Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4223
Peer-review started: July 28, 2020
First decision: August 7, 2020
Revised: August 10, 2020
Accepted: August 22, 2020
Article in press: August 22, 2020
Published online: September 26, 2020
Neurofibroma can be a clinical manifestation of neurofibromatosis, which is a benign neurogenic tumor that occurs sporadically. Neurofibromas in the abdomen usually appear in the retroperitoneal space. Reports on neurofibromas in the abdominal wall are rare, and multiple recurrent neurofibromas in this area have not yet been reported.
This is a case of a 73-year-old man who suffered from multiple recurrent neurofibromas in the abdominal wall for 16 years and received 13 surgical treatments.
We need to pay due attention to its treatment, and primary surgery should be designed thoroughly.
Core Tip: Neurofibromas in the abdominal wall are rare, and multiple recurrent neurofibromas in this area have not yet been reported.
- Citation: Zhao XF, Shen YM, Chen J. Multiple recurrent neurofibromas in the abdominal wall: A case report. World J Clin Cases 2020; 8(18): 4223-4227
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4223.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4223
Neurofibromas are the most prevalent benign nerve sheath tumors in the peripheral nervous system[1-3]. Solitary neurofibroma is the most common of three types and occurs commonly in younger individuals regardless of sex[4]. Various body parts are reportedly affected by neurofibromas[5], including the abdominal wall. However, neurofibromas in the abdominal wall are rare, and recurrent cases have not been found in the literature[6,7]. We herein report multiple recurrent neurofibromas in the abdominal wall.
A 73-year-old man was admitted to our department with a huge mass in the abdominal wall for 4 mo.
Prior to admission, the patient had suffered from recurring abdominal wall tumor for 16 years. Sixteen years ago, a mass was observed on the patient’s lower abdominal wall for the first time. He underwent a resection surgery, and the postoperative pathologic report showed a neurofibroma. He did not receive any adjuvant therapy, and the tumor recurred quickly 1 year later. He received the second resection surgery and received the same pathologic result. From then on, the patient had to undergo resection surgeries repeatedly against the recurrent tumor. Before coming to our department, the patient had undergone 13 resection surgeries and received mesh repair simultaneously in 2 of the 13 operations. This time, the 4-mo mass in the lower abdominal wall was the reason for hospitalization.
There was nothing special in his medical history except well-controlled blood hypertension and he had no family history of the disease.
On physical examination, multiple surgical scars and local skin swelling were observed in the lower abdominal wall. A large hard subcutaneous mass was palpated in this area, which was covered with normal skin. The mass had a clear boundary and was immovable.
The results of routine blood tests and biochemical tests were normal. The serum tumor marker test showed an elevation of CA 72-4 (17.6 U/mL).
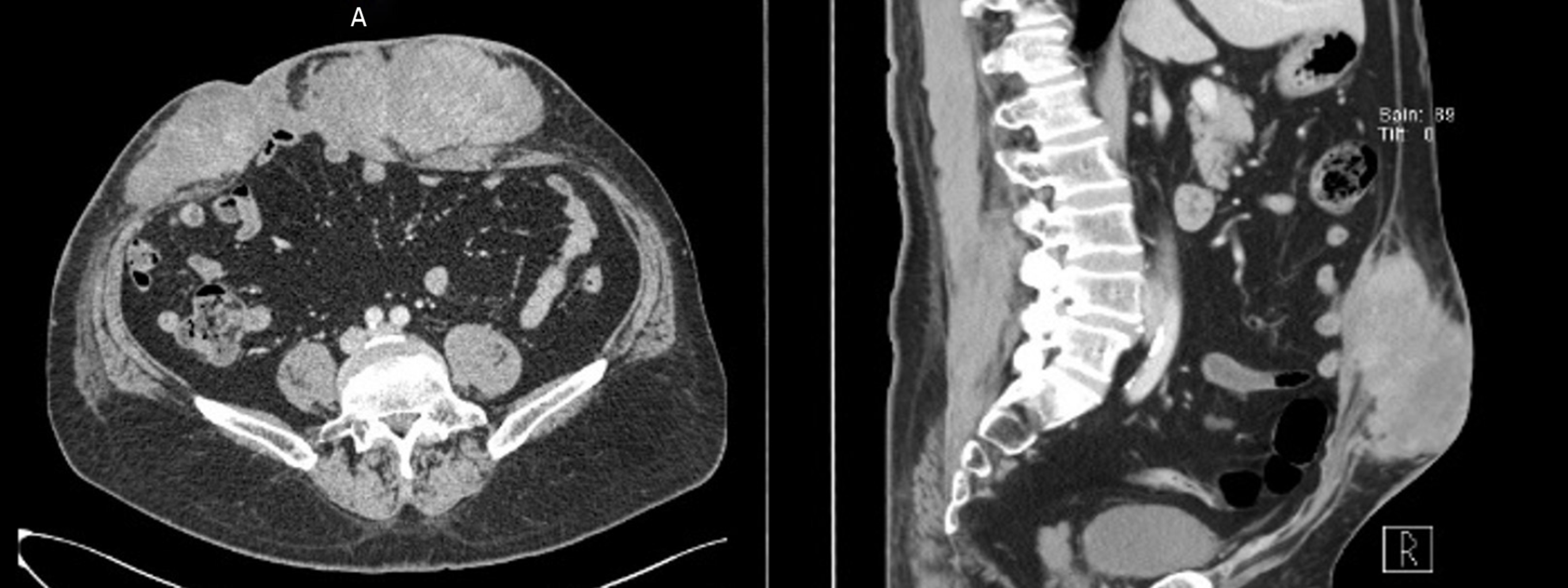
The enhanced computed tomography (CT) scan revealed a large irregular diffuse lobulated soft tissue mass, which was 25 cm × 15 cm × 8 cm in size and had an inhomogeneous enhancement (Figure 1). The mass was located at the subcutaneous layer, extending left to the lateral margin of left rectus abdominis and right to the right midaxillary line. The mass was well-defined to muscles posteriorly, but could not be separated from skin anteriorly.
The final diagnosis is multiple recurrent neurofibromas in the abdominal wall.
The patient received interventional artery therapy first. During the operation, bilateral superficial epigastric arteries were found to be the main blood supply to the tumor and were embolized. At 6 d after interventional therapy, the patient underwent radical tumor resection. During the operation, en bloc removal of the tumor with the surrounding tissues was performed. The invasion of abdominal wall muscles, peritoneum, and omentum was observed, and all of the impaired tissue was excised. The large full-thickness defect caused by resection was reconstructed by bridging repair with an anti-adhesive mesh.
Postoperative histopathological examination revealed a fusiform cell and oval cell tumor. No significant signs of atypia and necrosis were present. The mitosis count was 1-2/10 HPF. Areas of neutrophil infiltration were observed. The margin of the extracted samples tested positive. The further immunohistochemical test showed tumor cells were positive for vimentin, cluster of differentiation 34, S-100, and Ki-67 (< 5%). The diagnosis from the combined reports was neurofibroma.
The patient developed incisional infection induced by effusion postoperatively, and he was asked to leave the hospital although the infection had not been cured entirely. Fortunately, the mesh was not involved in the infection. One year later, this patient came to our department again for recurrent tumors, and underwent resection and reconstruction surgery again. The invaded small intestine was observed and resected together with the tumor body during the operation. The postoperative histopathological result was still neurofibroma.
The postoperative course was uneventful. Regrettably, we lost contact with the patient after several months’ follow-up.
Neurofibroma is a kind of benign tumor that results from a mutation in the NF1 gene[8,9]. Neurofibromas occur sporadically, and few cases are associated with neurofibromatosis[10]. Neurofibromas can be divided into three types: Localized/solitary (most common), diffuse, and plexiform. Except for the plexiform type, neurofibromas have a very low propensity for malignant transformation[10]. The retroperitoneal space is the most commonly involved site in the abdomen; neurofibromas of the abdominal wall are very rare[6,7,11], and no case of long-lasting and multiple recurrent neurofibromas in the abdominal wall has been reported to date.
Preoperative imagological examination CT/magnetic resonance imaging is necessary and helpful for assessing the location, size, and extent of the tumor and detecting invasions of other organs[12,13]. All of these clues are useful and critical for developing the surgical plan, but they are not sufficient for qualitative diagnosis. Histological and immunohistochemical results are still needed to make the final diagnosis. In this case, the patient received a consistent postoperative histological diagnosis from two surgeries in our department—neurofibroma—and the immunohistochemical results supported the diagnosis.
Radical resection is the preferred and possibly only effective treatment for neurofibromas, especially for localized cases. There are also some reports of other therapies for neurofibromas, such as radiotherapy, interventional embolization, ACE inhibitors and interferon-α, with variable results[14-17]. In this case, we performed interventional embolization 6 d before resection surgery as an adjuvant therapy in an attempt to shrink the tumor to decrease the difficulty of surgery. However, it did not seem to work well, as shrinking of the tumor was not obvious. We speculated that the procedure needed more time to take effect.
Such tumor resections typically create an extensive full-thickness abdominal wall defect. The complex reconstruction of the abdominal wall in these cases is challenging and requires advanced techniques, which can involve various autologous tissue grafts and flaps and mesh reinforcement[18]. The procedure also demands it experienced senior surgeons who work in reconstruction and even multidisciplinary collaboration.
The recurrence of neurofibromas is the most concerning problem for both patients and physicians. To obtain a radical margin, resection of normal tissue to > 2 cm beyond the tumor border is typically recommended[19,20]. In this case, the patient underwent multiple operations and experienced recurrence after each operation performed in the past 16 years. The presumed reason is an insufficient resection area, which resulted in residual tumors. The tumor advanced gradually and invaded the intraabdominal organs during the long course of the illness. Although we did our best to achieve radical resection by resecting all the invaded organs and tissue, the histological report still revealed a positive surgical margin. This demonstrated that multiple operations and recurrence led to a malignant process of disease and thus negatively influenced the ability to achieve radical resection.
Neurofibroma in the abdominal wall is a benign tumor. Nonetheless, we still need to pay due attention to its treatment. Primary surgery should be designed thoroughly to achieve radical resection and avoid postoperative recurrence, which might lead to malignant transformation of the tumor, resulting in multiple operations, and reduce patient quality of life and lifespan.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Becker C, Steenholdt C S-Editor: Yan JP L-Editor: Filipodia P-Editor: Liu JH
| 1. | Maertens O, Brems H, Vandesompele J, De Raedt T, Heyns I, Rosenbaum T, De Schepper S, De Paepe A, Mortier G, Janssens S, Speleman F, Legius E, Messiaen L. Comprehensive NF1 screening on cultured Schwann cells from neurofibromas. Hum Mutat. 2006;27:1030-1040. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Cichowski K, Shih TS, Schmitt E, Santiago S, Reilly K, McLaughlin ME, Bronson RT, Jacks T. Mouse models of tumor development in neurofibromatosis type 1. Science. 1999;286:2172-2176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 359] [Cited by in F6Publishing: 376] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 3. | Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 2005;102:246-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 199] [Cited by in F6Publishing: 191] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 4. | Tahririan MA, Hekmatnia A, Ahrar H, Heidarpour M, Hekmatnia F. Solitary giant neurofibroma of thigh. Adv Biomed Res. 2014;3:158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Lee YB, Lee JI, Park HJ, Cho BK. Solitary neurofibromas: does an uncommon site exist? Ann Dermatol. 2012;24:101-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Barajas-Gamboa JS, Flórez-Salamanca L. Solitary neurofibroma in the abdominal wall of a patient without neurofibromatosis: case report. Biomedica. 2009;29:501-505. [PubMed] [Cited in This Article: ] |
| 7. | Patel M, Rani KU, Sharma M, Bhatnagar A. A Rare Case of Giant Solitary Neurofibroma of Abdominal Wall Masked by Pregnancy. J Clin Diagn Res. 2017;11:QD08-QD09. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Behrad S, Sohanian S, Ghanbarzadegan A. Solitary intraosseous neurofibroma of the mandible: Report of an extremely rare histopathologic feature. Indian J Pathol Microbiol. 2020;63:276-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Fontana S, Menutti L, Borrego F, Ferreyra de Prato R, Corominas OS. [Isolated neurofibroma of oral cavity. An unusual manifestation case report]. Rev Fac Cien Med Univ Nac Cordoba. 2020;77:45-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Skovronsky DM, Oberholtzer JC. Pathologic classification of peripheral nerve tumors. Neurosurg Clin N Am. 2004;15:157-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Chang CG, Provost DA, LeVoyer T, Ellison RW. Abdominal wall neurofibroma presenting as an inguinal hernia. Mil Med. 2004;169:192-193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Subhawong TK, Fishman EK, Swart JE, Carrino JA, Attar S, Fayad LM. Soft-tissue masses and masslike conditions: what does CT add to diagnosis and management? AJR Am J Roentgenol. 2010;194:1559-1567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 13. | Serletis D, Parkin P, Bouffet E, Shroff M, Drake JM, Rutka JT. Massive plexiform neurofibromas in childhood: natural history and management issues. J Neurosurg. 2007;106:363-367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Marchetti M, Franzini A, Nazzi V, De Martin E, Fariselli L. Radiosurgical treatment of ulnar plexiform neurofibroma in a neurofibromatosis type 1 (NF1) patient. Acta Neurochir (Wien). 2013;155:553-555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Cavallaro G, Pedullà G, Crocetti D, D'Ermo G, Giustini S, Calvieri S, De Toma G. Vacuum-assisted closure treatment of leg skin necrosis after angiographic embolization of a giant plexiform neurofibroma. G Chir. 2012;33:239-242. [PubMed] [Cited in This Article: ] |
| 16. | Namazi H. ACE inhibitors: a novel treatment for neurofibroma. Ann Surg Oncol. 2008;15:1538-1539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Kebudi R, Cakir FB, Gorgun O. Interferon-α for unresectable progressive and symptomatic plexiform neurofibromas. J Pediatr Hematol Oncol. 2013;35:e115-e117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Kovacević P, Velickov A, Stojiljković D, Velickov A, Ceranić Z. Reconstruction of full thickness abdominal wall defect following tumor resection: a case report. Srp Arh Celok Lek. 2014;142:347-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Stojadinovic A, Hoos A, Karpoff HM, Leung DH, Antonescu CR, Brennan MF, Lewis JJ. Soft tissue tumors of the abdominal wall: analysis of disease patterns and treatment. Arch Surg. 2001;136:70-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Bodin F, Dissaux C, Romain B, Rohr S, Brigand C, Bruant-Rodier C. Complex abdominal wall defect reconstruction using a latissimus dorsi free flap with mesh after malignant tumor resection. Microsurgery. 2017;37:38-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |