Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.791
Peer-review started: July 23, 2018
First decision: August 30, 2018
Revised: November 2, 2018
Accepted: November 7, 2018
Article in press: November 7, 2018
Published online: November 26, 2018
Meckel’s diverticulum (MD) occurs predominantly in children and adolescents. It is rarely diagnosed in adults. Preoperative diagnosis is difficult due to low sensitivity of the radiological imaging studies. The role of video capsule endoscopy (VCE) in the diagnosis of MD is unknown, and the endoscopic patterns are not defined. We will describe four of our cases of MD evaluated with VCE and make a review of the literature focusing on the endoscopic characteristics.
We present four cases of MD confirmed by surgery. They were all adult males with ages going from 18 to 50 years, referred to our service from 2004 to 2018, due to obscure gastrointestinal bleeding (OGIB). They had a history of 1 mo to 10 years of overt and occult bleeding episodes. Laboratory blood test showed an iron-deficiency anemia from 4 to 9 g/dL of hemoglobin that required multiple hospitalizations and blood transfusions in all cases. Repeated upper digestive endoscopies and colonoscopies were negative. Small bowel was examined with VCE, which revealed double lumen images in all cases, one with polyps and three with circumferential ulcers in the diverticulum. However, based on VCE findings, preoperative diagnosis of MD was suggested only in two patients. Capsule was retained in one patient, which was recovered with surgery. The anatomopathological report revealed ulcerated ectopic gastric mucosa in all cases.
VCE is useful for the diagnosis of MD. However, endoscopic characteristics must be recognized in order to establish preoperative diagnosis.
Core tip: Preoperative diagnosis of Meckel’s diverticulum (MD) is practically nonexistent due to the low sensitivity of imaging studies. Video capsule endoscopy (VCE) allows direct examination of the small bowel. However, few publications report evaluating the role of VCE on diagnosis of MD, and the endoscopic characteristics have not been defined. For the above-mentioned, it is highly probable that this disease is under-diagnosed. In this literature review, we focus on the endoscopic features of MD by VCE, and in its clinical and pathological characteristics. Recognition of endoscopic features will increase preoperative diagnosis of this disease.
- Citation: García-Compeán D, Jiménez-Rodríguez AR, Del Cueto-Aguilera ÁN, Herrera-Quiñones G, González-González JA, Maldonado-Garza HJ. Meckel’s diverticulum diagnosis by video capsule endoscopy: A case report and review of literature. World J Clin Cases 2018; 6(14): 791-799
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/791.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.791
Meckel’s diverticulum (MD) is the most frequent gastrointestinal malformation. This condition arises from the incomplete involution of the omphalomesenteric duct[1] and is located in the antimesenteric region, in the last 60 to 100 cm of the ileum. Prevalence of MD has been estimated at 2% in the general population[1,2]. It predominates in male children and adolescents and is rarely diagnosed in adults[3]. This prevalence, however, could be significantly underestimated, since MD is asymptomatic in most cases. Only about 16% of cases may present clinical manifestations, with gastrointestinal bleeding (GIB) being the most frequent one[4]. On the other hand, most radiological studies, such as computerized tomography (CT) or magnetic resonance imaging, abdominal ultrasound, barium intestinal transit and mesenteric angiography, have poor diagnostic sensitivity[5]. It has been reported that technetium-99m pertechnetate scintigraphy (Meckel’s Scan) has moderate diagnostic sensitivity in children and adolescents, and poor sensitivity in adults[5]. Therefore, the preoperative diagnosis of MD is practically nonexistent in most cases.
Currently, it is expected that the use of new techniques enabling the direct revision of small intestine mucosa, such as video capsule endoscopy (VCE) and balloon enteroscopy, can increase preoperative diagnosis of MD. Despite the fact that VCE was approved for clinical use in 2000, nowadays there is scarce literature regarding its usefulness in the diagnosis of MD and endoscopic characteristics of this entity.
In view of the foregoing, we decided to report a case series of MD evaluated with VCE and to analyze clinical, demographic and anatomopathological characteristics, together with similar published cases through a review of the literature, emphasizing the endoscopic findings.
Chief complaints: A 20-year-old male who was referred to our unit in 2004 with a 3-year history of anemic syndrome.
History of present illness: He had suffered anemic syndrome for 3 years, treated with blood transfusions and intravenous iron. He did not have abdominal symptoms.
History of past illness: He had no history of past comorbidities.
Physical examination upon admission: On physical examination, he was pale and did not show hemodynamic instability.
Laboratory examinations: The laboratory blood tests showed an iron-deficiency anemia (hemoglobin: 4 g/dL).
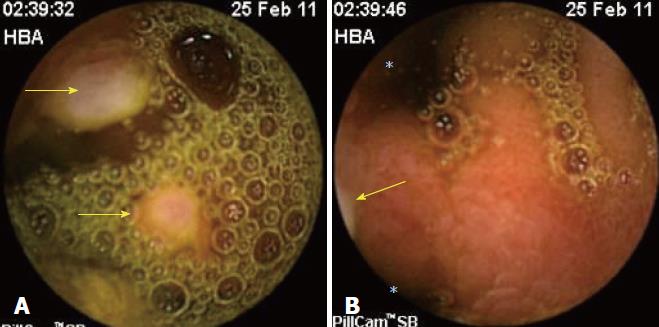
Imaging examinations: Previously, the patient had undergone four upper digestive endoscopies (UDEs), one colonoscopy and one barium intestinal transit, with non-relevant results. It was decided to examine the small intestine with a VCE, which showed an image with circumferential ulcers in the ileum. A diagnosis of ulcerated enteropathy of undetermined etiology was suggested. The retrospective review of the VCE images showed typical images of the MD (double lumen), which had gone unnoticed by the endoscopist (Figure 1). A Meckel’s Scan was then performed, which was positive. A surgical intervention was decided by laparoscopy.
Chief complaints: A 50-year-old male was referred to our unit in 2011 due to one-month history of hematochezia.
History of present illness: He had suffered hematochezia for 1 mo. He did not complain of abdominal pain.
History of past illness: He had no history of relevant comorbidities. He denied the use of nonsteroid anti-inflammatory drugs.
Physical examination upon admission: He presented only paleness of teguments and no hemodynamic instability.
Laboratory examinations: Laboratory blood tests showed an iron-deficiency anemia (hemoglobin: 9 g/dL).
Imaging examinations: UDE and colonoscopy performed during current hospitalization were both negative. It was considered adequate to evaluate the small intestine with VCE, which showed ulcerated polyps in a circumferential structure in the ileum (Figure 2A). Images with double lumen (Figure 2B) were found through retrospective review of VCE study; the gastrointestinal endoscopist before surgery had not noticed such images.
Since there was no conclusive diagnosis, a laparotomy was performed.
Chief complaints: An 18-year-old male was referred to our unit in 2017 with a 9-year history of recurrent episodes of hematochezia and anemia (hemoglobin: 4 g/dL).
History of present illness: He had suffered recurrent episodes of hematochezia and anemia for 9 years, which required multiple hospitalizations and blood transfusions. Two UDEs, two colonoscopies and one CT-enterography, which were performed in the last 3 years, showed negative results.
History of past illness: He did not present past comorbid conditions.
Physical examination upon admission: On examination, he was pale and did not show hemodynamic instability. He did not have abdominal complaints.
Laboratory examinations: Laboratory blood tests showed an iron-deficiency anemia (hemoglobin: 4 g/dL).
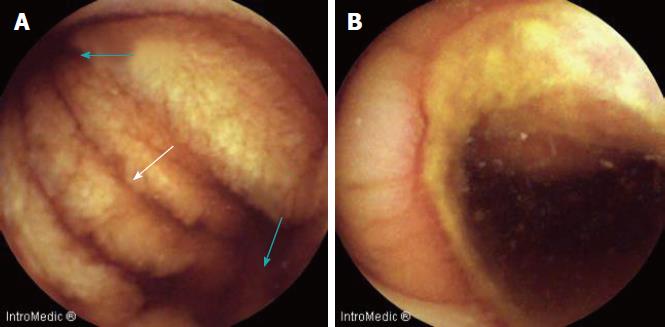
Imaging examinations: A review of the small intestine with VCE was performed, which showed a double lumen image with circumferential ulcerations (Figure 3). The capsule was retained in this place until the battery was consumed after 10 h from the beginning of the procedure. The probable diagnosis of MD was suggested. A plain abdominal radiography, which was performed 7 d later, showed VCE retention. An abdominal CT scan showed the presence of a diverticulum in the ileum, with the capsule lodged inside it. Meckel’s Scan was negative. The patient underwent laparoscopy.
Chief complaints: A 24-year-old male was referred to our unit in 2018 with a 10-year history of iron-deficiency anemia and hematochezia.
History of present illness: He had suffered iron-deficiency anemia and hematochezia. His plasma hemoglobin values varied during this period, from 5 g/dL to 8 g/dL; the patient underwent blood transfusions and intravenous infusions of iron repeatedly.
History of past illness: He did not show past relevant comorbidities.
Physical examination upon admission: On examination, he was pale and did not show hemodynamic instability. He did not have abdominal pain.
Laboratory examinations: Laboratory blood tests showed an iron-deficiency anemia (hemoglobin: 9 g/dL).
Imaging examinations: Two UDEs and two colonoscopies, which were previously performed, were negative. It was decided to examine the small intestine with VCE, which showed a double lumen image in the ileum (Figure 4A). A severe circumferential ulcer with intense edema and recent bleeding evidence were identified in one of the lumens (Figure 4B). The findings were reported as suggestive of MD. CT-enterography revealed a diverticulum in the ileum. A Meckel’s Scan was not performed, and surgical intervention was decided by laparoscopy.
Final diagnosis was GIB due to MD in all patients.
Specific treatment in all cases was surgical resection of intestinal diverticulum with primary anastomosis. Surgical findings were: Case 1, an 8-cm long diverticulum at 30 cm from the ileocecal junction was found; case 2, an 8-cm in length diverticulum was observed in the ileum; in case 3, a 5 cm × 5 cm diverticulum located 45 cm from the ileocecal junction, which was resected and the video capsule was removed and in case 4, a 10-cm in length diverticulum within 53 cm of the ileocecal valve was found. The anatomopathological report revealed the presence of ulcerated ectopic gastric mucosa in the diverticulum in all the cases.
None had surgical or postoperative complications. The GIB disappeared after surgical treatment and they were discharged from the hospital in good conditions. Currently, none has showed recurrence of GIB.
A literature review of articles published in PubMed, Medline and Ovid databases from 2000 to date on patients with MD (confirmed by surgery) who underwent VCE was conducted. Publications describing the endoscopic characteristics of MD were selected. In addition, the demographic and clinical characteristics of patients as well as the prevalence of ectopic mucosa in the diverticulum were determined.
In total, 20 case reports[6-25] and 1 cohort study with 11 patients[26] were selected. The addition of our 4 patients gave a total of 35 patients for analysis. Of them, 30 were male (85.7%). The mean age was 28 ± 21.1 years (range: 2-80 years). Ten (28.5%) were pediatric patients (under 18 years). The majority of the patients were adults (71.5%), 68.5% were younger than 30 years old and 23% were over 50 years of age (Table 1).
| Parameter | n (%) |
| Male | 30 (87.5) |
| Female | 5 (12.5) |
| Age in yr, mean ± SD (range) | 24 ± 21.1 (2-80) |
| < 18 | 10 (28.5) |
| 19-39 | 14 (40) |
| 40-60 | 7 (20) |
| > 60 | 4 (11.5) |
| Symptoms | |
| Overt GIB | 26 (74.2) |
| Occult GIB | 8 (22.8) |
| Abdominal pain | 5 (14.2) |
| Duration of symptoms in mo, mean (range) | 35.1 (1–120) |
| Imaging studies prior to VCE | |
| Reported studies | 25 (71.4) |
| No reported studies | 10 (28.6) |
| CT/MRI enterography | 5 |
| CT scan | 2 |
| Push enteroscopy | 3 |
| Barium intestinal transit | 15 |
| Meckel's Scan | |
| Reported studies | 13 |
| Positive Meckel's Scan | 2 (15.3) |
| Ectopic Tissue | |
| Reported studies | 18 |
| Gastric/pancreatic | 16 (88.8) |
The clinical manifestations of the patients were overt GIB in 26 (74.2%), anemia in 8 (23%) and abdominal pain in 5 (14.2%). Symptoms had a mean duration of 35.1 mo (range: 1-120 mo) (Table 1).
In all cases, at least one UDE and one colonoscopy were performed. In 25 patients, one or more of the following diagnostic procedures were done: CT/magnetic resonance imaging-enterography in 5 patients; plain CT scan in 2 patients; push enteroscopy in 3 patients; and, barium intestinal transit in 15 patients. All procedures were reported as negative or showing irrelevant findings.
Meckel’s Scan was positive only in 2 out of 13 patients (15.3%). The 61.5% of cases having negative Meckel’s Scan were pediatric patients (Table 1).
Description of the endoscopic images of MD was available in 22 cases (18 published case reports and our 4 clinical cases) (Table 2). The images could be grouped into the following categories: (1) double lumen images in 15 (68.8%) patients; among them, those showing ulcers in one lumen accounted for 9 (41%) patients (Figures 1 and 3) and those not showing ulcers accounted for 6 (27.2%) patients (Figures 2B and 4A); (2) polypoid structure (true polyp in the diverticular mucosa or diverticular eversion) in 4 (18%) patients (Figures 2A, 5A and 5B); and (3) stenotic lumen and circumferential ulcer in 3 (12.6%) patients (Figure 4B).
| Feature | n (%) |
| Double lumen | 15 (68.8) |
| Double lumen with ulcers | 9 (41) |
| Double lumen without ulcers | 6 (27.2) |
| Polypoid structure (true polyp or diverticular eversion) | 4 (18) |
| Stenotic lumen with ulcer | 3 (13.6) |
The capsule was retained in the small intestine in 6 (17.1%) patients. It was lodged inside the diverticulum in 4 patients. Capsule removal through laparoscopy was performed in 2 cases at 4 mo after the procedure, where unsuspected MD was found[6,24]. One patient had delayed spontaneous elimination of the capsule[8]. Finally, the capsule was removed by double balloon enteroscopy in another patient[15], and by surgery in 2 cases[10].
In 16 (88.8%) out of 18 cases, ectopic mucosa was found in the diverticulum lining, represented by 14 gastric and 2 pancreatic findings.
Some publications have reported that MD can be found in 2.9% to 16% of cases with obscure (O)GIB[26-28]. In these patients, the complete revision of the small bowel is necessary in order to identify the source of bleeding. This was not possible until 2000 when the VCE was approved by the Food and Drug Administration for clinical use. Prior to this date, push enteroscopy was the only direct method for examining the interior of the small bowel. However, the intestine was only partially reviewed, so diagnostic yield was low[29].
VCE is a noninvasive procedure that consists of a mini photographic camera that takes multiple images per second after ingestion. In accordance with the published international guidelines[30,31], VCE should be used as the first procedure for small bowel examination in the diagnostic strategy of OGIB. In recent years, the use of VCE has been extensively increased worldwide, in such a way that a greater number of physicians face the challenge of identifying endoscopic patterns of small bowel diseases. It is strange that so far, very few studies on the endoscopic characteristics of MD by VCE have been published.
Age: Symptomatic MD is described as a predominant condition in children and adolescents and as infrequent in adults over 40-year-old[4]. The majority of patients included in our analysis were adults (71.5%). Many children with MD do not usually undergo a VCE because they are operated on, since they more frequently present complications of the disease[32]. Notwithstanding, this review seems to indicate that clinically-manifested MD is not an uncommon condition in adults.
Clinical manifestations: In this analysis, 34 of 35 patients had GIB and only 1 had abdominal pain. Hemorrhage was overt in 76.4% of cases. GIB has been described as one of the most frequent clinical manifestations of MD in children and adults. In a study with 119 adults with MD (mean age: 43 years), of whom 52 (43.6%) experienced clinical symptoms, GIB was observed only in 15% of the patients. Twenty-two percent of the whole group developed complications, which required urgent surgical intervention (inflammation, intestinal perforation, intestinal obstruction, severe abdominal pain, foreign body perforation)[33]. Another study involving 43 adults reported that patients with symptomatic MD had significant morbidity. Complications arising from surgical resection of incidental or symptomatic diverticulum were uncommon (8% to 9%), but were more frequently fatal[34].
Duration of symptoms: The diagnosis of MD in most of the patients in this review was made late (mean time of 3 years, ranging from 1 mo to 10 years). The majority of the patients underwent multiple transfusions, repeated hospitalizations and diverse endoscopic and radiological examinations. This may indicate that the current recommendations of the international guidelines for the diagnosis of OGIB (concerning early use of VCE) are not followed in many cases.
Diagnostic procedures: Conventional imaging procedures performed before VCE, did not suggest the diagnosis of MD in any case. Some published reports show the diagnostic accuracies of intestinal transit with barium, plain CT and mesenteric angiography to be 44%, 33% and 60%, respectively[33]. The CT-enterography scan, which combines the advantages of CT with those of conventional barium enteroclysis, could improve the diagnostic performance of MD[35]. However, its diagnostic performance in MD is unknown.
Meckel’s Scan: This test was positive in only 18.7% of the patients-a low figure compared to those reported in the literature. Some publications have reported sensitivity and specificity of 85% and 95% in children and of 62% and 9% in adults, respectively[36]. It is noteworthy that in this review, 61.5% of patients with negative Meckel’s Scan were pediatric patients, contrary to the aforementioned results. The causes of the poor sensitivity of Meckel’s Scan in both pediatric and adult patients in this review are difficult to explain. The presence of factors that produce a false negative result (i.e. active bleeding, poor vascular supply, previous use of barium for diagnosis of intestinal disorders, use of atropine, gastrointestinal study with barium, or small diverticulum) cannot be ruled out[37].
Endoscopic characteristics: Double lumen was the most frequent endoscopic pattern in patients with MD (69%). In some cases, ulcers in the circumference of one of the lumens were observed. Some authors have described a diaphragm image in the interluminal septum, which they called a “diaphragm sign” (Figure 4A). The double lumen image is strongly suggestive of MD and should lead to the indication of complementary imaging procedures or double balloon enteroscopy in order to establish preoperative diagnosis. In addition, other images of MD should be taken into account for diagnostic suspicion, such as a polypoid formation (which can be confounded with an intestinal tumor) and which was seen in 18% of cases in this review, or circumferential ulcers with luminal stenosis (which can evoke a nonsteroidal anti-inflammatory drug enteropathy or Crohn’s disease) and which was observed in 13% of the patients. The sensitivity and specificity of VCE in the diagnosis of MD is unknown; however, in a cohort study in which surgery was used as a gold standard test, the positive predictive value of VCE was 81.8%[26].
Capsule retention is the most feared complication of VCE, but occurs in only 2% of the patients. Crohn’s disease and intestinal tumor significantly increase this risk, up to 13%[30-38]. Capsule retention in this analysis was more frequent (17.1%). This places MD as a high-risk condition of capsule retention, so that use of the biodegradable Agile capsule may be considered[39,40].
Ectopic mucosa: The prevalence of ectopic mucosa in the diverticulum was higher (89%) in this analysis than that reported by other studies (43% to 48%)[4,33]. Ectopic mucosa is more frequent in symptomatic patients than in asymptomatic ones (48% vs 14%, respectively). The sensitivity of Meckel’s Scan in the patients with ectopic mucosa of this analysis was 16%, and this figure is far lower than that published in other series[36].
The limitations of this analysis are the following: (1) the number of patients was low, although this issue may reflect the low frequency with which endoscopic findings of this disease are reported in the literature, even in the era of VCE; and (2) the patients that comprised this analysis were selected by the fact that they underwent a VCE, and therefore may not represent the universe of patients with MD since the asymptomatic ones and those who required emergency surgery were not included.
In conclusion, our review indicated that symptomatic MD is not infrequent in adults. As such, we suggest that this condition should always be included in the differential diagnosis of OGIB or intestinal disease in this age group. We also found that conventional imaging studies have a low diagnostic sensitivity, and Meckel’s Scan may be negative, even in pediatric patients, suggesting that this test should not be taken as a reference for decision making. In addition, VCE appears to have high probability of diagnosing MD, so it should be done as early as possible. However, it is highly recommended that gastrointestinal endoscopists be trained for recognizing the different endoscopic patterns of MD. Images should be interpreted in the appropriate clinical context in order to perform complementary studies to confirm (or rule out) MD before surgery. Finally, we found the most frequently observed endoscopic pattern of MD to be the double lumen image and that MD may be considered as a high-risk condition of VCE retention, even with previous normal imaging studies.
In view of the difficulties for preoperative diagnosis of MD, the performance of multicenter studies with a large number of patients, in which the precise role of VCE in the diagnosis of MD is assessed, will be necessary.
Because of this review, we think that MD is an under-diagnosed disease in adults. Abdominal imaging procedures (CT/MR-enterography), have limited usefulness for diagnosis and Meckel’s Scan may not be a diagnostic reference test. VCE and balloon enteroscopy, which allow direct examination of small bowel, increase the probabilities of preoperative diagnosis. Notwithstanding, endoscopic patterns of MD have not been defined and there are very scarce publications concerning this issue. The most frequent endoscopic pattern of MD observed in our patients and in other reported cases was “double lumen”, followed by polyp formations and circumferential ulcers with luminal stenosis. In our experience with four patients reported here, diagnosis was initially missed in the first two cases because of lack of experience of endoscopist on recognition of endoscopic patterns of MD at that time. Endoscopic diagnosis was established retrospectively in them. Three patients had a long history of GI bleeding without etiologic diagnosis and VCE indication was delayed.
The improvement of preoperative diagnosis rates of MD will be possible through high suspicion of this condition and the training of gastrointestinal endoscopists on recognition of endoscopic features of MD obtained with VCE.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Mexico
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chan KWE, Dhaliwal HS S- Editor: Ma RY L- Editor: A E- Editor: Song H
| 1. | Lin XK, Huang XZ, Bao XZ, Zheng N, Xia QZ, Chen CD. Clinical characteristics of Meckel diverticulum in children: A retrospective review of a 15-year single-center experience. Medicine (Baltimore). 2017;96:e7760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Sagar J, Kumar V, Shah DK. Meckel’s diverticulum: a systematic review. J R Soc Med. 2006;99:501-505. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 171] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | Hong SN, Jang HJ, Ye BD, Jeon SR, Im JP, Cha JM, Kim SE, Park SJ, Kim ER, Chang DK. Diagnosis of Bleeding Meckel’s Diverticulum in Adults. PLoS One. 2016;11:e0162615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg. 2005;241:529-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 347] [Cited by in F6Publishing: 322] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Thurley PD, Halliday KE, Somers JM, Al-Daraji WI, Ilyas M, Broderick NJ. Radiological features of Meckel’s diverticulum and its complications. Clin Radiol. 2009;64:109-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Yu H, Song H, Cai J. Laparoscopic treatment of hemorrhagic Meckel diverticulum after diagnosis with wireless capsule endoscopy and double-balloon enteroscopy. Rev Esp Enferm Dig. 2017;109:315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Day NJ, Fultz P, Marino D. Recurrent Small-Bowel Obstruction Caused by a Meckel’s Diverticulum Diagnosed on Video Capsule Endoscopy. Clin Gastroenterol Hepatol. 2016;14:A21-A22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Xinias I, Mavroudi A, Fotoulaki M, Tsikopoulos G, Kalampakas A, Imvrios G. Wireless Capsule Endoscopy Detects Meckel’s Diverticulum in a Child with Unexplained Intestinal Blood Loss. Case Rep Gastroenterol. 2012;6:650-659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Desai SS, Alkhouri R, Baker SS. Identification of meckel diverticulum by capsule endoscopy. J Pediatr Gastroenterol Nutr. 2012;54:161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Courcoutsakis N, Pitiakoudis M, Mimidis K, Vradelis S, Astrinakis E, Prassopoulos P. Capsule retention in a giant Meckel’s diverticulum containing multiple enteroliths. Endoscopy. 2011;43 Suppl 2 UCTN:E308-E309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Ibuka T, Araki H, Sugiyama T, Takada J, Kubota M, Shirakami Y, Shiraki M, Shimizu M, Suzui N, Miyazaki T. A case of an elderly patient with inverted Meckel’s diverticulum with small intestinal bleeding detected using capsule and double-balloon endoscopies. Nihon Shokakibyo Gakkai Zasshi. 2017;114:2005-2011. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 12. | Montemaggi A, Paci M, Barp J, Milla M, Lionetti P. Circumferential peptic ulceration from Meckel diverticulum by capsule endoscopy. J Pediatr Gastroenterol Nutr. 2012;54:1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Pastore S, Gortani G, Maschio M, Di Leo G, Ventura A. Two lumens, one diagnosis. J Pediatr. 2011;159:511. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Mavrogenis G, Coumaros D, Bellocq JP, Leroy J. Detection of a polypoid lesion inside a Meckel’s diverticulum using wireless capsule endoscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E115-E116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Tanaka Y, Motomura Y, Akahoshi K, Nakama N, Osoegawa T, Kashiwabara Y, Chaen T, Higuchi N, Kubokawa M, Nishida K. Capsule endoscopic detection of bleeding Meckel’s diverticulum, with capsule retention in the diverticulum. Endoscopy. 2010;42 Suppl 2:E199-E200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Sokol H, Seksik P, Wendum D, Bellanger J, Parc Y, Cosnes J, Beaugerie L. Gastrointestinal bleeding diagnosed using video capsule endoscopy. Meckel’s diverticulum. Gut. 2009;58:1206, 1290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Sy ED, Chen MD, Yang YJ, Shan YS. Obscure gastrointestinal bleeding due to Meckel’s diverticulum: unusual capsule endoscopic finding as polyp-like lesion. Endoscopy. 2008;40 Suppl 2:E203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Kovács M, Davidovics S, Gyurus P, Rácz I. Identification of a Meckel’s diverticulum bleeding by urgent capsule endoscopy. Orv Hetil. 2006;147:2003-2006. [PubMed] [Cited in This Article: ] |
| 19. | Pozzato P, Brancaccio M, Sacco S, Virzì S, Ventrucci M. Capsule endoscopy for the detection of bleeding Meckel’s diverticulum. A case report. Minerva Gastroenterol Dietol. 2006;52:327-331. [PubMed] [Cited in This Article: ] |
| 20. | Yu WK, Yang RD. M2A video capsule lodged in the Meckel’s diverticulum. Gastrointest Endosc. 2006;63:1071-1072; discussion 1072. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Moon JH, Park CH, Kim JH, Jung JW, Kim JP, Kim KO, Yoo KS, Hahn T, Park SH, Park CK. Meckel’s diverticulum bleeding detected by capsule endoscopy. Gastrointest Endosc. 2006;63:702, discussion 703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Gölder S, Schmidt J, Kolmsee P, Rösner K, Strik M, Mohren W, Weigert N. Identification of a Meckel’s diverticulum by wireless capsule endoscopy. Endoscopy. 2005;37:608. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Park SM, Chun HJ, Jeen YT, Yoon I, Kim JY, Kim CY, Kim JH, Lee JY, Choung RS, Kim YS. A case of chronic gastrointestinal bleeding from a Meckel’s diverticulum detected by wireless capsule endoscopy. Korean J Gastroenterol. 2004;43:125-128. [PubMed] [Cited in This Article: ] |
| 24. | Gortzak Y, Lantsberg L, Odes HS. Video Capsule entrapped in a Meckel’s diverticulum. J Clin Gastroenterol. 2003;37:270-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Mylonaki M, MacLean D, Fritscher-Ravens A, Swain P. Wireless capsule endoscopic detection of Meckel’s diverticulum after nondiagnostic surgery. Endoscopy. 2002;34:1018-1020. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Krstic SN, Martinov JB, Sokic-Milutinovic AD, Milosavljevic TN, Krstic MN. Capsule endoscopy is useful diagnostic tool for diagnosing Meckel’s diverticulum. Eur J Gastroenterol Hepatol. 2016;28:702-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Hartmann D, Schmidt H, Bolz G, Schilling D, Kinzel F, Eickhoff A, Huschner W, Möller K, Jakobs R, Reitzig P. A prospective two-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61:826-832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 230] [Cited by in F6Publishing: 245] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 28. | Fritscher-Ravens A, Scherbakov P, Bufler P, Torroni F, Ruuska T, Nuutinen H, Thomson M, Tabbers M, Milla P. The feasibility of wireless capsule endoscopy in detecting small intestinal pathology in children under the age of 8 years: a multicentre European study. Gut. 2009;58:1467-1472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | ASGE Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Yang J, DeWitt JM. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017;85:22-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 30. | Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, Leontiadis GI, Tse F, Sadowski D. Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology. 2017;152:497-514. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 245] [Cited by in F6Publishing: 242] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 31. | Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 482] [Cited by in F6Publishing: 511] [Article Influence: 56.8] [Reference Citation Analysis (0)] |
| 32. | Huang CC, Lai MW, Hwang FM, Yeh YC, Chen SY, Kong MS, Lai JY, Chen JC, Ming YC. Diverse presentations in pediatric Meckel’s diverticulum: a review of 100 cases. Pediatr Neonatol. 2014;55:369-375. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 33. | Groebli Y, Bertin D, Morel P. Meckel’s diverticulum in adults: retrospective analysis of 119 cases and historical review. Eur J Surg. 2001;167:518-524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Stone PA, Hofeldt MJ, Campbell JE, Vedula G, DeLuca JA, Flaherty SK. Meckel diverticulum: ten-year experience in adults. South Med J. 2004;97:1038-1041. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Kotha VK, Khandelwal A, Saboo SS, Shanbhogue AK, Virmani V, Marginean EC, Menias CO. Radiologist’s perspective for the Meckel’s diverticulum and its complications. Br J Radiol. 2014;87:20130743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 36. | Dillman JR, Wong KK, Brown RK, Frey KA, Strouse PJ. Utility of SPECT/CT with Meckel’s scintigraphy. Ann Nucl Med. 2009;23:813-815. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Tauro LF, Martis JJ, Menezes LT, Shenoy HD. Clinical profile and surgical outcome of Meckel’s diverticulum. J Indian Med Assoc. 2011;109:489-490. [PubMed] [Cited in This Article: ] |
| 38. | Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 472] [Cited by in F6Publishing: 425] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 39. | Goenka MK, Majumder S, Goenka U. Capsule endoscopy: Present status and future expectation. World J Gastroenterol. 2014;20:10024-10037. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 60] [Cited by in F6Publishing: 48] [Article Influence: 4.8] [Reference Citation Analysis (2)] |
| 40. | Rezapour M, Amadi C, Gerson LB. Retention associated with video capsule endoscopy: systematic review and meta-analysis. Gastrointest Endosc. 2017;85:1157-1168.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |