Published online Dec 6, 2018. doi: 10.12998/wjcc.v6.i15.1029
Peer-review started: July 5, 2018
First decision: October 4, 2018
Revised: November 4, 2018
Accepted: November 14, 2018
Article in press: November 15, 2018
Published online: December 6, 2018
A floating shoulder may be associated with catastrophic neurovascular injury and requires a multidisciplinary approach for its management. To maximize the likelihood of good patient outcomes, this unique injury pattern should be recognized in patients as early as possible. This can be difficult to achieve, however, as there are currently few reports of floating shoulder in the literature, meaning that associated neurovascular injuries may be overlooked.
We present here a rare case of floating shoulder with axillary artery injury in a 34-year-old woman. The patient complained of pain and numbness of her left upper limb after losing control of her motorcycle on a highway and falling from the vehicle 2 h ago. No blood pressure reading could be obtained from her left upper limb and no blood oxygen readings could be obtained from any of her left fingers. Computed tomography angiography and duplex ultrasonography revealed interruption of blood flow through the axillary artery, with distal flow being maintained through collateral arteries. The clinical diagnosis including fracture of the left proximal humerus, the left clavicle, and the left scapula, left axillary artery rupture, and left brachial plexus injury. We successfully performed open reduction and internal fixation of the fracture and vascular repair. The patient showed satisfactory recovery that was observed during 4-mo follow-up.
Emergency surgery can be an effective therapeutic option for the closed floating shoulder with catastrophic axillary artery injury.
Core tip: A floating shoulder with catastrophic neurovascular injury may be overlooked, as there are currently few reports in the literature. This case report describes that brachial plexus and axillary artery injury by the distal fragment of the clavicle in a closed floating shoulder, and we successfully performed open reduction and internal fixation of the fracture and vascular repair.
- Citation: Chen YC, Lian Z, Lin YN, Wang XJ, Yao GF. Injury to the axillary artery and brachial plexus caused by a closed floating shoulder injury: A case report. World J Clin Cases 2018; 6(15): 1029-1035
- URL: https://www.wjgnet.com/2307-8960/full/v6/i15/1029.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i15.1029
A floating shoulder is a fracture of the scapular neck with ligament disruption, and may or may not involve a clavicular fracture[1,2]. It is often associated with catastrophic neurovascular injury[1-5] and requires a multidisciplinary approach for its management. To maximize the likelihood of good patient outcomes, this unique injury pattern should be recognized in patients as early as possible. This can be difficult to achieve, however, as there are currently few reports of floating shoulder in the literature, meaning that associated neurovascular injuries may be overlooked[5]. We herein report a case involving injury to the axillary artery and brachial plexus caused by a closed floating shoulder injury. Based on a review of the current literature, we suggest how early diagnosis and effective treatment of this uncommon injury can be achieved.
A 34-year-old, 80-kg, and alcohol-intoxicated East Asian woman presented to our emergency department after losing control of her motorcycle on a highway and falling from the vehicle (Figure 1). While the patient did occasionally drink, her drinking history was otherwise unremarkable. She also did not smoke and had no history of drug addiction or chronic disease, and was overall a healthy woman. At presentation, pain and swelling of her left shoulder were evident. She also complained of numbness of her left upper limb. Her vital signs upon arrival were as follows: Blood pressure, 135/95 mmHg; heart rate, 82 beats per minute; and respiratory rate, 19 breaths per minute. No blood pressure reading could be obtained from her left upper limb and no blood oxygen readings could be obtained from any of her left fingers. Her Glasgow Coma Scale score was 15.
Closer examination of the patient revealed that capillary refill of all left-hand fingers was disturbed, although the patient’s left arm and hand were warm and radial and ulnar pulses at the wrist were absent. Movement of her left shoulder, elbow, and wrist was also restricted along with a local shoulder injury. However, no bruit could be detected. Laboratory results, including complete blood count, electrolytes, and coagulation panels, were also normal, with hemoglobin and hematocrit results of 13.0 g/dL and 38.4%, respectively.
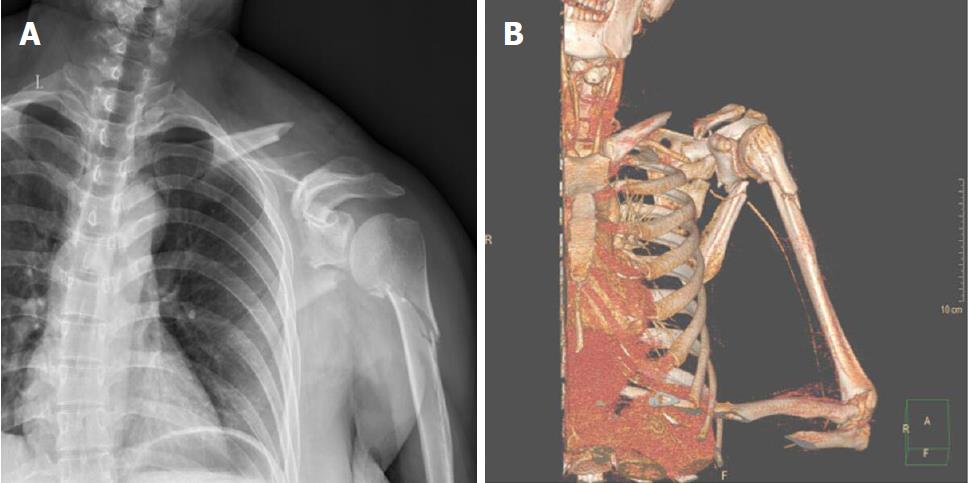
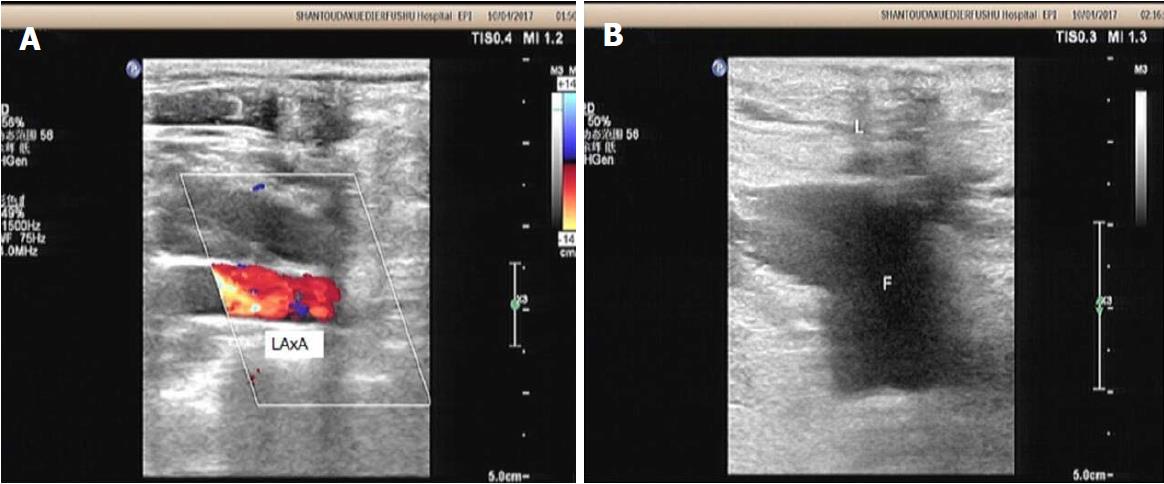
Plain anterior-posterior radiographs and computed tomography (CT) images were subsequently taken (Figure 2), which revealed multiple fractures of the scapular area, implying that it is a floating shoulder injury. Injuries included a fracture of the left clavicle at the middle third and downward displacement of the distal fragment, a displaced comminuted fracture of the left scapula, and a displaced comminuted fracture of the left proximal humerus. In addition, CT angiography (Figure 2) and duplex ultrasonography (Figure 3) revealed interruption of blood flow through the axillary artery, with distal flow being maintained through collateral arteries. During observation, the patient reported increasing numbness and coldness of her left arm. To avoid limb-threatening irreversible ischaemia and amputation, it was decided that emergency vascular repair surgery should be performed immediately.
A 34-year-old woman presented to the hospital with 2 h of persistent pain and swelling of her left shoulder and numbness of her left upper limb after losing control of her motorcycle on a highway and falling from the vehicle.
Fracture of the left proximal humerus, left clavicle, and left scapula, left axillary artery rupture, and left brachial plexus injury.
The differential diagnoses included arterial thrombosis and compression. Complete blood count, electrolytes, and coagulation panels, were also normal, with hemoglobin and hematocrit results of 13.0 g/dL and 38.4%, respectively. X-ray and CT images displayed multiple fractures of the shoulder that were indicative of a floating shoulder injury. In addition, CT angiography and duplex ultrasonography revealed interruption of blood flow through the axillary artery, with distal flow being maintained through collateral arteries.
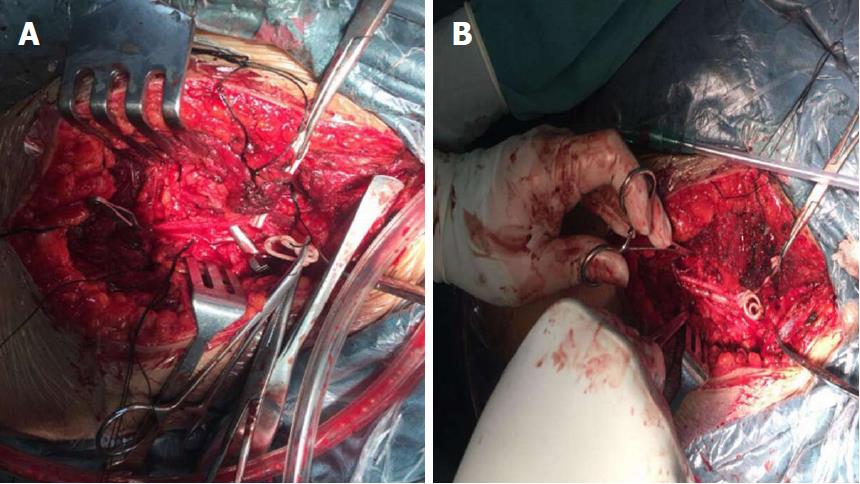
Emergency surgical exploration revealed that the axillary artery was completely amputated by the distal fragment of the left clavicle, and that the brachial plexus had suffered contusions (Figure 4). The proximal axillary artery was also completely occluded by a thrombus that had formed over a tear in the tunica intima. End-to-end anastomoses were thus performed, resulting in shortening of the artery by about 2 cm after excision of traumatized vessel segments (Figure 4). One-stage reconstruction with placement of a locking plate was then performed to treat the patient’s clavicle fracture. The displaced comminuted fracture of the left proximal humerus was treated during the second-stage operation 3 wk after the initial injury (after angiogenesis). The fracture of the scapula was not surgically treated.
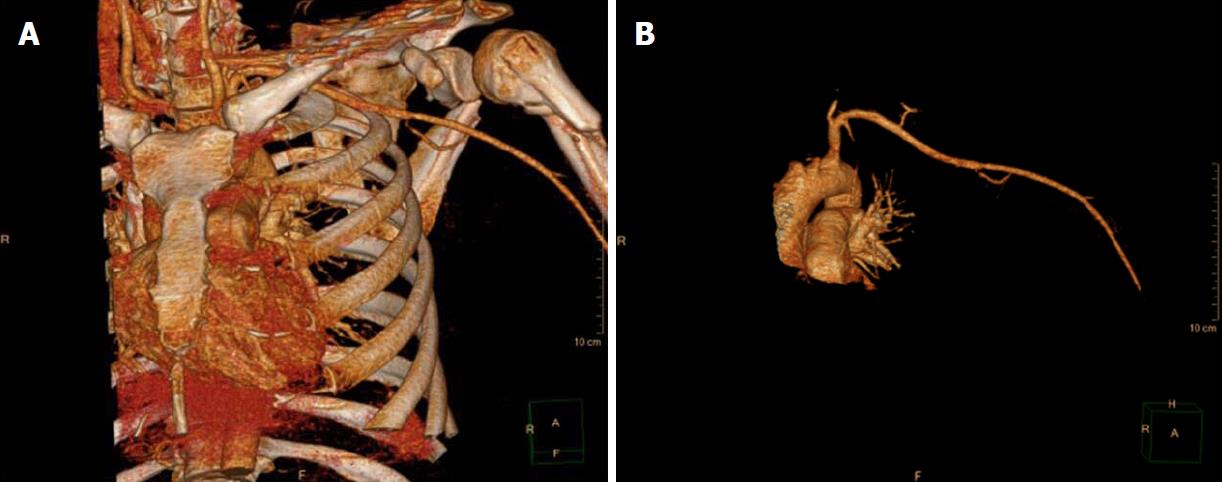
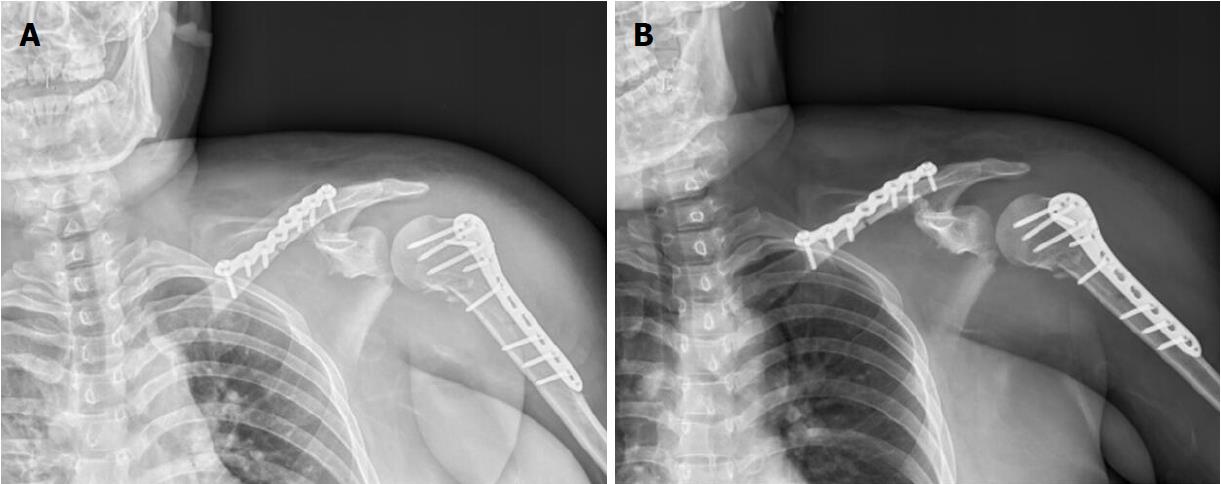
Revascularization of the patient’s upper extremity was achieved by emergency surgery about 10 h after the initial injury. Specifically, the patient’s radial and ulnar pulses were restored, and CT angiography confirmed that blood flow was uninterrupted (Figure 5). Furthermore, the blood oxygen concentration of her left upper extremity was 100% and systolic blood pressure measurements were equal in both arms. Postoperative X-ray showed that reduction and internal fixation results were satisfactory (Figure 6). Regarding the injury to the brachial plexus, emergency surgical exploration revealed that the brachial plexus had suffered contusions, and preoperative and postoperative neurological examinations revealed paresthesia resulting from brachial plexus contusion. Before the operation, the patient did not undergo electromyography and magnetic resonance examination due to emergency surgery. The patient was not willing to undergo electromyography and magnetic resonance examination after initial vascular reconstruction. And the patient left our city after discharge before the wound healed. We can only follow her by telephone. During the follow-up period, the patient refused to undergo electromyography and magnetic resonance examination in her city. Three months after injury, the fingers of the left hand can move freely; the movement of the left shoulder, elbow, and wrist became more and more flexible and free; the numbness of the left upper limb was reduced; the strength of the left upper limb was significantly better than before; and she was able to take care of her daily life. At the 4th month of follow-up, the patient felt that the movement, numbness, and strength of the left upper limb were better than before. After the fourth month of follow-up, the patient could not be contacted by telephone and the follow-up was completed, although we have been trying to contact this patient. Overall, the patient showed satisfactory recovery that was observed during 4-mo follow-up.
Fracture of the left proximal humerus, left clavicle, and left scapula, left axillary artery rupture, and left brachial plexus injury.
Emergency surgical exploration revealed that the axillary artery was completely amputated by the distal fragment of the left clavicle, and that the brachial plexus had suffered contusions. End-to-end anastomoses were thus performed. One-stage reconstruction with placement of a locking plate was then performed to treat the patient’s clavicle fracture. The displaced comminuted fracture of the left proximal humerus was treated during the second-stage operation 3 wk after the initial injury (after angiogenesis). The fracture of the scapula was not surgically treated.
At the 4th month of follow-up, the patient felt that the movement, numbness and strength of the left upper limb were better than before. Overall, the patient showed satisfactory recovery that was observed during 4-mo follow-up.
Since Ganz and Noesberger’s first statement of the pathologic anatomy of the floating shoulder, its defining characteristics have been revised by other authors[2,6,7]. Herscovici et al[7] defined the floating shoulder as an ipsilateral clavicle fracture with a scapular neck fracture. Goss et al[6] stated the definition of the superior shoulder suspensory complex (SSSC), and extended the description of a floating shoulder comprising the SSSC. Egol et al[8] suggested that a floating shoulder injury involves ipsilateral acromioclavicular joint dislocation with a scapular neck fracture. The most comprehensive definition of a floating shoulder was put forward by Vogels, who asserted that the following fractures of the scapular region are suggestive of this injury: A fracture of the left clavicle at the middle third and downward displacement of the distal fragment, a displaced comminuted fracture of the left scapula, and a displaced comminuted fracture of the left proximal humerus[9]. Despite this progress in understanding, the unified definition of a floating shoulder is still considerably ambiguous, probably because it is a rare injury complex[2].
Indeed, floating shoulder has an incidence rate of approximately 0.10% among trauma patients[10]. It is typically caused by the infliction of high-energy blunt force on the shoulder during road traffic accidents. Consequently, it is associated with a broad range of injuries, with affected patients presenting with a mean of 3.9 co-injuries[11]. The most common co-injuries are those associated with the ipsilateral upper limb, shoulder girdle, brachial plexus, and chest (e.g., rib fractures, blood pneumothorax, and pulmonary contusion), and have an overall incidence of 44%-100% among floating shoulder patients[12]. Of these injuries, chest trauma is the most common (rib fractures, 38%-45%; pulmonary contusion, pneumo- or haematothorax, 15%-50%)[11]. Other common injuries associated with floating shoulder include head injuries (20%), ipsilateral clavicle fractures (15%-40%), and ipsilateral humeral head fractures (12%)[11]. In addition, injuries to the brachial plexus, axillary artery, and subclavian vein can occur[11]. Patient morbidity is highly dependent on the severity of these associated injuries, especially in the presence of neurovascular injuries, which occur in about 10%–12% of floating shoulder patients[11]. A number of these co-injuries occurred in our patient, including a head injury, ipsilateral clavicle fractures, ipsilateral proximal humerus fractures, and injury to the axillary artery and the brachial plexus.
Despite the anatomic proximity of the axillary artery to the clavicle, scapula, and proximal humerus, its injury is rare. There are few reported cases of axillary artery injury following closed trauma in the literature[13]; indeed, we were only able to find a few reports of axillary artery and brachial plexus injury in the English-language literature. In these reports, these injuries mainly resulted from proximal humeral, humeral neck, and rib fractures, shoulder and glenohumeral dislocation, open shoulder injury, and iatrogenic injury. Thus, to the best of our knowledge, this is the first report of axillary artery and brachial plexus injury after an injury pattern such as that described in our patient.
The axillary artery is a continuation of the subclavian artery and is divided into three sections based on its location relative to the pectoralis minor muscle. The first section is defined as the part of the artery superior to the pectoralis minor muscle, the second section lies posterior to the pectoralis minor muscle, and the third section comprises the part of the artery inferior to the pectoralis minor. Although injury can occur anywhere along the course of the artery, previous reports have documented a high rate of injury to its third section. It has been speculated that this is because the axillary artery is fixed and bent by other branch arteries and the humeral head[14]. Injury to the artery may therefore be caused by penetrating sharp bone fragments, overstretching of the vessel, entrapment of the artery within the fracture site, contusion by the humeral head that leads to abrasion of the intima, or even delayed axillary artery thrombosis after a proximal humeral fracture[9]. However, in our patient, the injury occurred in the first section of the axillary artery, and we are inclined to suggest that injury to this section and the brachial plexus resulted from penetration by a distal clavicle fragment.
When arterial injury occurs with a floating shoulder injury, the vascular anatomy of the shoulder has an important role in patient outcome, since any disruption of vascular supply can jeopardize the viability of the entire limb. The main symptoms of ischemia (i.e., paralysis, paresthesia, pain, pallor, and pulselessness) do not always appear in all patients with an injury to the axillary artery because of well-developed collateral vessels around the shoulder joint[14]. Extensive connections among the suprascapular artery, the subscapular artery, and other arteries supply adequate amounts of blood to the distal limb. Therefore, axillary artery injury sites that are near to the origin of the subscapular artery may not impair blood supply to the upper limb. In contrast, injury sites distal to the subscapular artery will most likely result in ischemia of the limb[14].
Axillary artery injuries are also commonly associated with injury to the brachial plexus, with the latter occurring in up to 43% of patients with axillary artery injury[13]. Due to the proximity of the axillary artery and the brachial plexus, the area is predisposed to hemorrhagic lesions, brachial plexus compression, and subsequent ischemia[13]. Vascular occlusion alone can also produce permanent neurological damage; thus, minimizing diagnostic time is vital[13]. However, neurological injuries are most frequently caused by the direct infliction of injury on nerve structures by sharp bone fragments[13], with neurological lesions such as these principally affecting patient functional outcomes[13,15].
This case report informs clinical practice guidelines of floating shoulder with arterial injury. Emergency surgery is recommended in cases of vascular compromise[16]. The gold standard for treatment includes open reduction and internal fixation of fractures and vascular reconstruction when the lesion is clinically significant or visible by angiography[13]. Ischemia time and the general condition of the patient determine the order and type of definitive treatment that is to be run[13]. In the case of short ischemic time or only mild ischemia of the limb, a quick reduction and definitive fixation of the fracture may be beneficial. If the ischemia is severe or prolonged, vascular repair is preferred over orthopedic surgery and must be performed immediately. It is recommended that a stable surgical field through prior internal fixation of the fracture be obtained to avoid new injuries and facilitate vascular reconstruction. However, in patients with hemodynamic instability or in patients with ischemia for more than 8 h, quick reduction and temporary fixation, and prior revascularization and subsequent osteosynthesis definitive fixation for fractures are instead recommended[13,17]. The type of vascular repair depends on the type of arterial injury, with possible procedures including thrombectomy, endarterectomy, primary repair, saphenous vein interposition grafting, term-terminal anastomosis, vascular prosthesis[13], and more recently, endovascular techniques. Forearm compartment syndrome may also occur if ischemia time is greater than 6-8 h. In these cases, prophylactic fasciotomies and strict monitoring of compartment pressures should be carried out[13].
To prevent prolonged ischemia, and in turn devastating results such as upper limb amputation and patient death, early diagnosis and treatment of vascular lesions are necessary. We therefore suggest a testable hypothesis that when weak pulsation of the radial and ulnar arteries is observed in a patient with multiple shoulder fractures or shoulder dislocation, the axillary artery injury should be suspected. However, axillary artery injury is difficult to diagnose in some cases. Repeated neurovascular evaluations, along with complementary studies such as Doppler ultrasound and CT angiography or other angiography tests, are essential for diagnosing ischemia. In particular, Doppler ultrasonography can be useful for quantifying the weakness of pulsation. Catheter-based CT angiography can be used to detect damaged areas, and it can facilitate arterial repair by placing stent grafts at the same time. If this fails, open surgical treatment involving direct anastomosis, vein grafting, or artificial vessel grafting should be considered.
The complications of axillary artery and brachial plexus injuries following shoulder trauma are rare but can have serious consequences. This case report stresses the importance of suspecting catastrophic neurovascular injuries in any kind of shoulder trauma, and more importantly, axillary artery injury that can lead to a seriously ischemic limb. The state of the blood vessels should be assessed periodically after the fracture, as the pulse may disappear and ischemic symptoms may appear after a few days. If vascular injury is suspected, early diagnosis and accurate treatment are essential.
There were several strengths in our approach to this case: (1) rapid diagnosis of a floating shoulder with axillary artery injury by detailed physical examination, X-ray, duplex ultrasonography, and CT angiography; (2) perfect collaboration among multiple departments, such as emergency departments, orthopedics, radiology, ultrasound, laboratory, electrocardiogram, vascular surgery, and operating room, in order to race against time; and (3) successful revascularization by emergency surgery. The limitations in our approach to this case included: (1) there was too little evidence about brachial plexus injury; (2) EMG and MRI were not performed before or after surgery; (3) the follow-up period was too short, and the data of follow-up was too small, such as postoperative imaging examination, postoperative vascular examination, and evaluation of brachial plexus recovery.
We emphasize that catastrophic neurovascular injuries can occur with floating shoulder injuries. Therefore, they need to be identified and coordinated by a multidisciplinary team of orthopaedics, trauma and vascular surgeons. We also advise against any attempt at closed reduction of floating shoulder injuries with a pulseless limb as this can have potentially grave consequences; open surgery should instead be indicated without delay with consultation of a vascular surgeon. With swift and proper treatment, the prognosis for patients is good. However, final outcomes are compromised and determined by neurologic morbidity from concomitant brachial plexus injuries. The complications of axillary artery and brachial plexus injuries after shoulder trauma are rare, but can have serious consequences. This case report highlights the importance of suspecting catastrophic neurovascular injury in any type of shoulder trauma, and more importantly, axillary artery injury can result in severe ischemic limbs. The vascular status should be assessed periodically after the fracture, as the pulse may disappear and symptoms may appear after a few days. Early diagnosis and accurate treatment are necessary if vascular injury is suspected.
We thank our coworkers of the departments of emergency, orthopedics, radiology, ultrasound, laboratory, electrocardiogram, vascular surgery, and operating room for their invaluable technical help.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kvolik S, Malik H S- Editor: Ji FF L- Editor: Wang TQ E- Editor: Tan WW
| 1. | Heng K. “Floating shoulder” injuries. Int J Emerg Med. 2016;9:13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Wright DE, Johnstone AJ. The floating shoulder redefined. J Trauma. 2010;68:E26-E29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Gallucci G, Ranalletta M, Gallucci J, De Carli P, Maignon G. Late onset of axillary artery thrombosis after a nondisplaced humeral neck fracture: a case report. J Shoulder Elbow Surg. 2007;16:e7-e8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Labler L, Platz A, Weishaupt D, Trentz O. Clinical and functional results after floating shoulder injuries. J Trauma. 2004;57:595-602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Owens BD, Goss TP. The floating shoulder. J Bone Joint Surg Br. 2006;88:1419-1424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 152] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Herscovici D Jr, Fiennes AG, Allgöwer M, Rüedi TP. The floating shoulder: ipsilateral clavicle and scapular neck fractures. J Bone Joint Surg Br. 1992;74:362-364. [PubMed] [Cited in This Article: ] |
| 8. | Egol KA, Connor PM, Karunakar MA, Sims SH, Bosse MJ, Kellam JF. The floating shoulder: clinical and functional results. J Bone Joint Surg Am. 2001;83-A:1188-1194. [PubMed] [Cited in This Article: ] |
| 9. | Vogels J, Pommier N, Cursolle JC, Belin C, Tournier C, Durandeau A. PreFix™ external fixator used to treat a floating shoulder injury caused by gunshot wound. Chir Main. 2014;33:370-374. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Gilde AK, Hoffmann MF, Sietsema DL, Jones CB. Functional outcomes of operative fixation of clavicle fractures in patients with floating shoulder girdle injuries. J Orthop Traumatol. 2015;16:221-227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Südkamp NP, Jaeger N, Bornebusch L, Maier D, Izadpanah K. Fractures of the scapula. Acta Chir Orthop Traumatol Cech. 2011;78:297-304. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 176] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Ramos L, Mencía R, Alonso A, Ferrández L. Conservative treatment of ipsilateral fractures of the scapula and clavicle. J Trauma. 1997;42:239-242. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Bucci G, Lucar-López G, Sanchez-Gonzalez J, Malagelada F, Palencia Lopez J, Guevara-Noriega KA. Axillary artery injury and brachial plexus palsy as a complication of proximal humerus fractures. J Orthop. 2017;14:340-341. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Inui A, Kokubu T, Fujioka H, Toyokawa N, Nakagiri K, Doita M, Kurosaka M. Shoulder fracture dislocation associated with axillary artery injury: a case report. J Shoulder Elbow Surg. 2009;18:e14-e16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Cotman SJ, Trinh TQ, Vincent S, Backes JR. Proximal Humerus Fracture-Dislocation with Laceration of the Axillary Artery: A Case Report. Iowa Orthop J. 2017;37:53-55. [PubMed] [Cited in This Article: ] |
| 16. | Wenger JD, Olsson CJ. Acute limb ischemia after a proximal humeral epiphyseal fracture: intraoperative findings of an illustrative vascular lesion. J Shoulder Elbow Surg. 2011;20:e1-e3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Yagubyan M, Panneton JM. Axillary artery injury from humeral neck fracture: a rare but disabling traumatic event. Vasc Endovascular Surg. 2004;38:175-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |