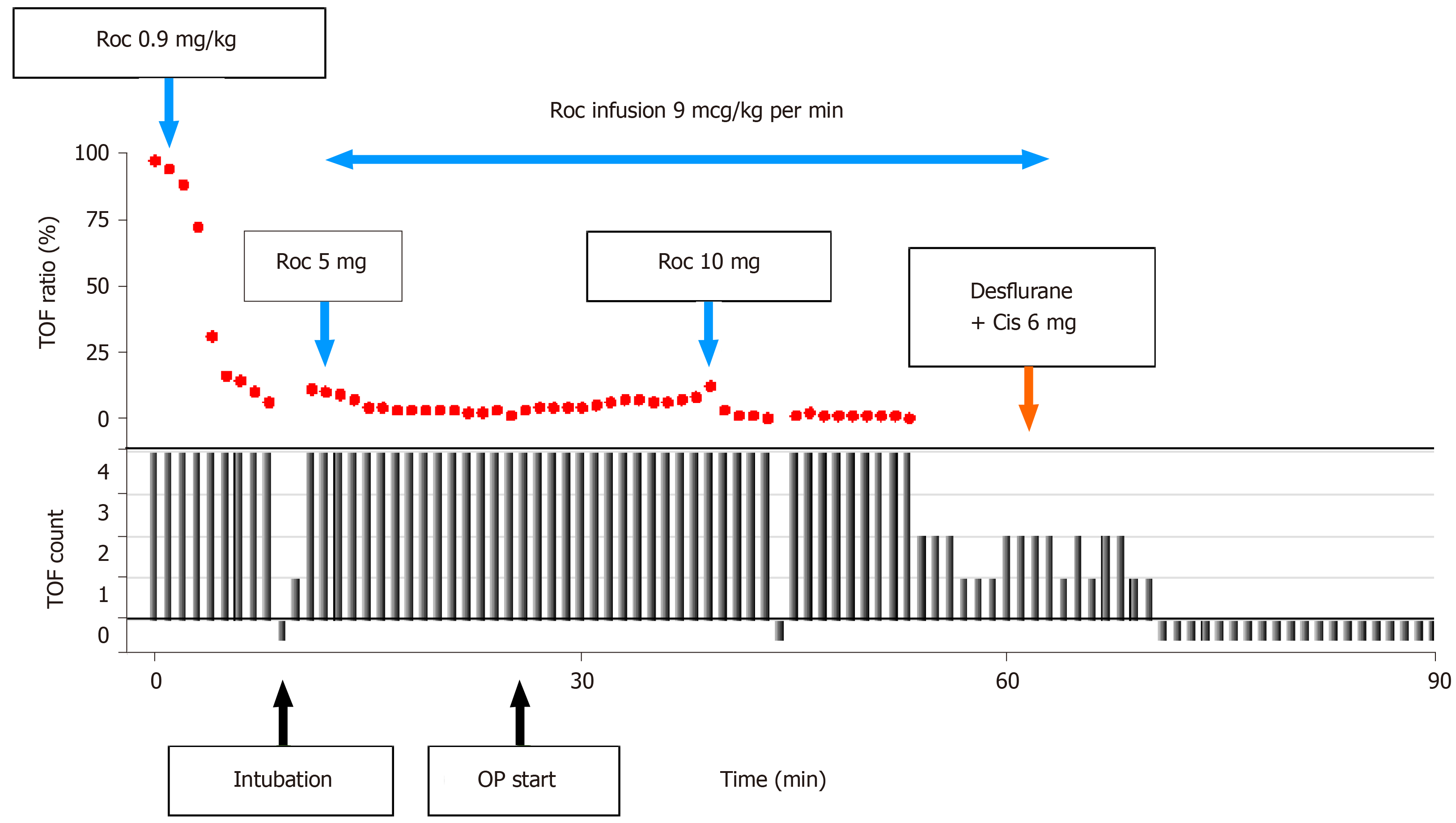
A 71-year-old man was scheduled for laparoscopic gastrectomy. He had been taking donepezil 5 mg for dementia. General anesthesia was induced with propofol and remifentanil. The depth of neuromuscular blockade was monitored by train-of-four (TOF) stimulation. After the administration of rocuronium, the TOF ratio decreased at an unusually slow rate, and a TOF count of 0 was detected 7 min later. After intubation, a TOF count of 1 was detected within 1 min, and a TOF ratio of 12% was detected within 2 min. The TOF count remained at 4 even with an additional bolus and continuous infusion of rocuronium, suggesting resistance to this NMBA. Instead of propofol, an inhalation anesthetic was administered alongside another NMBA (cisatracurium). Then, the quality of neuromuscular blockade improved, and the TOF count remained at 0-1 for the next 70 min. No further problems were encountered with respect to surgery or anesthesia.
Donepezil may be responsible for inadequate neuromuscular blockade during anesthesia, especially when total intravenous anesthesia is used.
Core Tip: In the present case of a 71-year-old patient taking donepezil for dementia, we collected peripheral nerve stimulation data that showed objective evidence of inadequate neuromuscular blockade during total intravenous anesthesia. The goal of this case report is to draw attention to the need to carefully review potential drug interactions between donepezil and neuromuscular blocking agents during general anesthesia. As the number of elderly patients with dementia is increasing and total intravenous anesthesia has become more popular, there is a possibility that this drug interaction may be observed more frequently in the future.
- Citation: Jang EA, Kim TY, Jung EG, Jeong S, Bae HB, Lee S. Donepezil-related inadequate neuromuscular blockade during laparoscopic surgery: A case report. World J Clin Cases 2020; 8(21): 5341-5346
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5341.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5341
As a result of an increasing life expectancy, it is likely that anesthesiologists will encounter an increasing number of elderly patients with dementia in the operating room. As most types of dementia are associated with profound cholinergic deficits, acetylcholinesterase inhibitors have been used to improve cognition and delay disease progression in dementia patients by increasing cerebral acetylcholine levels[1]. Due to this mechanism, these anti-dementia drugs may potentially interact with neuromuscular blocking agents (NMBAs), which act on muscular nicotinic acetylcholine receptors during general anesthesia. Donepezil is an acetylcholinesterase inhibitor approved by the United States Food and Drug Administration for the treatment of Alzheimer’s disease. A few case reports have described donepezil-related resistance to nondepolarizing NMBAs, rocuronium and atracurium, through subjective observations of train-of-four (TOF) stimulation or respiratory effort[2-5]. Herein, we present a case of inadequate neuromuscular blockade with rocuronium during total intravenous anesthesia (TIVA) with propofol-remifentanil in a dementia patient who had taken donepezil. Furthermore, we demonstrate the objective time course of TOF responses. In this case, adequate neuromuscular blockade was achieved with the subsequent administration of an inhalational anesthetic (desflurane) and another NMBA (cisatracurium). Written informed consent was obtained from the patient for the publication of this case.
A 71-year-old man (55 kg, 149 cm) was admitted to the hospital for total laparoscopic distal gastrectomy under general anesthesia. During surgery, insufficient muscle relaxation was reported repeatedly by surgical team.
General anesthesia was induced and maintained with 2% propofol and remifentanil using target-controlled infusion. When the patient became unconscious, TOF stimulation of the right ulnar nerve was initiated using a peripheral nerve stimulator (NMT module of the Carescape monitor B850; GE Healthcare, Madison, WI, United States). The initial TOF ratio was 0.98, and the patient then received a bolus injection of rocuronium 50 mg (0.9 mg/kg). According to routine practice, we waited to perform intubation until a TOF count of 0 was observed. The TOF ratio decreased at an unusually slow rate, and a TOF count of 0 was detected approximately 7 min after the administration of rocuronium (Figure 1). After successful endotracheal intubation, however, a TOF count of 1 was detected within 1 min, and a TOF ratio of 12% was detected within 2 min. Rocuronium 5 mg was then injected followed by a continuous infusion at a rate of 9 µg/kg/min for deep neuromuscular blockade (post-tetanic count of 1-2). However, a TOF count of 4 (TOF ratio < 10%) was continuously recorded and visually detected. The surgical team noted insufficient muscle relaxation 20 min after the start of the laparoscopic procedure.
The patient had previously been diagnosed with dementia and mild parkinsonism with tremor and had been taking donepezil 5 mg, quetiapine 25 mg, and pregabalin 75 mg twice a day for 16 mo. He had been taking anti-hypertensive medication for 11 years and had undergone diaphragm surgery in our hospital 7 and 10 years prior. During these two surgeries, he required rocuronium 50 mg during 195 min of balanced anesthesia with sevoflurane-remifentanil and rocuronium 60 mg during 225 min of TIVA with propofol-remifentanil. No specific events or comments regarding insufficient muscle relaxation were identified from a review of his anesthesia records of previous surgeries.
The patient had no history of smoking or alcohol abuse. He had no family history of cancer or any other hereditary diseases.
During general anesthesia, vascular access for intravenous anesthetics and NMBAs was well secured, and the patient’s vital signs and state entropy (Entropy module of the Carescape monitor B850; GE Healthcare, Madison, WI, United States) were within the normal ranges, which indicated adequate depth of anesthesia. Using forced-air warming blankets, the central core temperature and skin temperature over the adductor pollicis muscle were maintained above 35.5 °C and 32 °C, respectively. The preoperative physical examination was unremarkable.
The results of preoperative laboratory tests and electrocardiography were normal.
The preoperative chest X-ray showed elevation of the left diaphragm, which was considered evidence of previous diaphragm surgeries.
The etiology was considered donepezil-related resistance to nondepolarizing NMBAs based on donepezil’s mechanism and previous case reports.
An additional bolus injection of rocuronium 10 mg (0.18 mg/kg) from different batches of drug product was administered, but the TOF count remained at 1-2 for the next 15 min, and the surgical team requested additional relaxation for optimal surgical conditions. We decided to use an inhalational anesthetic (desflurane) instead of propofol. Therefore, we administered desflurane at an end-tidal concentration of 4-6 vol% while stopping the infusion of propofol and rocuronium. We also administered a bolus dose of cisatracurium 6 mg (0.1 mg/kg) instead of rocuronium.
Adequate neuromuscular blockade was achieved with the subsequent administration of desflurane and cisatracurium. The TOF count remained at 0-1 for the next 70 min without further complaints from the surgical team. At the end of surgery, the TOF ratio was 0.78, and spontaneous respiratory efforts returned soon after all anesthetic drugs were stopped. Residual neuromuscular blockade was reversed with neostigmine 2.5 mg and glycopyrrolate 0.4 mg. When the TOF ratio increased to 0.91 and consciousness returned, extubation was performed successfully. There were no significant problems with the patient’s vital signs in the operating room or recovery room. The patient was transferred to the ward 1 h after the end of surgery. He was discharged from the hospital after 9 d without any complications.
Surgical patients sometimes exhibit resistance to nondepolarizing NMBAs during anesthesia. This manifests as an increased NMBA dose required to abolish the twitch response, a prolonged time to maximum effect, and a shortened duration of neuromuscular blockade after the administration of a bolus[6], as seen in this case.
Resistance to NMBAs has been reported in patients with burns[7,8] and cerebral palsy[9], immobilized patients[10], and patients taking anticonvulsants[11,12]. However, all of these conditions were excluded in this patient. Moreover, no specific problems were described in his anesthesia records from two diaphragm surgeries performed 7 and 10 years prior. During these two surgeries, he required rocuronium 50 mg during 195 min and rocuronium 60 mg during 225 min. In the present case, however, the dose of rocuronium administered during the first 60 min of anesthesia (83 mg) was higher than that administered during two previous surgeries. Therefore, individual variability in NMBA sensitivity may not explain the inadequate neuromuscular blockade observed in this case.
We suspected the existence of a drug-drug interaction between the NMBA and the patient’s current medications. Donepezil was considered to be the drug most likely to be responsible for the observed inadequate neuromuscular blockade, as it is an acetylcholinesterase inhibitor and thus theoretically antagonizes the effects of nondepolarizing NMBAs. We also identified four case reports (two in English) of donepezil-related resistance to nondepolarizing NMBAs. Baruah et al[2] reported that four twitches were continuously observed in response to TOF stimulation after the administration of a single intubating dose of atracurium 30 mg and a supplemental dose of 10 mg in an Alzheimer’s disease patient who had been taking donepezil for 14 mo. Bhardwaj et al[3] reported the case of an Alzheimer’s disease patient who had been taking donepezil (5 mg daily) for 4 mo. Spontaneous respiratory efforts reappeared while attempting intubation after the administration of a single intubation dose of rocuronium 0.6 mg/kg, and repeated administrations of rocuronium and vecuronium could not inhibit the return of spontaneous respiratory efforts. Inadequate neuromuscular blockade with atracurium or rocuronium in Alzheimer’s disease patients taking donepezil (10 mg daily) was also described in the abstracts of two non-English articles[4,5]. In addition, donepezil is known to produce prolonged neuromuscular blockade with depolarizing NMBAs such as succinylcholine[5,13].
Donepezil is a new generation of acetylcholinesterase inhibitors that are considered the first-choice drugs for the pharmacological treatment of dementia, usually of the Alzheimer type[14]. This therapy targets elevated acetylcholine levels in the brain. However, acetylcholine levels at the neuromuscular junction may also increase, resulting in potential interactions between donepezil and NMBAs. The manufacturer of this drug and a few previous articles have recommended that donepezil should be discontinued 2-4 wk before elective surgery due to its long half-life (70 h in heathy volunteers and even longer in elderly patients)[2,13,15]. However, this long withdrawal period may cause irreversible cognitive decline such that cognitive function becomes even worse than that before treatment was initiated[16]. To date, there are no clear guidelines on whether this drug should be discontinued before elective surgery.
In this case, inadequate neuromuscular blockade was noted even at doses higher than those indicated for the patient's weight. The quality of neuromuscular blockade improved when desflurane inhalation was initiated and a single bolus of cisatracurium was administered. Inhalation anesthetics such as desflurane and sevoflurane cause a slight reduction in neuromuscular transmission and enhance the neuromuscular blocking effects of nondepolarizing NMBAs[17,18]. Therefore, the improved muscle relaxation might be associated with the use of desflurane.
Meanwhile, we could not exclude the possibility that cisatracurium might also have contributed to the observed improvement of neuromuscular blockade. Although cisatracurium is a commonly used, intermediate duration, nondepolarizing NMBA just like as rocuronium, the chemical structures of cisatracurium and rocuronium are quite different (benzylisoquinolinium vs steroidal). Mixtures of structurally different NMBAs are considered to produce a synergistic response[19,20]. Thus, the additional administration of cisatracurium might have enhanced the quality of neuromuscular blockade synergistically. In addition, further studies are required to investigate whether cisatracurium has a relatively weak interaction with donepezil.
As the number of elderly patients with dementia is increasing, it is essential that anesthesiologists carefully review the current medications of these patients prior to surgery. In situations when an acetylcholinesterase inhibitor is not discontinued sufficiently long before surgery, the use of a peripheral nerve stimulator and inhalation anesthetics may help achieve adequate neuromuscular blockade for surgery and avoid residual neuromuscular blockade after surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Higa K S-Editor: Gao CC L-Editor: A P-Editor: Xing YX
| 1. | Noufi P, Khoury R, Jeyakumar S, Grossberg GT. Use of Cholinesterase Inhibitors in Non-Alzheimer's Dementias. Drugs Aging. 2019;36:719-731. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Baruah J, Easby J, Kessell G. Effects of acetylcholinesterase inhibitor therapy for Alzheimer's disease on neuromuscular block. Br J Anaesth. 2008;100:420. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Bhardwaj A, Dharmavaram S, Wadhawan S, Sethi A, Bhadoria P. Donepezil: A cause of inadequate muscle relaxation and delayed neuromuscular recovery. J Anaesthesiol Clin Pharmacol. 2011;27:247-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Pautola L, Reinikainen M. [Interaction of donepezil with rocuronium]. Duodecim. 2012;128:1031-1032. [PubMed] [Cited in This Article: ] |
| 5. | Sánchez Morillo J, Demartini Ferrari A, Roca de Togores López A. [Interaction of donepezil and muscular blockers in Alzheimer's disease]. Rev Esp Anestesiol Reanim. 2003;50:97-100. [PubMed] [Cited in This Article: ] |
| 6. | Jung KT, An TH. Updated review of resistance to neuromuscular blocking agents. Anesth Pain Med. 2018;13:122-127. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Martyn JA, Goudsouzian NG, Chang Y, Szyfelbein SK, Schwartz AE, Patel SS. Neuromuscular effects of mivacurium in 2- to 12-yr-old children with burn injury. Anesthesiology. 2000;92:31-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Han T, Kim H, Bae J, Kim K, Martyn JA. Neuromuscular pharmacodynamics of rocuronium in patients with major burns. Anesth Analg. 2004;99:386-392, table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Moorthy SS, Krishna G, Dierdorf SF. Resistance to vecuronium in patients with cerebral palsy. Anesth Analg. 1991;73:275-277. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Hepağuşlar H, Uyar M, Uğur G, Balcioğlu T. Resistance to vecuronium after immobilization. Paediatr Anaesth. 1999;9:94-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Soriano SG, Sullivan LJ, Venkatakrishnan K, Greenblatt DJ, Martyn JA. Pharmacokinetics and pharmacodynamics of vecuronium in children receiving phenytoin or carbamazepine for chronic anticonvulsant therapy. Br J Anaesth. 2001;86:223-229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Gray HS, Slater RM, Pollard BJ. The effect of acutely administered phenytoin on vecuronium-induced neuromuscular blockade. Anaesthesia. 1989;44:379-381. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Crowe S, Collins L. Suxamethonium and donepezil: a cause of prolonged paralysis. Anesthesiology. 2003;98:574-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Birks JS, Harvey RJ. Donepezil for dementia due to Alzheimer's disease. Cochrane Database Syst Rev. 2018;6:CD001190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 174] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 15. | Dooley M, Lamb HM. Donepezil: a review of its use in Alzheimer's disease. Drugs Aging. 2000;16:199-226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 108] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Alcorn S, Foo I. Perioperative management of patients with dementia. BJA Education. 2016;17:94-98. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Kelly RE, Lien CA, Savarese JJ, Belmont MR, Hartman GS, Russo JR, Hollmann C. Depression of neuromuscular function in a patient during desflurane anesthesia. Anesth Analg. 1993;76:868-871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Rupp SM, Miller RD, Gencarelli PJ. Vecuronium-induced neuromuscular blockade during enflurane, isoflurane, and halothane anesthesia in humans. Anesthesiology. 1984;60:102-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 120] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Naguib M, Samarkandi AH, Ammar A, Elfaqih SR, Al-Zahrani S, Turkistani A. Comparative clinical pharmacology of rocuronium, cisatracurium, and their combination. Anesthesiology. 1998;89:1116-1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Paul M, Kindler CH, Fokt RM, Dipp NC, Yost CS. Isobolographic analysis of non-depolarising muscle relaxant interactions at their receptor site. Eur J Pharmacol. 2002;438:35-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |