Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.759
Peer-review started: August 8, 2018
First decision: August 24, 2018
Revised: September 13, 2018
Accepted: October 11, 2018
Article in press: October 12, 2018
Published online: November 26, 2018
To retrospectively evaluate the safety and feasibility of a new modified laparoscopic Sugarbaker repair in patients with parastomal hernias.
A retrospective study was performed to analyze eight patients who underwent parastomal hernia repair between June 2016 and January 2018. All of these patients received modified laparoscopic Sugarbaker hernia repair treatment. This modified technique included an innovative three-point anchoring and complete suturing technique to fix the mesh. All procedures were performed by a skilled hernia surgeon. Demographic data and perioperative outcomes were collected to evaluate the safety and efficacy of this modified technique.
Of these eight patients, two had concomitant incisional hernias. All the hernias were repaired by the modified laparoscopic Sugarbaker technique with no conversion to laparotomy. Three patients had in-situ reconstruction of intestinal stoma. The median mesh size was 300 cm2, and the mean operative time was 205.6 min. The mean postoperative hospitalization time was 10.4 d, with a median pain score of 1 (visual analog scale method) at postoperative day 1. Two patients developed postoperative complications. One patient had a pocket of effusion surrounding the biologic mesh, and one patient experienced an infection around the reconstructed stoma. Both patients recovered after conservative management. There was no recurrence during the follow-up period (6-22 mo, average 13 mo).
The modified laparoscopic Sugarbaker repair could fix the mesh reliably with mild postoperative pain and a low recurrence rate. The technique is safe and feasible for parastomal hernias.
Core tip: Parastomal hernia is a common complication after enterostomy. We introduce a new modified laparoscopic Sugarbaker repair technique with three-point anchoring to repair the parastomal hernia. The findings confirm the safety and feasibility of the modified method and support the application of this technique to parastomal hernias.
- Citation: Huang DY, Pan L, Chen QL, Cai XY, Fang J. Modified laparoscopic Sugarbaker repair of parastomal hernia with a three-point anchoring technique. World J Clin Cases 2018; 6(14): 759-766
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/759.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.759
Parastomal hernia (PSH) is an incisional hernia at the site of the surgical wound. It is a common complication following enterostomy with an incidence rate as high as 48%[1]. Surgery is the only treatment to repair PSH. Similar to the repair of an abdominal wall hernia, the recurrence rate of postoperative PSH has decreased significantly with the development of mesh technology[2]. However, given the existence of intestinal stoma PSH, repair is always a challenge for the surgeons.
Similar to other incisional hernias, PSH could be safely and effectively repaired by the laparoscopic approach. The laparoscopic Sugarbaker technique is the most effective method to reduce the recurrence rate[3] and is recommended by the International Endohernia Society[4]. However, consensus does not exist regarding the mesh selection procedure, the method of mesh fixation, and other operative technical details for this technique. These issues require further investigation.
One of the technical details most difficult to determine during the laparoscopic Sugarbaker technique is a strategy for reliably fixing the mesh to construct a funnel that can hold the ostomic intestine inside not only to avoid injury and compression to the intestine but also to reduce the hernia recurrence rate. We focused on this aspect to improve the technical details of the laparoscopic Sugarbaker technique[5-7]. In our hospital, we applied an innovative three-point anchoring and suturing technique to fix the mesh during the laparoscopic Sugarbaker technique. We retrospectively review our techniques and the outcomes of our patients.
Our research was a single-center retrospective study performed between June 2016 and January 2018. Eight patients with the diagnosis of primary PSH who underwent a modified laparoscopic Sugarbaker technique were included. Inclusion criteria were clinical symptoms consistent with PSH with no acute bowel obstruction or strangulation. All the operations were performed by the same surgeon. The study protocol was approved by the hospital ethics committee.
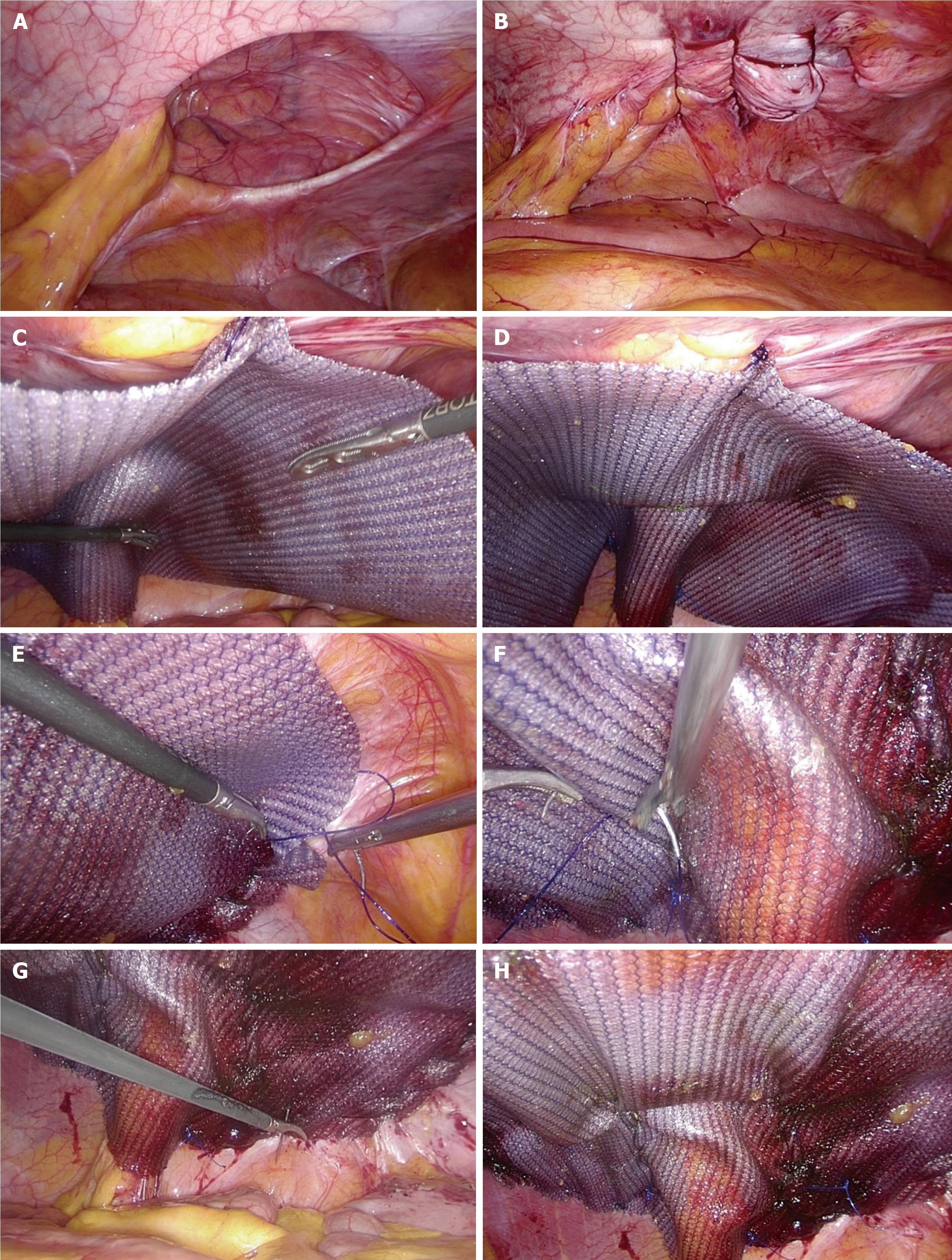
All patients underwent preoperative abdominal computed tomography (CT) imaging to evaluate the size of the PSH defect, the contents of the hernia, and the length of the ostomic intestine. Routine bowel preparation was performed before the operation. After successful general anesthesia, patients were placed in the supine position. Gauze and polyurethane film dressing tape were used to cover the intestinal stoma after routine disinfection. Based on the location of the stoma, the first incision was made on the opposite side of the abdomen as far as possible away from the stoma and the previous incision site. For example, in patients with stoma on the left lower quadrant of the abdomen, the first incision was made to the right upper quadrant of the abdomen. The puncture incision was performed using the Verssel technique to establish and maintain a 15-mmHg carbon dioxide pneumoperitoneum. The abdominal cavity was explored after the placement of the laparoscopic lens. Under direct visualization, two or three incisions were made on both sides of the first incision followed by the placement of 5-mm or 12-mm Trocars. Adhesiolysis was performed to separate the intestine and omentum from the abdominal wall by cold and sharp instruments, such as scissors. An ultrasound knife and coagulation were only used for hemostasis. Adhesiolysis was performed in the hernia sac to reduce the hernia contents as much as possible. After adhesiolysis, the size of the defect was assessed to confirm whether the defect could be closed under laparoscopy (a defect larger than 5 cm was typically difficult to close using the laparoscopic approach) (Figure 1A). Then, the dressing covering the stoma was removed, and the area around the stoma was disinfected again. The defect was closed by interrupted suturing with PDSTM (Ethicon®) with assistance from a suture grasping device (Figure 1B). Under the following conditions, we performed the reconstruction of stoma using the Lap-Re-Do technique, which was previously published in detail by Yang et al[8]: The hernia contents could not be reduced completely laparoscopically, there was a large defect that was unlikely to be closed laparoscopically, and there was a long and twisted stoma in the hernia sac. The loop of ostomic intestine was also evaluated to ensure that the Sugarbaker technique could be applied. If the loop was not long enough for the Sugarbaker technique, the keyhole technique was used.
Then, the first anchoring point for the mesh was determined under laparoscopic visualization. A 5-cm-long suture thread was placed into the abdominal cavity. One end of the suture thread was placed at the innermost point of the stoma, and the thread was straightened to be perpendicular to the midline of the abdomen. The abdominal wall, which was reached by the other end of the suture thread, was marked. Based on the actual operating conditions, we selected one of two types of mesh. If the operative field might be contaminated, a biologic mesh (BiodesignTM, Surgsis®) was selected. Otherwise, a synthetic mesh (SeprameshTM, Bard®) was used if no signs of contamination were present. The mesh was trimmed to the appropriate size to cover the defect by at least 5 cm in all directions. One stitch with PDS thread was placed and tied at the middle point of the long edge on the inner side of the mesh. Pneumoperitoneum was re-established. The mesh was rolled up, placed inside the abdominal cavity, and then expanded. A small incision was made at the site on the abdominal wall marked previously. The PDS thread tied to the mesh was pulled out with a suture-grasping device and knotted. Two pairs of clamps were used to adjust the mesh to attach to the peritoneal wall to place the stoma in the middle position on the outside surface of the mesh (Figure 1C). Stitches with a 2-0 ProleneTM (Ethicon®) thread were placed in the upper and lower part of the mesh to anchor the mesh to the peritoneal wall at the site close to the stoma. The mesh was folded to form a funnel to accommodate the ostomic intestine passing inside. Positioning of the mesh was completed after the abovementioned three-point anchoring and suturing (Figure 1D). Then, four edges of the mesh were fixed to the peritoneal wall with continuous suturing using 2-0 StratifixTM (Ethicon®) thread (Figure 1E). Care was taken not to injure the underlying peritoneal vessels during the suturing. The same stitches were placed in the upper and lower edges of the ostomic intestine to suture the mesh to the peritoneal wall. Stitches were placed from the lateral side of the mesh to the inside of the stoma to construct a funnel to allow the passage of the ostomic intestine (Figure 1F). Finally, we performed the transfascial suture with a purse-string needle (ST-70, ProleneTM, Ethicon®) to puncture the abdominal wall corresponding to the four corners of the mesh (Figure 1G). Two tips of the purse-string needle entered the skin at the same site and passed through the mesh at two different points 1 cm apart. The thread was cut and knotted inside the abdominal cavity. The mesh was then fixed to the peritoneal fascia (Figure 1H). We did not use any tack or glue to fix the mesh. Before the end of the operation, the stoma was examined manually to ensure there was no stenosis.
Postoperative pain intensity was assessed by a visual analog scale. Intravenous analgesic medication was administered for pain relief up to the postoperative day 3. Patients who did not undergo the Lap-Re-Do procedure were given a semi-liquid diet from postoperative day 1. They did not receive any intravenous antibiotics or total parenteral nutrition, and they were discharged when stool passed normally from the stoma. For patients undergoing the Lap-Re-Do procedure, intravenous antibiotics were administered for 3 d postoperatively to prevent any infection near the incisional site. The patients fasted, and total parenteral nutrition was given until postoperative day 5. A liquid diet was started on day 5 and changed to a semi-liquid diet on day 7. Patients were discharged when no infection was observed, and the stool passed through the stoma.
Patients’ preoperative conditions are listed in Table 1. None of the patients received emergent surgery. Two patients had diabetes, and preoperative blood glucose levels were well controlled. One patient had a long smoking history and quit smoking 3 years ago. All the ileostomies were located in the right lower quadrant of the abdomen. All the colostomies were located in the left lower quadrant of the abdomen. Two patients had a concomitant incisional hernia, which was located in the midline of the lower abdominal wall.
| No. of patients | 8 |
| Age (yr) | 65.3 ± 7.4 |
| Gender (male/female) | 5/3 |
| BMI (kg/m2) | 24.5 ± 3.8 |
| ASA | |
| I | 0 |
| II | 7 |
| III | 1 |
| Comorbidity | Two cases of diabetes |
| Smoker (yes/no) | 1/7 |
| Type of stoma | |
| Colostomy | 4 |
| Ileostomy | 4 |
| Size of defect (cm2) | 17.9 ± 10.3 |
| EHS classification of PSHs | |
| EHS 1 | 3 |
| EHS 2 | 1 |
| EHS 3 | 3 |
| EHS 4 | 1 |
Patients’ intraoperative conditions and postoperative follow-up outcomes are presented in Table 2. All laparoscopic procedures were successful, and none of the patients required laparotomy. Three patients received the Lap-Re-Do procedure to remove the extra ostomic intestinal segment and the hernia sac to facilitate the reconstruction of the stoma in situ. Two patients with concomitant incisional hernias received simultaneous incisional hernia repairs with the same mesh to cover the incision and parastomal defects. In these procedures, no additional mesh was used, and no additional incisions were made. Two patients had potential postoperative contaminations around the surgical field. One patient underwent the Lap-Re-Do procedure. Another patient had an ileal PSH after the radical cystectomy for bladder cancer. The ostomic intestine was injured when separating the adhesion between the bowels. This injury was immediately repaired under the laparoscope. We used a biologic mesh in these two patients. The remaining six patients received a synthetic mesh.
| Outcomes | Results |
| Time spent for operation (min), mean ± standard deviation | 205.6 ± 66.7 |
| No. of patients undergoing Lap-Re-Do (yes/no) | 3/5 |
| Concomitant incisional hernia (yes/no) | 2/6 |
| Types of mesh (biologic/Sepramesh) | 2/6 |
| Intraoperative complication (yes/no) | 1/7 |
| Size of mesh (cm2), median (range) | 300 (221.3-300) |
| Pain score on postoperative day 1 (VAS) | |
| Median (range) | 1 (1-2) |
| VAS = 1 | 6 patients |
| VAS = 2 | 2 patients |
| Number of days of postoperative stay, mean ± standard deviation | 10.4 ± 6.3 |
| Follow-up period (mo), mean (min, max) | 12.9 (6, 22) |
| Number of hernia recurrences | 0 |
| Postoperative complication (yes/no) | 2/6 |
On the first postoperative day, the pain score was 1–2 points with a mean of 1.4 ± 0.5. No patient reported a pain score greater than 3 points or required additional analgesic treatments. All patients were able to ambulate on postoperative day 1. Two patients developed complications during the postoperative hospital stay. One patient with ileal PSH had an intraoperative ileal injury that was repaired by the biologic mesh. He suffered from a cloudy fluid leakage from the left side of the Trocar incision site on postoperative day 7. Ultrasound examination revealed a pocket of fluid around the mesh. CT-guided puncture and aspiration were performed, and a drainage catheter was placed. The aspirated fluid was turbid effusion with no intestinal fluid. The patient had no fever, abdominal pain or distension and could eat and defecate normally. Fluid drainage gradually decreased and finally disappeared. The catheter was removed, and the patient was discharged. Another patient undergoing the Lap-Re-Do procedure developed a postoperative parastomal abscess, which was superficial with no connection to the peritoneal cavity after opening the incision. The abscess gradually resolved after dressing changes and intravenous antibiotic treatments. The incision healed with no requirement for a secondary repair.
The mean follow-up time was 13 mo, ranging from 6 to 22 mo. No evidence for hernia recurrence was found during the clinic visits. Only one patient underwent repeated CT scans, which confirmed that there was no recurrence of the hernia.
PSH is a common complication after surgeries for colon or small intestine stoma reconstruction. Some patients with no clinical symptoms can be treated conservatively[9]. However, between 30%–70% patients eventually require surgical treatment for various reasons. Similar to a ventral hernia, PSH can be repaired by simple suturing, which is an easy operation. However, simple suturing commonly results in a high recurrence rate and is not appropriate for most patients[10]. Mesh repair is the most effective surgical method in this situation. Peritoneal mesh placement through the laparoscopic approach has many advantages for abdominal wall hernia repair. It can shorten the operation time and has a low recurrence rate[3]. The laparoscopic approach has become one of the most commonly used methods to repair PSH. Based on the position of the mesh and its distance to the ostomic intestine, laparoscopic PSH repair employs three main surgical techniques: the keyhole, Sugarbaker, and sandwich methods. According to previous publications, the Sugarbaker method has a lower recurrence rate compared with the keyhole method and is significantly less expensive compared with the sandwich method[3,11,12].
The Sugarbaker method was first proposed in 1980. The Sugarbaker method was performed during the laparotomy, and a nonslit prosthesis was placed to the lateral side of the bowel. The prosthesis was fixed to the peritoneal fascia by suturing at 1-cm intervals. Advantages of this method are that the stoma is not affected and the intestinal function recovers quickly after the operation. In addition, the colon passes through the funnel formed by the prosthesis, and recurrent herniation around the stoma is prevented[13]. In 2000, Voitk performed the Sugarbaker technique through the laparoscopic approach for the first time[14]. He used the tack to anchor the mesh without transfascial suturing. Since then, many researchers have made various improvements in the placements and fixations of the mesh[5-7,15].
The main technical difficulty during the Sugarbaker procedure involves how to fix the mesh to the abdominal wall to establish an appropriate funnel to allow the passage of ostomic intestine and its content without causing any stenosis or obstruction. The mesh should also prevent other intestines from entering the funnel, which could lead to incarceration and hernia recurrence. At the same time, the mesh should be fully flattened along the peritoneal wall. In the cases reported previously, the mesh was fixed to the peritoneal wall via transfascial suturing, a tack, or a combination of the two, which is similar to the method used during ventral hernia repair. We believe that transfascial suturing is necessary for the Sugarbaker technique given that transfascial suturing is critical to prevent hernia recurrence. However, unlike the ventral hernia, the final shape of the mesh around the PSH is not flat but rather a complex curved surface. From the outside of the peritoneal cavity, it is difficult to predict the final position for the mesh inside the peritoneal cavity for transfascial suturing. Mesh fixation via the simple technique similar to ventral hernia repair often causes the mesh to be distorted and not flattenable[5]. In addition, inappropriately positioned and tensional transfascial sutures could cause significant postoperative pain[16,17]. Therefore, we believe that the placement of the mesh during the Sugarbaker technique should be improved. Ideally, the mesh should be placed in the peritoneal cavity at the most appropriate location with initial anchoring, and then the final fixation is performed by transfascial suturing.
Currently, there is no uniform standard for meshes used in the Sugarbaker procedure. Meshes reported in the literature include polypropylene, expanded polytetrafluoroethylene (ePTFE), polyvinylidene fluoride (PVDF), polyester and biological meshes[18]. SeprameshTM and BiodesignTM were used in our study. SeprameshTM, a synthetic mesh with coating, is safe and effective in parastomal hernia repair[19]. The advantage of biological meshes is that they can be used safely in herniorrhaphy with minimal risk of contamination; however, the recurrence rate is high[20,21]. Therefore, we only apply this mesh to cases where the surgical area is suspected to be contaminated. In our study, no mesh-related complications were found.
Our procedure to shape and fix the mesh inside the peritoneal cavity includes four steps. The first step is to determine the initial three anchoring points. One is the midpoint of the inside surface of the mesh, which is anchored through the transfascial suturing. The other two anchoring points, which are located on the outside surface of the mesh, are used to form the funnel and are sutured to the peritoneal wall with Prolene thread. After this first step, the position of the mesh and the shape of the funnel are determined in the peritoneal cavity. The second step is to flatten the mesh and place continuous stitches at the edges of the mesh to suture it to the peritoneal wall. The third step is to construct the funnel by continuous stitches through suturing from the outer edges of the mesh until the site of the stoma is reached. Given that this step is performed without tension and along the natural course of the intestine, it avoids bowel twisting and obstruction after the Sugarbaker procedure as reported by some authors[22,23]. After these three steps, the mesh is completely flattened and fixed on the peritoneal wall without distortion. The final step to fix the mesh in our procedure is transfascial suturing. Our method is different from the traditional method. A double-ended needle is inserted through the skin and passed into the peritoneal cavity to reach the mesh at two different locations 1 cm apart. Then, the needle is removed, and a loose knot is placed. Given that the mesh is already fixed inside the peritoneal cavity, this step is easy and does not cause any tension. Therefore, our procedure is tension free. Our patients suffered minimal postoperative pain, even with activity.
Although a tack is the most common choice by other physicians, we do not use a tack to fix mesh. A tack is easy to use but can cause some potential risks, including acute and chronic postoperative pain[24,25], volvulus, and bowel injury[26,27]. The length of the commonly used metal tack is 4 mm. When considering the thickness of the mesh, the actual depth of the tack nailed into the tissue is less than 3 mm, potentially cause its unreliability to fix the mesh to the peritoneal wall. In addition, the tack is placed close to the PSH, which could cause tension to both sides of the funnel formed by the mesh. When intestinal peristalsis or passage of the intestinal contents occurs, mesh failure and hernia recurrence could result[28]. Thus, the effect of fixation of the mesh to the peritoneal wall through the tack remains unclear. In addition, the tack device is relatively expensive. It was reported that continuous suturing to fix the mesh to the peritoneal wall during ventral hernia repair could avoid complications from the tack placement[29]. Our fixation technique is reliable, and the procedure is inexpensive. Patients also had minimal pain postoperatively. Our patients had minimal pain postoperatively, and none of them suffered hernia recurrence. One of the reasons for this finding might be attributed to the use of continuous suturing instead of a tack. Although continuous suturing requires higher technical skills and longer operation times than tack placement, it should be acceptable when considering its better outcomes.
In patients with long and twisted ostomic intestine in the hernia sac, we followed the Lap-Re-Do procedure reported by Yang et al[8], which involves the resection of the original stoma, opening of the fascia, and reconstruction of the stoma in situ. We believe that this procedure could improve stoma function and restore the normal contour of the abdominal wall. Three of our patients underwent the Lap-Re-Do procedure. One of them had a postoperative infection around the stoma, which did not spread to the deep tissues and the mesh. The infection was resolved after drainage and intravenous antibiotic administration.
In summary, our modified laparoscopic Sugarbaker technique could repair the PSH. In addition to being tension free, it is easy to operate inside the peritoneal cavity. It also has the advantages of fewer postoperative complications and minimal postoperative pain. We did not observe any hernia recurrence during the follow-up period; however, long-term studies should be conducted to confirm our results.
Parastomal hernia (PSH) is a common complication following enterostomy. The laparoscopic Sugarbaker technique has been shown to be the most effective method and is recommended by the International Endohernia Society. However, no consensus exists regarding the mesh selection procedure, the method of mesh fixation, and other operative technical details for this technique.
One of the technical details most difficult to determine during the laparoscopic Sugarbaker technique is a strategy for reliably fixing the mesh to construct a safe funnel. We applied a modified Sugarbaker technique to PSH in our center to try to reduce the technical difficulty.
To assess the safety and feasibility of the modified laparoscopic Sugarbaker repair in patients with PSH.
A total of 8 patients received modified laparoscopic Sugarbaker hernia repair treatment. This modified technique included an innovative three-point anchoring and complete suturing technique to fix the mesh. Perioperative outcomes, including operative and postoperative complications, were collected to retrospectively evaluate the safety and efficacy of this modified technique.
All the hernias were repaired using the modified laparoscopic Sugarbaker technique with no conversion to laparotomy. The mean operative time was 205.6 min, and the mean postoperative hospitalization time was 10.4 d, with a median pain score of 1 (visual analog scale method) at postoperative day 1. Two patients experienced mild postoperative complications and recovered after conservative management. No recurrence occurred during the follow-up period.
The modified laparoscopic Sugarbaker repair with three-point anchoring technique could fix the mesh reliably with mild postoperative pain and a low recurrence rate. The technique is safe and feasible for PSH.
Our study demonstrates that the modified laparoscopic Sugarbaker repair is safe and efficient via three-point anchoring for PSH. Surgeons can use our method to repair PSH.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Park BK, Richardson WS S- Editor: Ma RY L- Editor: A E- Editor: Song H
| 1. | Carne PW, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg. 2003;90:784-793. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 453] [Cited by in F6Publishing: 381] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 2. | Hansson BM, Slater NJ, van der Velden AS, Groenewoud HM, Buyne OR, de Hingh IH, Bleichrodt RP. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Ann Surg. 2012;255:685-695. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 3. | DeAsis FJ, Lapin B, Gitelis ME, Ujiki MB. Current state of laparoscopic parastomal hernia repair: A meta-analysis. World J Gastroenterol. 2015;21:8670-8677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 70] [Cited by in F6Publishing: 61] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 4. | Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli G, Fortelny R, Köckerling F, Kukleta J, LeBlanc K, Lomanto D. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])-Part III. Surg Endosc. 2014;28:380-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Suwa K, Nakajima S, Uno Y, Suzuki T, Sasaki S, Ushigome T, Eto K, Okamoto T, Yanaga K. Laparoscopic modified Sugarbaker parastomal hernia repair with 2-point anchoring and zigzag tacking of Parietex™ Parastomal Mesh technique. Surg Endosc. 2016;30:5628-5634. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Stelzner S, Hellmich G, Ludwig K. Repair of paracolostomy hernias with a prosthetic mesh in the intraperitoneal onlay position: modified Sugarbaker technique. Dis Colon Rectum. 2004;47:185-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Pauli EM, Juza RM, Winder JS. How I do it: novel parastomal herniorrhaphy utilizing transversus abdominis release. Hernia. 2016;20:547-552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Yang X, He K, Hua R, Shen Q, Yao Q. Laparoscopic repair of parastomal hernia. Ann Transl Med. 2017;5:45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Cévese PG, D’Amico DF, Biasiato R, Frego MG, Tropea A, Giaconi MA, Bianchera GG. Peristomal hernia following end-colostomy: a conservative approach. Ital J Surg Sci. 1984;14:207-209. [PubMed] [Cited in This Article: ] |
| 10. | Riansuwan W, Hull TL, Millan MM, Hammel JP. Surgery of recurrent parastomal hernia: direct repair or relocation? Colorectal Dis. 2010;12:681-686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Hansson BM, Bleichrodt RP, de Hingh IH. Laparoscopic parastomal hernia repair using a keyhole technique results in a high recurrence rate. Surg Endosc. 2009;23:1456-1459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Hansson BM, Morales-Conde S, Mussack T, Valdes J, Muysoms FE, Bleichrodt RP. The laparoscopic modified Sugarbaker technique is safe and has a low recurrence rate: a multicenter cohort study. Surg Endosc. 2013;27:494-500. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 13. | Sugarbaker PH. Prosthetic mesh repair of large hernias at the site of colonic stomas. Surg Gynecol Obstet. 1980;150:576-578. [PubMed] [Cited in This Article: ] |
| 14. | Voitk A. Simple technique for laparoscopic paracolostomy hernia repair. Dis Colon Rectum. 2000;43:1451-1453. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Fischer I, Wundsam H, Mitteregger M, Köhler G. Parastomal Hernia Repair with a 3D Funnel Intraperitoneal Mesh Device and Same-Sided Stoma Relocation: Results of 56 Cases. World J Surg. 2017;41:3212-3217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Kobayashi M, Ichikawa K, Okamoto K, Namikawa T, Okabayashi T, Araki K. Laparoscopic incisional hernia repair. A new mesh fixation method without stapling. Surg Endosc. 2006;20:1621-1625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, Köckerling F, Kukleta J, LeBlanc K, Lomanto D. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])—Part 2. Surg Endosc. 2014;28:353-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 18. | Antoniou SA, Agresta F, Garcia Alamino JM, Berger D, Berrevoet F, Brandsma HT, Bury K, Conze J, Cuccurullo D, Dietz UA. European Hernia Society guidelines on prevention and treatment of parastomal hernias. Hernia. 2018;22:183-198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 190] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 19. | Rose J, Jayaraman S, Colquhoun P, Taylor B. Minimal abdominal adhesions after Sepramesh repair of a parastomal hernia. Can J Surg. 2009;52:E211-E212. [PubMed] [Cited in This Article: ] |
| 20. | Slater NJ, Hansson BM, Buyne OR, Hendriks T, Bleichrodt RP. Repair of parastomal hernias with biologic grafts: a systematic review. J Gastrointest Surg. 2011;15:1252-1258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Warwick AM, Velineni R, Smart NJ, Daniels IR. Onlay parastomal hernia repair with cross-linked porcine dermal collagen biologic mesh: long-term results. Hernia. 2016;20:321-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | DeAsis FJ, Linn JG, Lapin B, Denham W, Carbray JM, Ujiki MB. Modified laparoscopic Sugarbaker repair decreases recurrence rates of parastomal hernia. Surgery. 2015;158:954-959; discussion 959-961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Hansson BM, van Nieuwenhoven EJ, Bleichrodt RP. Promising new technique in the repair of parastomal hernia. Surg Endosc. 2003;17:1789-1791. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Bansal VK, Misra MC, Babu D, Singhal P, Rao K, Sagar R, Kumar S, Rajeshwari S, Rewari V. Comparison of long-term outcome and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a prospective, randomized, controlled study. Surg Endosc. 2012;26:3476-3485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J. Randomized clinical trial of fibrin sealant versus titanium tacks for mesh fixation in laparoscopic umbilical hernia repair. Br J Surg. 2011;98:1537-1545. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Fitzgerald HL, Orenstein SB, Novitsky YW. Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutan Tech. 2010;20:e132-e135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Haltmeier T, Groebli Y. Small bowel lesion due to spiral tacks after laparoscopic intraperitoneal onlay mesh repair for incisional hernia. Int J Surg Case Rep. 2013;4:283-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Mancini GJ, McClusky DA 3rd, Khaitan L, Goldenberg EA, Heniford BT, Novitsky YW, Park AE, Kavic S, LeBlanc KA, Elieson MJ, Voeller GR, Ramshaw BJ. Laparoscopic parastomal hernia repair using a nonslit mesh technique. Surg Endosc. 2007;21:1487-1491. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Jagad RB. Laparoscopic ventral hernia repair: a new method for fixation of the mesh with sutures. Surg Laparosc Endosc Percutan Tech. 2008;18:277-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |