Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2644
Peer-review started: May 21, 2019
First decision: July 30, 2019
Revised: August 14, 2019
Accepted: August 20, 2019
Article in press: August 20, 2019
Published online: September 6, 2019
As the population ages and people’s living standards gradually improve, the incidence of cerebrovascular disease in China is increasing annually, posing a serious threat to people’s health. The incidence of brachiocephalic artery stenosis in ischemic cerebrovascular disease is relatively low, accounting for 0.5% to 2% of patients, but its consequences are very serious. Herein, we report a case of brachiocephalic artery stenting through the carotid artery.
The patient was a 66-year-old man. He came to our hospital because of repeated dizziness and was diagnosed with ischemic cerebrovascular disease (stenosis at the beginning of the brachiocephalic artery). Cerebral angiography suggested that the stenosis of the brachiocephalic artery had almost occluded it. Contrast agent threaded a line through the stenosis, and there was reversed blood flow through the right vertebral artery to compensate for the subclavian steal syndrome in the right subclavian artery. To improve the symptoms, we placed an Express LD (8 mm × 37 mm) balloon expanding stent in the stenosis section. After the operation, the patient’s dizziness significantly improved. However, after 6 mo, the patient was re-admitted to the hospital due to dizziness. A computed tomography scan of the head revealed multiple cerebral infarctions in bilateral basal ganglia and the right lateral ventricle. An auxiliary examination including computerized tomography angiography of the vessels of the head and cerebral angiography both showed severe stenosis in the brachiocephalic artery stent. During the operation, the guidewire and catheter were matched to reach the opening of the brachiocephalic artery. Therefore, we decided to use a right carotid artery approach to complete the operation. We sutured the neck puncture point with a vascular stapler and then ended the operation. After the operation, the patient recovered well, his symptoms related to dizziness disappeared, and his right radial artery pulsation could be detected.
In patients with brachial artery stenosis, when the femoral artery approach is difficult, the carotid artery is an unconventional but safe and effective approach. At the same time, the use of vascular suturing devices to suture a carotid puncture point is also commendable. Although it is beyond the published scope of the application, when used cautiously, it can effectively avoid cerebral ischemia caused by prolonged artificial compression, and improper suturing can lead to stenosis of the puncture site and improper blood pressure, resulting in the formation of a hematoma. Finally, satisfactory hemostasis can be achieved.
Core tip: Ischemic cerebrovascular disease is one of the diseases most harmful to the Chinese elderly population. Although the brachiocephalic artery stenosis is rare, it is very harmful. This article describes the possibility and safety of brachiocephalic arterioplasty through a carotid artery. It also illustrates the feasibility of suturing the carotid puncture site with a suturing device. We hope that it will inspire our peers.
- Citation: Xu F, Wang F, Liu YS. Brachiocephalic artery stenting through the carotid artery: A case report and review of the literature. World J Clin Cases 2019; 7(17): 2644-2651
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2644.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2644
As the population ages and people's living standards gradually improve, the incidence of cerebrovascular disease in China is increasing annually, posing a serious threat to people’s health[1-4]. Ischemic cerebrovascular disease is the main type of cerebrovascular disease, accounting for more than 70% of cerebrovascular disease cases. It mainly includes vertebrobasilar insufficiency, cerebral insufficiency, transient ischemic attack, and cerebral infarction, and its main cause is atherosclerosis[5,6]. Regardless of the location, interventional therapy and open surgery are the standard methods of treatment. The stenosis or occlusion of the origin of the brachiocephalic artery has unique characteristics. If endarterectomy is used, making the incision in the neck makes it difficult to reach the target blood vessels and requires thoracotomy. These open surgeries are traumatic, risky, and difficult to perform. Interventional minimally invasive surgery has therefore become the main method to treat stenosis at the beginning of the brachiocephalic artery. The femoral artery approach is the most common approach used for endovascular exclusion of the aorta. However, in cases involving an abnormal aortic arch or obvious distortion of the arteries, the trans-femoral approach is difficult to use because of its low success rate and high incidence of complications during the perioperative period. In addition to avoiding the occurrence of this situation and achieving faster and more effective hemostasis, we used a Perclose Proglide vascular stapler to suture the carotid puncture point. Herein, we report a case sustaining the possibility and safety of brachiocephalic arterioplasty through a carotid artery. It also illustrates the feasibility of suturing the carotid puncture site with a suturing device.
A 66-year-old man presented with intermittent dizziness for two years and aggravation for 10 d.
The patient have been smoking for more than 30 years, with more than 20 cigarettes a day. He had drunk for more than 40 years and has stopped drinking now.
The patient had a more than 10-year history of type 2 diabetes and severe diabetic eye disease with blindness in the left eye. The patient self-injected long-acting insulin subcutaneously, 12 units per day. The patient denied having other diseases.
His father died of heart disease at the age of 72 years. His mother and children are healthy.
First admission to hospital in March 2018: On physical examination, the patient’s blood pressure in the left upper limb was 120/70 mmHg, and blood pressure was not detected in the right upper limb. The patient was conscious and able to answer questions fluently, no abnormalities were detected on a nervous system examination, and the right brachial artery and radial artery pulsations were not detected.
Second admission in October 2018: The pressures in the left and right upper limbs were 140/68 mm and 85/60 mmHg, respectively. The results of a nervous system examination were normal. The right radial artery pulsation could not be detected, but the left radial artery pulsation was accessible. The patient was conscious and could carry on a normal conversation but had slightly slurred speech.
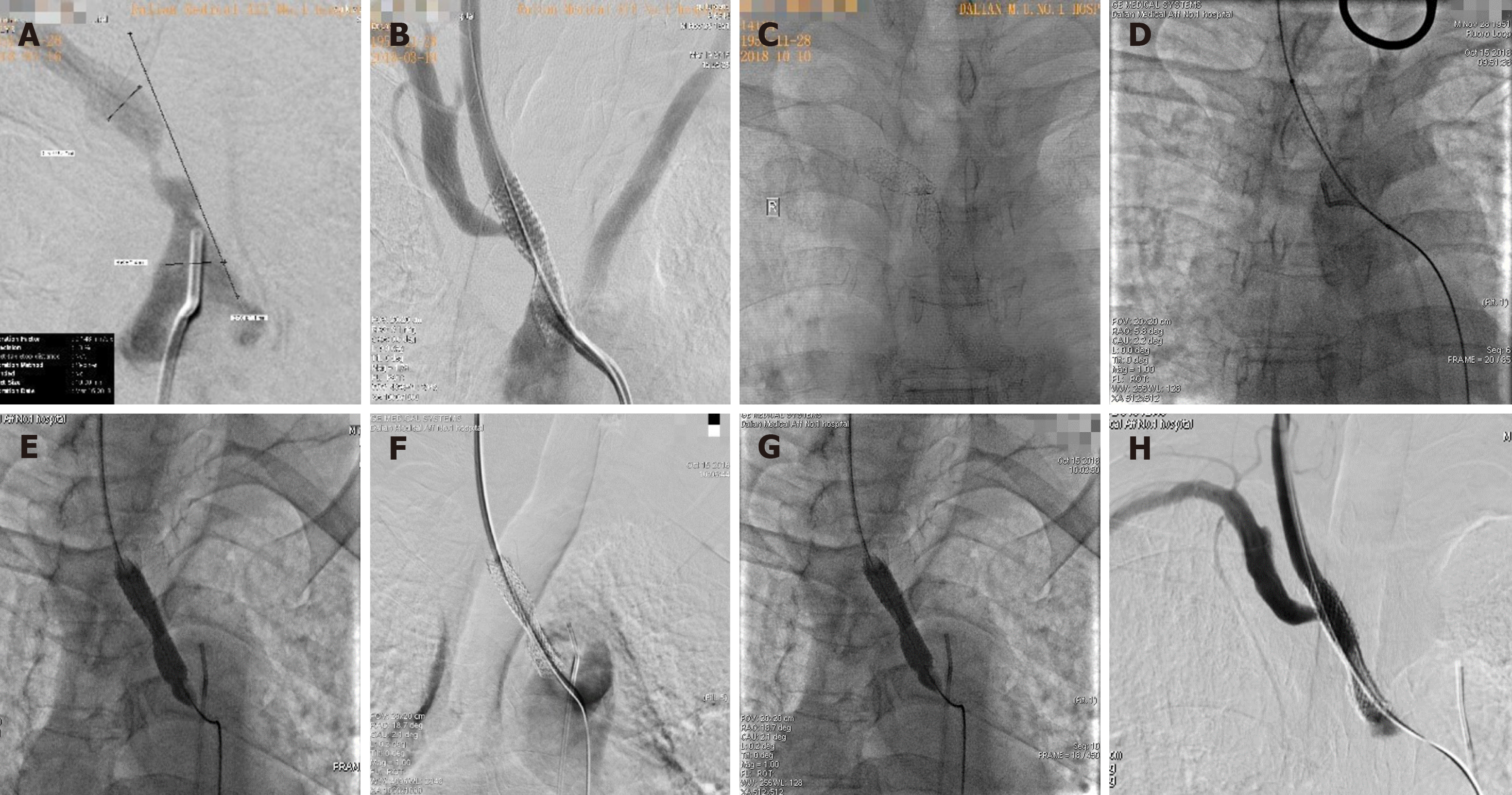
Imaging studies including a computed tomography (CT) scan of the head, computerized tomography angiography (CTA) of the vessels of the head and neck, and cerebral angiography. Upon the first admission to hospital in March 2018, CTA of the vessels of the head and neck showed severe stenosis at the beginning of the brachiocephalic artery. A CT scan of the head showed no obvious abnormalities. Cerebral angiography showed that the stenosis of brachiocephalic artery had almost occluded it (Figure 1A). Upon the second admission in October 2018, a CT scan of the head revealed multiple cerebral infarctions in bilateral basal ganglia and the right lateral ventricle. CTA of the vessels of the head and cerebral angiography both showed severe stenosis in the brachiocephalic artery stent. Reverse blood flow through the right vertebral artery compensated for the right subclavian artery, and the left internal carotid artery was occluded.
Laboratory examinations included routine blood tests, liver function, kidney function, electrolytes, coagulation function, routine stool, and urine tests and relevant immune factor tests, and no obvious abnormalities were found. Only blood lipid examination was abnormal (Table 1).
| First admission to hospital in March 2018 | Second admission in October 2018 | |
| TG | 2.14 mmol/L | 2.07 mmol/L |
| TC | 7.43 mmol/L | 7.03 mmol/L |
| LDL-C | 4.36 mmol/L | 4.29 mmol/L |
After a series of imaging examinations and laboratory tests, the patient was diagnosed with cerebral vascular stenosis caused by atherosclerosis (stenosis of the brachiocephalic artery).
In order to clarify the situation of vascular stenosis, we first performed cere-brovascular angiography. Cerebral angiography showed severe stenosis at the beginning of the brachiocephalic artery (Figure 1A). To improve the symptoms, including cerebral ischemia, and prevent cerebral stroke, interventional surgery was performed on March 19, 2018. We placed an Express LD (8 mm × 37 mm) balloon expanding stent (Boston, United States) in the stenosis section (Figure 1B). After the operation, the patient’s dizziness significantly improved. His upper left arm blood pressure was 130/85 mmHg, his right upper arm blood pressure was 122/73 mmHg, and his right radial artery pulsation was detectable.
The patient continued oral aspirin (100 mg) and clopidogrel antiplatelet therapy (75 mg) after discharge.
In order to clarify the situation of vascular stenosis, we first performed cerebrovascular angiography. Cerebral angiography showed severe stenosis at the beginning of the brachiocephalic artery (Figure 1C). After clarifying the stenosis of blood vessels, we carefully studied the operation plan. During the operation, vascular access was conventionally established in the right femoral artery, and a 6F sheath tube was inserted. The guidewire and catheter were matched to reach the opening of the brachiocephalic artery. We repeatedly attempted but failed to use the guidewire to pass the stenosis segment. We believe that there were certain difficulties related to the surgical approach through the femoral artery, and we therefore determined that continuing attempts may have resulted in plaque detachment and affected the patency of distal cerebral blood vessels. Preoperative angiography confirmed that the patient’s right carotid artery was unobstructed and showed no obvious stenosis or plaque. Therefore, we decided to use a right carotid artery approach to complete the operation. First, we punctured the right common carotid artery with a miniature puncture needle according to the Roadmap (the puncture point was located approximately 1 cm below the bifurcation of the carotid artery). After a 6F short sheath was inserted, we replaced the V-18 guidewire with a vertebral artery catheter and reversed the blood flow through the stricture to reach the ascending aorta (Figure 1D). Along the guidewire, we sent an Evercross (6 mm × 60 mm) (EV3, United States) balloon into the stenosis place to pre-expand it (Figure 1E). We placed a Wallstent (9 mm × 30 mm) stent (Boston, United States) in the stricture, and we then performed another angiogram. We found residual stenosis in the stent (Figure 1F), and we therefore sent an Evercross (8 mm × 40 mm) balloon (EV3, United States) through to expand the stenosis (Figure 1G). Angiography showed that the position of the stent was satisfactory, and the blood flow rate returned to normal (Figure 1H). We sutured the neck puncture point with a vascular stapler (Perclose Proglide, provided by Abbott Vascular, United States) and then ended the operation. After the operation, the patient recovered well, his symptoms related to dizziness disappeared, and his right radial artery pulsation could be detected. The blood pressure of the left upper limb was 135/88 mmHg, while that of the right was 128/80 mmHg. A follow-up performed 6 mo after the operation showed that there were no ischemic symptoms, such as dizziness, and no pulse.
The patient continued oral aspirin (100 mg) and clopidogrel antiplatelet therapy (75 mg) after discharge. And we asked the patient to take the drug on time and in volume. A follow-up performed 6 mo after the operation showed that there were no ischemic symptoms, such as dizziness, and no pulse.
The brachiocephalic artery is the largest branch of the aortic arch and is also known as the brachial artery or the innominate artery. It extends distally into the right carotid artery and the right subclavian artery and supplies blood to the right cerebral hemisphere and right upper limb. Therefore, patients with brachiocephalic artery stenosis often have dizziness and no pulse in the right upper limb. Further development of this condition may lead to ischemic gangrene in the right upper limb and cerebral infarction caused by posterior circulation ischemia[7]. Common causes of stenosis of the brachiocephalic artery include atherosclerosis, multiple arteritis, and radiation arteritis. There are several treatments for patients with ischemic cerebrovascular disease who exhibit significant ischemic symptoms or are not treated with medicine. Traditional endovascular stripping, intracranial and extravascular revascularization, or interventional endovascular treatment can be selected. Endovascular stripping is one of the earliest surgical procedures that can be used in extracranial cerebral vascular stenosis. It is the first choice for the treatment of carotid stenosis in developed regions, such as Europe and the United States[8,9]. Several multicenter randomized controlled trials have confirmed the efficacy of endovascular stripping, such as the North American Symptomatic Carotid Endarterectomy Text[10], the European Carotid Surgery Test[11], the Asymptomatic Carotid Atherosclerosis Study, and the Asymptomatic Carotid Surgery Test. Resection of atherosclerotic plaques in the intima can reduce the incidence of cerebral infarction at low cost and with a high success rate. This is therefore one of the methods used to prevent and treat moderate and severe cerebrovascular stenosis[12]. However, this operation is more traumatic and has higher requirements regarding the patient’s physical condition; it is therefore not suitable for patients with stenotic vessels that are too long or difficult to expose. Intracranial and extracranial revascularization can theoretically improve intracranial blood supply in patients with severe cerebral hemodynamic disorders; however, an international multicenter randomized controlled trial denied that this treatment method produced good effects. More recently, the Carotid Occlusion Surgery Study showed that the probability of recurrent cerebrovascular events occurring in patients undergoing bypass surgery has not decreased[13]. Due to the deep and complicated location of the brachiocephalic artery, it is very difficult to expose the operative field during surgery. In contrast, endovascular interventional therapy is widely used because of its advantages, which include a small amount of trauma, a fast recovery, a high success rate, a low rate of operation-related complications, and high mid and long-term patency rates[14]. Hüttl et al[15] reported 89 cases of brachiocephalic artery stenosis or occlusion treated with interventional therapy, and theirs is the largest case series published so far. The technical success rate was 96.6%, and the follow-up rate was 12%, with a follow-up period ranging from 12 to 117 mo. This shows that endovascular therapy is a simpler, safer, and more effective method for treating brachiocephalic artery stenosis. However, this approach is not perfect, and vascular stenting does have limitations. For example, in cases with inadequate brain protection, the incidence of postoperative cerebral infarction is higher[16-18]. In addition, the costs of this treatment are higher. With the improvement of interventional devices and techniques, the incidence of related complications has been significantly reduced, and an increasing number of patients therefore choose vascular interventional therapy[19-21].
The femoral artery approach is the most common approach used for endovascular exclusion of the aorta. However, in cases involving an abnormal aortic arch or obvious distortion of the arteries, the trans-femoral approach is difficult to use because of its low success rate and high incidence of complications during the perioperative period. In addition, it is also difficult to apply the femoral artery approach in patients with thoracic aortic dissection, iliofemoral artery occlusive disease, or inguinal infection[22]. For the patient in this case, we tried the femoral artery approach first, but we could not pass the guidewire through the lesion after repeated attempts because of severe restenosis in the stent. An approach via the brachial artery and radial artery was also abandoned because of severe stenosis in the brachiocephalic artery, and his arterial pulsation was difficult to detect. Under these circumstances, the carotid artery approach, although unconventional, has become another option to establish vascular access. At present, no relevant articles have reported performing brachial arterioplasty via this approach. Some scholars have suggested that[23,24] compared with the conventional femoral artery approach, the carotid artery approach can reduce the risk of embolism because it avoids an abnormal aortic arch (type III aortic arch, long aortic arch, severe atherosclerosis of aorta, deformed aorta, etc.). Possible complications of using the trans-carotid approach include local nerve injury, local hemorrhage, or hematoma. Patients with severe atherosclerosis of the common carotid artery or stenosis at the puncture site are not suitable for this treatment if they also have a history of neck surgery or radiotherapy[25]. Bergeron[24] reported 52 cases in which carotid artery stenting was performed via the carotid artery approach, achieving a technical success rate of 100% and no occurrence of stroke, cardiovascular events, or hemorrhage. Ghosh et al[26] reported performing endovascular exclusion of abdominal aortic aneurysms via the carotid artery and also achieved satisfactory results. In our case, it was difficult to establish vascular access via conventional approaches, and the carotid artery approach was therefore adopted. The operation was successful without any serious complications. Drawing on the literature and the cases presented in our work, we propose that the carotid artery approach, although unconventional, can be used to complete surgeries on intracranial, extracranial, cerebrovascular, and even large blood vessels.
However, the carotid artery approach has disadvantages. If the condition of the carotid artery is poor or the carotid pulse weak due to stenosis and occlusion, puncture will be difficult. Moreover, no brain-protecting device has been specially designed for the carotid artery approach, which can cause plaque detachment during the operation. Therefore, the selection of a carotid artery approach should be carefully considered in these cases. It is suggested that cerebral angiography results should be refined preoperatively to clarify the condition of the bilateral carotid arteries. When puncturing the target carotid artery, the puncture should be performed using Roadmap or ultrasound[27]. On the one hand, this can clarify the puncture position and thereby avoid any damage to the carotid bifurcation. On the other hand, it can also avoid cerebral infarction caused by plaque detachment.
It is more difficult to apply compression hemostasis to a carotid puncture point than to the femoral artery. Bleeding and even subcutaneous hematoma can therefore easily occur. In severe cases, a huge cervical subcutaneous hematoma may even compress the esophagus, causing dyspnea[28]. To avoid the occurrence of this situation and achieve faster and more effective hemostasis, we used a Perclose Proglide vascular stapler to suture the carotid puncture point. Previous studies have reported that the Proglide vascular stapler is mainly used in the endovascular treatment of large vessels with the femoral artery used as the puncture approach[29]. Perclose prosglide vascular stitching devices can reduce postoperative recovery times and the time spent bed-bound. More importantly, it can also reduce subcutaneous hematoma and surgical scars[30]. Patients undergoing endovascular intervention often take antiplatelet or anticoagulant drugs for a long time before surgery, and this increases the risk of hemostasis complications at the puncture point. Since the 1990s, vascular suturing devices have been used in coronary interventions performed through the femoral artery, in which they have been shown to have advantages, such as reduced hemostasis and bed rest times[30]. Compared with traditional manual compression hemostasis, vascular suturing devices can also reduce the incidence of vagus nerve reflexes and deep venous thrombosis caused by excessive compression[31,32]. The main factors affecting the suture success rate include self-factors, such as obesity, severe calcification of the target vessel wall, and severe tortuosity of the blood vessels, as well as the size of the sheath. Therefore, before using a vascular stapler, whether the above situation exists should be clarified. The product instructions included with the Proglide Vascular Stapler state that for patients undergoing interventional catheterization or treatment, a 5F to 21F sheath is suggested to be used. The suture is delivered percutaneously after surgery to suture the common femoral artery puncture site. In this case, this approach was used to suture the carotid puncture points; while this is beyond the scope of the described applications, there were no complications, such as vascular stenosis or subcutaneous hematoma formation. Finally, satisfactory hemostatic effects have been achieved. Compared with other hemostasis methods, such as manual compression hemostasis and vascular closure, using vascular suturing devices produces fewer complications[33,34]. This method also helps to reduce the time during which the puncture points must be pressed, shortens bed rest times, and improves patient comfort. Therefore, the authors believe that it is appropriate to carefully use a vascular stapler for the cervical vascular puncture point. The surgeons must be able to use the vascular suture devices skillfully. The puncture site must be adequately anesthetized to avoid vagus nerve reflex caused by local pain. The operation must be performed carefully to achieve safe and effective use of the vascular suture devices and make patients more comfortable[35].
In summary, in patients with brachial artery stenosis, when the femoral artery approach is difficult, the carotid artery is an unconventional but safe and effective approach. At the same time, the use of vascular suturing devices to suture a carotid puncture point is also commendable. Although it is beyond the published scope of the application, when used cautiously, it can effectively avoid cerebral ischemia caused by prolonged artificial compression, and improper suturing can lead to stenosis of the puncture site and improper blood pressure, resulting in the formation of a hematoma. Finally, satisfactory hemostasis can be achieved.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim KC, Pizzirusso F S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Zhao FF, Gao HY, Gao Y, Zhao Z, Li J, Ning FB, Zhang XN, Wang ZG, Yu AL, Guo YY, Sun BL. A Correlational Study on Cerebral Microbleeds and Carotid Atherosclerosis in Patients with Ischemic Stroke. J Stroke Cerebrovasc Dis. 2018;27:2228-2234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Xu T, Zuo P, Cao L, Gao Z, Ke K. Omentin-1 is Associated with Carotid Plaque Instability among Ischemic Stroke Patients. J Atheroscler Thromb. 2018;25:505-511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Kim SW, Kim YD, Chang HJ, Hong GR, Shim CY, Chung SJ, Hong JY, Song TJ, Song D, Bang OY, Heo JH, Nam HS. Different infarction patterns in patients with aortic atheroma compared to those with cardioembolism or large artery atherosclerosis. J Neurol. 2018;265:151-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Zhang Y, Chen Z, Tang Y, Shan W, Wang L, Shi J, Luo Q, Duan J, Xu G. Association between procalcitonin levels and carotid atherosclerosis in acute ischemic stroke patients. Int J Neurosci. 2018;128:237-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Santoro L, Schinzari F, Di Veronica A, Cardillo C, Santoliquido A. Carotid free-floating thrombus in woman with meningioma: a case report and review of the literature. Eur Rev Med Pharmacol Sci. 2015;19:1442-1445. [PubMed] [Cited in This Article: ] |
| 6. | Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Executive Summary: Heart Disease and Stroke Statistics--2016 Update: A Report From the American Heart Association. Circulation. 2016;133:447-454. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1864] [Cited by in F6Publishing: 1709] [Article Influence: 213.6] [Reference Citation Analysis (0)] |
| 7. | David Spence J. Advances in Stroke Prevention. J Transl Int Med. 2018;6:105-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Annambhotla S, Park MS, Keldahl ML, Morasch MD, Rodriguez HE, Pearce WH, Kibbe MR, Eskandari MK. Early versus delayed carotid endarterectomy in symptomatic patients. J Vasc Surg. 2012;56:1296-302; discussion 1302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Huibers A, Calvet D, Kennedy F, Czuriga-Kovács KR, Featherstone RL, Moll FL, Brown MM, Richards T, de Borst GJ. Mechanism of Procedural Stroke Following Carotid Endarterectomy or Carotid Artery Stenting Within the International Carotid Stenting Study (ICSS) Randomised Trial. Eur J Vasc Endovasc Surg. 2015;50:281-288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 10. | Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415-1425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2514] [Cited by in F6Publishing: 2198] [Article Influence: 84.5] [Reference Citation Analysis (0)] |
| 11. | Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379-1387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2359] [Cited by in F6Publishing: 1997] [Article Influence: 76.8] [Reference Citation Analysis (0)] |
| 12. | Musicant SE, Guzzetta VJ, Terramani TT, Greenwood KL, Chiodo WC, Heaney KM, Berthiaume SJ. Modified Eversion Carotid Endarterectomy (mECEA): Analysis of Clinical and Financial Outcomes. Ann Vasc Surg. 2017;42:16-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Powers WJ, Clarke WR, Grubb RL, Videen TO, Adams HP, Derdeyn CP; COSS Investigators. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA. 2011;306:1983-1992. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 540] [Cited by in F6Publishing: 526] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 14. | Li K, Liu YS, Wang F. One case of brachial artery stenting complicated with basilar artery embolization. Zhonghua Shenjing Waike Jibing Yanjiu Zazhi. 2015;14:84-85. [Cited in This Article: ] |
| 15. | Hüttl K, Nemes B, Simonffy A, Entz L, Bérczi V. Angioplasty of the innominate artery in 89 patients: experience over 19 years. Cardiovasc Intervent Radiol. 2002;25:109-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W; . Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF; CREST Investigators. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med. 2010;363:11-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2118] [Cited by in F6Publishing: 1941] [Article Influence: 138.6] [Reference Citation Analysis (0)] |
| 17. | Okahara M, Kiyosue H, Kashiwagi J, Ueda S, Hori Y, Mori H. Small in-stent Low Density on CT Angiography after Carotid Artery Stenting. Interv Neuroradiol. 2008;14 Suppl 2:41-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Hashimura N, Mutoh T, Matsuda K, Matsumoto K. Evaluation and management of plaque protrusion or thrombus following carotid artery stenting. Neurol Med Chir (Tokyo). 2015;55:149-154. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Lee JH, Kim BK, Seol DC, Byun SJ, Park KH, Sung IK, Park HS, Shim CS. Rescue endoscopic bleeding control for nonvariceal upper gastrointestinal hemorrhage using clipping and detachable snaring. Endoscopy. 2013;45:489-492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Bonati LH, Engelter ST, Lyrer PA. Carotid artery stenting. Swiss Med Wkly. 2012;142:w13619. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Rigatelli G, Zuin M, Dell'Avvocata F, Nanjundappa A, Daggubati R, Nguyen T. Non-invasive Evaluation of Fluid Dynamic of Aortoiliac Atherosclerotic Disease: Impact of Bifurcation Angle and Different Stent Configurations. J Transl Int Med. 2018;6:138-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Etxegoien N, Rhyne D, Kedev S, Sachar R, Mann T. The transradial approach for carotid artery stenting. Catheter Cardiovasc Interv. 2012;80:1081-1087. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Sfyroeras GS, Moulakakis KG, Markatis F, Antonopoulos CN, Antoniou GA, Kakisis JD, Brountzos EN, Liapis CD. Results of carotid artery stenting with transcervical access. J Vasc Surg. 2013;58:1402-1407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Bergeron P. Direct percutaneous carotid access for carotid angioplasty and stenting. J Endovasc Ther. 2015;22:135-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Alvarez B, Matas M, Ribo M, Maeso J, Yugueros X, Alvarez-Sabin J. Transcervical carotid stenting with flow reversal is a safe technique for high-risk patients older than 70 years. J Vasc Surg. 2012;55:978-984. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Ghosh J, Murray D, Farquharson F, Serracino-Inglott F. Abdominal aortic aneurysm repair: The carotid approach. J Vasc Surg. 2009;49:763-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Levy I, Binmoeller KF. EUS-guided vascular interventions. Endosc Ultrasound. 2018;7:228-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Sharma M, Singh P, Kirnake V, Toshniwal J, Chopra A. Dysphagia aortica: Emerging role of endoscopic ultrasound (with videos). Endosc Ultrasound. 2018;7:343-346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Zhang T, Wang F, Ji DH, Li C. Preliminary experience of using ProGlide vascular closure system in performing percutaneous endovascular aortic repair. Jieru Fangshexue Zazhi. 2016;25:664-667. [Cited in This Article: ] |
| 30. | Sanborn TA, Tomey MI, Mehran R, Généreux P, Witzenbichler B, Brener SJ, Kirtane AJ, McAndrew TC, Kornowski R, Dudek D, Nikolsky E, Stone GW. Femoral vascular closure device use, bivalirudin anticoagulation, and bleeding after primary angioplasty for STEMI: results from the HORIZONS-AMI trial. Catheter Cardiovasc Interv. 2015;85:371-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Smilowitz NR, Kirtane AJ, Guiry M, Gray WA, Dolcimascolo P, Querijero M, Echeverry C, Kalcheva N, Flores B, Singh VP, Rabbani L, Kodali S, Collins MB, Leon MB, Moses JW, Weisz G. Practices and complications of vascular closure devices and manual compression in patients undergoing elective transfemoral coronary procedures. Am J Cardiol. 2012;110:177-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Hermanides RS, Ottervanger JP, Dambrink JH, de Boer MJ, Hoorntje JC, Gosselink AT, Suryapranata H, Van't Hof AW; Zwolle Myocardial Infarction Study Group. Closure device or manual compression in patients undergoing percutaneous coronary intervention: a randomized comparison. J Invasive Cardiol. 2010;22:562-566. [PubMed] [Cited in This Article: ] |
| 33. | Jaffan AA, Prince EA, Hampson CO, Murphy TP. The preclose technique in percutaneous endovascular aortic repair: a systematic literature review and meta-analysis. Cardiovasc Intervent Radiol. 2013;36:567-577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Nelson PR, Kracjer Z, Kansal N, Rao V, Bianchi C, Hashemi H, Jones P, Bacharach JM. A multicenter, randomized, controlled trial of totally percutaneous access versus open femoral exposure for endovascular aortic aneurysm repair (the PEVAR trial). J Vasc Surg. 2014;59:1181-1193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 176] [Cited by in F6Publishing: 188] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 35. | Biancari F, D'Andrea V, Di Marco C, Savino G, Tiozzo V, Catania A. Meta-analysis of randomized trials on the efficacy of vascular closure devices after diagnostic angiography and angioplasty. Am Heart J. 2010;159:518-531. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 179] [Cited by in F6Publishing: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |