Published online Dec 6, 2018. doi: 10.12998/wjcc.v6.i15.1042
Peer-review started: September 12, 2018
First decision: October 11, 2018
Revised: October 18, 2018
Accepted: October 22, 2018
Article in press: October 22, 2018
Published online: December 6, 2018
We report a case of intermittent lower abdominal pain and distension accompanied by defecation difficulties for 3 years due to Chilaiditi syndrome in a 59-year-old male. Before admission to our hospital, the patient had undergone gastroscopy, which showed gastritis and duodenitis, and colonoscopy, which showed cecum deformation and cicatricial changes of the mucous membrane in the colon hepatic flexure. A computed tomography (CT) scan of the abdomen at our hospital confirmed right hepatic atrophy and interposition of the colon. Moreover, CT simulation endoscopy identified cystic dilatation in the colon hepatic flexure with the widest diameter of 8.2 cm. The patient was diagnosed with Chilaiditi syndrome. As the patient was unable to endure his defecation difficulties, he underwent a laparoscope-assisted right hemicolectomy. The patient had a good recovery. During the follow-up period of 9 mo, the patient remained symptom-free.
Core tip: We report a rare case of intermittent lower abdominal pain and distension accompanied by defecation difficulties due to Chilaiditi syndrome. The incidence of Chilaiditi syndrome is very low and is easily misdiagnosed. Imaging examination is an important diagnostic technique for Chilaiditi syndrome.
- Citation: Luo XG, Wang J, Wang WL, Yu CZ. Intermittent abdominal pain accompanied by defecation difficulties caused by Chilaiditi syndrome: A case report. World J Clin Cases 2018; 6(15): 1042-1046
- URL: https://www.wjgnet.com/2307-8960/full/v6/i15/1042.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i15.1042
The Chilaiditi sign refers to the abnormal interposition of the colon or small bowel between the liver and right diaphragm, which was first observed in a clinical examination by Cantini in 1865. Subsequently, Demetrius Chilaiditi, a Greek radiologist, reported three cases of hepatodiaphragmatic interposition in 1910. Soon afterwards, this abnormal condition was named Chilaiditi sign. Chilaiditi sign always exists in individuals without clinical symptoms and is often an incidental finding through chest or abdominal radiography. If the Chilaiditi sign is associated with other respiratory and digestive symptoms such as abdominal pain, constipation, vomiting, respiratory distress, anorexia, volvulus, intestinal obstruction and perforation in a patient, the name is designated as Chilaiditi syndrome. The incidental finding at clinical imaging examination is rare, with an incidence of 0.025%-0.28%[1], it is more prevalent in males than in females, with a ratio of 4:1, and the incidence rate increases with age[2], especially in the elderly and the mentally ill[3]. Chilaiditi sign and Chilaiditi syndrome are chronic but benign conditions. Due to the low incidence and lack of specificity in clinical manifestations, clinicians should pay careful attention while making diagnoses to avoid misdiagnosis and mistreatment.
Here, we report a rare case of a 59-year-old male who was initially diagnosed with colitis and constipation. The patient was finally diagnosed with Chilaiditi syndrome by computed tomography (CT) scan and underwent laparoscope-assisted right hemicolectomy.
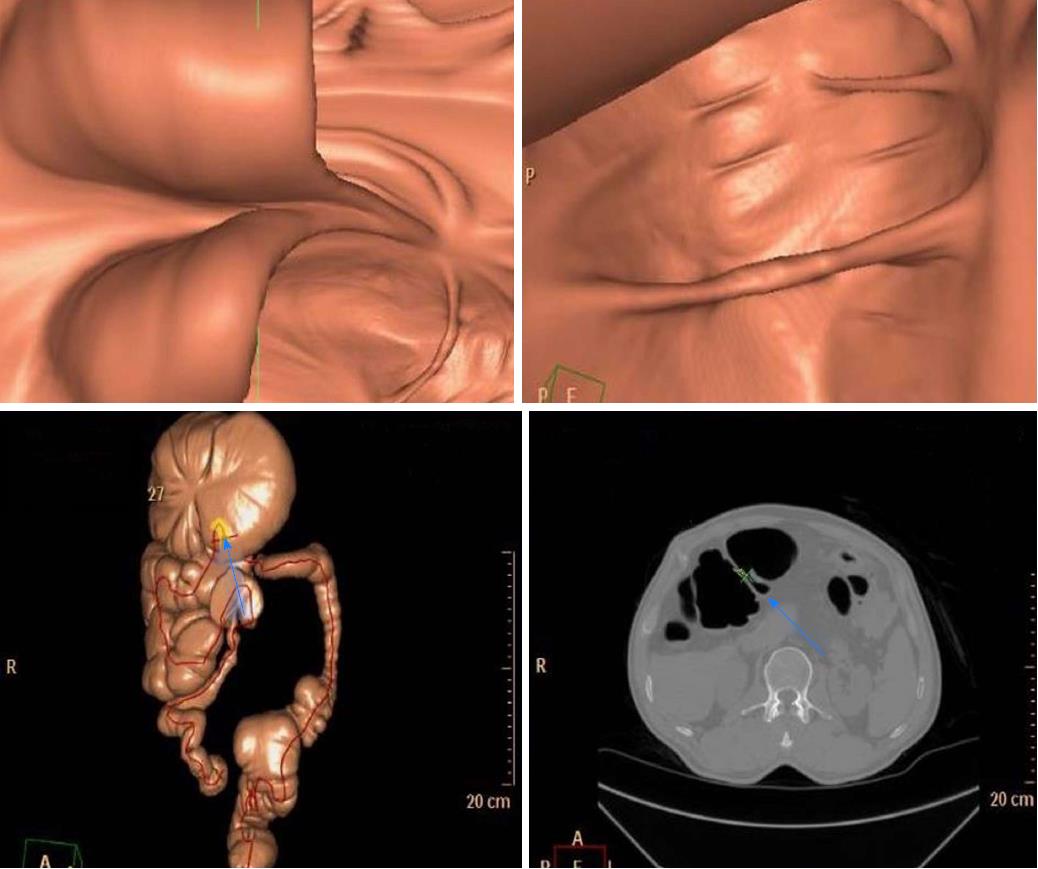
A 59-year-old male patient was admitted to the Department of General Surgery in the Second Affiliated Hospital of Nanjing Medical University (Nanjing, China) due to intermittent lower abdominal pain and distension accompanied by defecation difficulties for 3 years. These symptoms were initially relieved by laxatives but recently started to exacerbate. The patient denied nausea, vomiting, fever, melena and hematochezia. He had undergone several medical examinations including gastroscopy in another hospital, which showed gastritis and duodenitis. His colonoscopy showed cecum deformation and cicatricial changes of the mucous membrane in the colon hepatic flexure. The patient had never underwent surgery. There was nothing remarkable in his past medical and family histories. His vital signs were unremarkable. Upon physical examination, no obvious cardiovascular or respiratory system abnormalities were found. His abdomen was flat and soft. There were no signs of obvious pressure pain, rebound tenderness or abdominal mass. Murphy’s sign was negative. Auscultation revealed normal bowel sounds. Blood, urine, stool, as well as liver and kidney function tests, coagulation studies, and electrocardiograms were all unremarkable. Chest X-rays revealed an abnormal gas shadow in the right sub-phrenic space and a segment of gaseous distended colon, which was interposed between the liver and the right diaphragm. A CT scan of the abdomen confirmed right hepatic atrophy and interposition of the colon (Figure 1). Further imaging by CT simulation endoscopy identified a cystic dilatation in the colon hepatic flexure, where the maximum diameter was 8.2 cm. There was no evidence of bowel wall thickening or bowel obstruction (Figure 2). These findings, together with the symptoms this patient was experiencing, indicated that the patient has Chilaiditi syndrome. There was no urgent indication for surgery. However, the patient was unable to endure his defecation difficulties and finally underwent laparoscope-assisted right hemicolectomy. Postoperative recovery was uneventful. He was discharged after 14 d of hospitalization with close follow-up. During a 4-wk follow-up period, he reported complete resolution of abdominal pain and distension. Moreover, defecation improved due to ameliorated regularity of bowel movements. During the subsequent 9-mo follow-up period, the patient remained symptom-free.
Normally, upper abdominal anatomy, including the suspensory ligament of the liver, mesocolon, liver, and the falciform ligament, can maintain a suitable space around the liver. Under normal physiological conditions, it is impossible for interposition of the colon or other organs to occur. The change of the relationship between the colon, the small intestine and the diaphragm is generally due to changes in anatomy. As a result, this change contributes to the occurrence of Chilaiditi syndrome. Under the Chilaiditi sign or Chilaiditi syndrome condition, the colon hepatic flexure, ascending colon, transverse colon, and small bowel, either alone or in combination with the colon, are the most common interposed organs.
The etiology of Chilaiditi syndrome remains controversial[4] and multiple factors have been documented to contribute[5]. Congenital disorders that can lead to Chilaiditi syndrome include small or ptotic liver, deficient falciform ligament, deficient suspensory ligament and congenital malposition or malrotation of the colon, and redundant colon. Furthermore, acquired disorders that can lead to Chilaiditi syndrome include cirrhosis, degeneration of the diaphragm, paralysis of the phrenic nerve, increased intrathoracic pressure caused by emphysema or tuberculosis, and abnormal dilatation of the colon[6]. Some special groups including overweight individuals[7] and persons with high abdominal fat content[8] tend to have higher incidence in migration of the colon or small intestine. In addition, some operations concerning the liver can also cause Chilaiditi syndrome[9]. In our case, the cause of Chilaiditi syndrome is unclear, but the redundant colon and dilatation of colon at the hepatic flexure are presumed to relate to Chilaiditi syndrome. Although the Chilaiditi sign is asymptomatic, we must carefully consider the presence of gases under the diaphragm in chest radiographs. Careful monitoring of these patients is required, as they have the potential risk of perforation complications during various diagnostic and therapeutic processes, such as percutaneous liver biopsy, thoracentesis and colonoscopy[10]. When patients need liver puncture, B ultrasound or CT guidance is necessary to avoid potential intestinal perforation[11].
The diagnosis of Chilaiditi sign seems to be relatively easy because the interposition of the colon is occasionally found on chest films, abdominal plain films or B-ultrasounds, and this sign can be present temporarily or permanently[12]. When the condition is suspected, supplementary lateral chest radiographs, especially in the left decubitus position, are necessary. To differentiate from pneumoperitoneum, in which case patients require emergency surgery, gases can still be seen below the diaphragm in the left decubitus position when the body position is changed[13]. In spite of this, chest and abdominal radiography is still not as sensitive as CT scans for diagnosis[14].
Differential diagnosis including renal or biliary colic, sub-phrenic abscess, pneumoperitoneum or congenital diaphragmatic hernia must be considered in addition to Chilaiditi syndrome[15]. In rare cases, other intestinal diseases may also occur at the same time as Chilaiditi syndrome. There are several reports of intestinal perforation caused by Chilaiditi syndrome[1,16,17]. Under such complicated conditions, further CT scan imaging of the abdomen is recommended if necessary and will help clinicians make correct diagnoses[18]. Our patient was initially treated in other hospitals and was diagnosed with enteritis and constipation. Luckily, the patient did not receive secondary damage during colonoscopy examination. It was revealed that the colonic mucosa was flaky, striate, linear, with reticulate white scars, slightly higher than normal mucosa. With 3 years of conservative treatment in the outside institute, the symptoms of the patient appeared ingravescence. With the intention to avoid potential complications as a result of invasive examination, abdominal CT and CT simulation endoscopy were arranged in our hospital. The imaging by CT simulation endoscopy identified a cystic dilatation in the colon hepatic flexure with the widest diameter of 8.2 cm, which seemed to be similar to volvulus. Based on the CT manifestations and the absence of severe abdominal pain, vomiting, and fever, we excluded the diagnosis of intestinal volvulus, and the patient was finally diagnosed with Chilaiditi syndrome.
Chilaiditi syndrome generally does not require surgical intervention[19]. Management strategies for Chilaiditi syndrome consist of conservative treatment and surgical intervention. Conservative treatment based on different clinical symptoms is always effective, and these measures include bed rest, fluid therapy, gastrointestinal decompression, enemas, and stool softeners[15]. For obese patients, losing weight, which gradually decreases the frequency and intensity of the patient’s symptoms, is also a very important and effective method[7]. If conservative treatment is unsuitable or the patient has serious complications, such as intestinal obstruction, ischemia, volvulus and perforation[20], surgical intervention is recommended[21]. There are different operations for this syndrome, including transverse or right hemicolectomy, colopexy, and hepatopexy[22]. According to the literature, about 26% of all patients with Chilaiditi sign and Chilaiditi syndrome underwent surgical treatment, and stayed asymptomatic during different follow-up periods[14]. Recently, minimally-invasive surgery, such as laparoscopic surgery, is recommended[23], even to the extent that there is a report of robotic-assisted technique for the surgical management of Chilaiditi syndrome[24].
In the presented case, conservative treatment was first recommended because there were no symptoms of intestinal perforation, necrosis and volvulus. However, the patient complained that he could not tolerate long-term intermittent abdominal pain, distension and difficulty with defecation. He therefore demanded surgical treatment to resolve his symptoms. Based on the patient’s preference and given the long course of his condition, the patient underwent laparoscopic-assisted right hemicolectomy. With the preexsisting abdominal distention, an artificial pneumoperitoneum was created through a small open incision to avoid secondary injury during surgery. As a result, the patient had a good recovery.
Chilaiditi sign and Chilaiditi syndrome are two different states of the same condition. Now that interposition can be found in all patients, why is it that some patients are asymptomatic, while others are symptomatic? We speculate that patients with asymptomatic Chilaiditi sign may become symptomatic for Chilaiditi syndrome in the following situations: (A) sudden increased activity of the redundant colon; (B) increased bowel movements; (C) sudden gas increase in the intestine; and (D) severe increased pressure in the chest with cough in patients with pulmonary tuberculosis or empyema. At present, the etiological classification and pathogenesis of Chilaiditi syndrome are not elaborated thoroughly; therefore, more research should be encouraged to reveal the specific etiology and pathogenesis of Chilaiditi syndrome.
In conclusion, we present a rare case and highlight the importance of proper diagnosis and treatment for subdiaphragmatic gas. When gas is presented under the diaphragm, surgeons and medical students need to consider this syndrome routinely instead of performing emergency surgery as conventional medical education suggests. This condition is typically conservatively treated, and surgery is only required when the conservative treatment is invalid.
A 59-year-old male patient was admitted to our hospital due to intermittent lower abdominal pain and distension accompanied by defecation difficulties for 3 years.
Chilaiditi syndrome.
Renal or biliary colic, sub-phrenic abscess, pneumoperitoneum or congenital diaphragmatic hernia.
Computed tomography (CT) scan of the abdomen confirmed right hepatic atrophy and interposition of the colon. CT simulation endoscopy identified a cystic dilatation in the colon hepatic flexure with the widest diameter of approximately 8.2 cm.
Chilaiditi syndrome.
The patient underwent laparoscope-assisted right hemicolectomy.
The incidence of Chilaiditi syndrome is very low. Imaging examination is very important for differential diagnosis and can avoid unnecessary emergency operation. The main treatment is conservative treatment.
Chilaiditi sign refers to the abnormal interposition of the colon or small bowel between the liver and right diaphragm, Once Chilaiditi sign is associated with a variety of clinical respiratory and digestive symptoms, the name is designated as Chilaiditi syndrome.
Chilaiditi syndrome is rare. Due to its low incidence, Chilaiditi syndrome is easily misdiagnosed. Imaging examination is an important diagnostic technique in Chilaiditi syndrome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): E
P- Reviewer: Chiba T, Contini S, Kakisaka Y, Majbar AM, Shimizu Y, Wang YP, Wani IA S- Editor: Dou Y L- Editor: Filipodia E- Editor: Song H
| 1. | Aldoss IT, Abuzetun JY, Nusair M, Suker M, Porter J. Chilaiditi syndrome complicated by cecal perforation. South Med J. 2009;102:841-843. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Yin AX, Park GH, Garnett GM, Balfour JF. Chilaiditi syndrome precipitated by colonoscopy: a case report and review of the literature. Hawaii J Med Public Health. 2012;71:158-162. [PubMed] [Cited in This Article: ] |
| 3. | Joo YE. Chilaiditi’s sign. Korean J Gastroenterol. 2012;59:260-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Hountis P, Chounti M. Chilaiditi’s sign or syndrome? Diagnostic question in two patients with concurrent cardiovascular diseases. Monaldi Arch Chest Dis. 2017;87:775. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Gad MM, Al-Husseini MJ, Salahia S, Saad AM, Amin R. Chilaiditi syndrome - a rare case of pneumoperitoneum in the emergency department: a case report. J Med Case Rep. 2018;12:263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol (N Y). 2012;8:276-278. [PubMed] [Cited in This Article: ] |
| 7. | Sorrentino D, Bazzocchi M, Badano L, Toso F, Giagu P. Heart-touching Chilaiditi’s syndrome. World J Gastroenterol. 2005;11:4607-4609. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 12] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Farkas R, Moalem J, Hammond J. Chilaiditi’s sign in a blunt trauma patient: a case report and review of the literature. J Trauma. 2008;65:1540-1542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Jeng KS. Education and imaging. Hepatology: Chilaiditi sign after right hepatectomy for hepatocellular carcinoma. J Gastroenterol Hepatol. 2015;30:439. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Gurvits GE, Lau N, Gualtieri N, Robilotti JG. Air under the right diaphragm: colonoscopy in the setting of Chilaiditi syndrome. Gastrointest Endosc. 2009;69:758-759; discussion 759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Yamamoto K, Itoi T, Tsuchiya T, Tanaka R, Nagakawa Y. EUS-guided drainage of hepatic abscess in the right side of the liver of a patient with Chilaiditi syndrome. VideoGIE. 2017;2:299-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Uygungul E, Uygungul D, Ayrik C, Narci H, Bozkurt S, Köse A. Chilaiditi sign: why are clinical findings more important in ED? Am J Emerg Med. 2015;33:733.e1-733.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Evrengül H, Yüksel S, Orpak S, Özhan B, Ağladıoğlu K. Chilaiditi Syndrome. J Pediatr. 2016;173:260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Saber AA, Boros MJ. Chilaiditi’s syndrome: what should every surgeon know? Am Surg. 2005;71:261-263. [PubMed] [Cited in This Article: ] |
| 15. | Kang D, Pan AS, Lopez MA, Buicko JL, Lopez-Viego M. Acute abdominal pain secondary to chilaiditi syndrome. Case Rep Surg. 2013;2013:756590. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Acar T, Kamer E, Acar N, Er A, Peşkersoy M. Chilaiditi’s syndrome complicated by colon perforation: a case report. Ulus Travma Acil Cerrahi Derg. 2015;21:534-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Sunkara T, Rawla P, Yarlagadda KS, Baltazar GA, Gaduputi V. Chilaiditi Syndrome Complicated by Cecal Perforation in the Setting of Scleroderma. J Investig Med High Impact Case Rep. 2018;6:2324709618803387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Hussain S, Hussain S, Hussain S. Chilaiditi Syndrome-What’s Air Doing There? J Emerg Med. 2018;55:e131-e132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Esperto H, Ruivo C, Ferreira E. Chilaiditi’s sign. Acta Med Port. 2013;26:71. [PubMed] [Cited in This Article: ] |
| 20. | Correa Jiménez O, Buendía De Ávila M, Parra Montes E, Davidson Córdoba J, De Vivero Camacho R. Chilaiditi’s sign and syndrome: rare conditions but diagnostically important in pediatrics. Clinical cases. Rev Chil Pediatr. 2017;88:635-639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Williams A, Cox R, Palaniappan B, Woodward A. Chilaiditi’s syndrome associated with colonic volvulus and intestinal malrotation-A rare case. Int J Surg Case Rep. 2014;5:335-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Mateo de Acosta Andino DA, Aberle CM, Ragauskaite L, Khair G, Streicher A, Bartholomew J, Kacey D. Chilaiditi syndrome complicated by a closed-loop small bowel obstruction. Gastroenterol Hepatol (N Y). 2012;8:274-276. [PubMed] [Cited in This Article: ] |
| 23. | Takahashi K, Ito H, Katsube T, Tsuboi A, Hashimoto M, Ota E, Mita K, Asakawa H, Hayashi T, Fujino K. Treatment of Chilaiditi syndrome using laparoscopic surgery. Asian J Endosc Surg. 2017;10:63-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Garcia O, Rayhrer C. Surgical management of Chilaiditi syndrome with da Vinci® robotic system. Int J Surg Case Rep. 2017;41:450-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |