Published online Nov 6, 2018. doi: 10.12998/wjcc.v6.i13.683
Peer-review started: May 14, 2018
First decision: June 8, 2018
Revised: July 26, 2018
Accepted: October 8, 2018
Article in press: October 9, 2018
Published online: November 6, 2018
Processing time: 176 Days and 23 Hours
We present a case of adrenal CD in a 26-year-old female. The patient was referred to our hospital because of left flank pain for 1 wk. A computed tomography scan revealed a 4 cm × 3 cm well-defined mass, considered as a paraganglioma. A preoperative diagnosis of left adrenal neoplasm and urinary tract infection was made. The patient underwent anti-inflammatory therapy followed by an open operation to remove the mass in the left adrenal. Through analysis of the morphological pattern and immunohistochemical markers, a diagnosis of CD was made. During the 12-mo follow-up, there was no evidence of metastasis or recurrence. This case reminds clinicians that CD should be considered in the evaluation of an adrenal mass. Surgery is suggested for its therapeutic management.
Core tip: Castleman disease (CD), also known as giant lymph node hyperplasia or angiofollicular lymph node hyperplasia, is a highly heterogeneous clinicopathological entity belonging to the family of lymphoproliferative disorders. CD is commonly found in the mediastinum. Castleman-like masses in the adrenal grand are extraordinarily rare. We present a case of adrenal CD in a 26-year-old female. Through laparotomy, the tumor was removed. During a 12-mo follow-up, there was no evidence of metastasis or recurrence.
- Citation: Chen J, Yang C, Liang CZ. Detection of a unicentric type of Castleman-like mass at the site of adrenal grand: A case report and review of literature. World J Clin Cases 2018; 6(13): 683-687
- URL: https://www.wjgnet.com/2307-8960/full/v6/i13/683.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i13.683
Castleman disease (CD), also known as giant lymph node hyperplasia or angiofollicular lymph node hyperplasia, is a highly heterogeneous clinicopathological entity that belongs to the family lymphoproliferative disorders[1-3]. The first description of CD was made by Castleman[1] in 1956. As a complex lymphoproliferative disease, CD has been divided into two subtypes depending on its pathological classification, namely the hyaline vascular variant and the plasma cell variant.
The median age of patients was reported to be 43-years-old[4], with a slight female predilection[5]. The distribution of CD was reported as 60% in the thorax, 14% in the cervical area, 11% in the abdomen, and 4% in the axillary region[6-9]. Extrathoracic sites of CD had been reported in the pararenal region. However, adrenal CD is very rare[10].
The final diagnosis of CD at the site of adrenal grand is primarily based on histopathology and immunohistochemistry, although imaging and clinical symptoms are crucial for the diagnosis. The clinical diagnosis of CD is difficult. The primary treatment strategy for CD of the adrenal gland is surgery. We present a case of CD at the site of the adrenal gland in a 26-year-old female.
A 26-year-old female was referred to our department because of left flank pain for 1 wk. No additional symptoms were present. Pulse and blood pressure were within the normal range. A physical examination revealed pain on percussion of the left lumbar region.
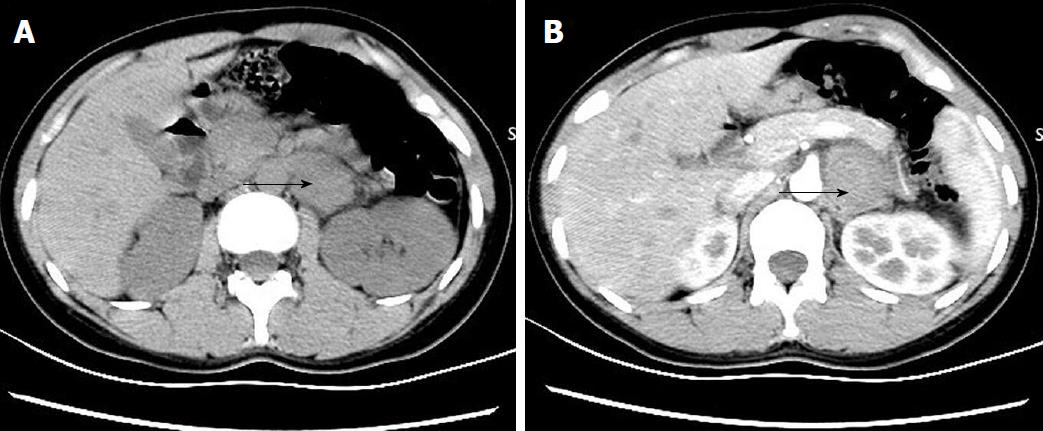
The biochemical findings were within normal ranges, including lactate dehydrogenase (2.45 mmol/L), albumin (44.4 g/L), creatinine (48 μmol/L), urinary catecholamine excretion, plasma renin activity, and plasma aldosterone. Routine urinalysis showed an increased number of leukocytes (181/μL), and fibrinogen (4.53 g/L) was also increased. Routine blood examination showed decreased hemoglobin (86 g/L) and hematocrit (28.6%). Ferritin (8.82 ng/mL) was low. The results of hormone measurements are listed in Table 1. Abdominal computed tomography (CT) revealed a 4 cm × 3 cm mass on the left adrenal region (Figure 1). No positive findings were revealed on chest X-ray.
| Hormone | Result | Normal or abnormal |
| Cortisol | 285.10 nmol/L | normal |
| ACTH | 23.90 pg/mL | normal |
| ALD (lying position) | 410.20 pmol/L | normal |
| ALD (standing position) | 527.90 pmol/L | normal |
| DA | 25.53 ng/mL | normal |
| E | 16 ng/mL | normal |
| NE | 38.68 ng/mL | normal |
A diagnosis of left adrenal neoplasm and urinary tract infection was made on the basis of physical examination, imaging, and laboratory tests.
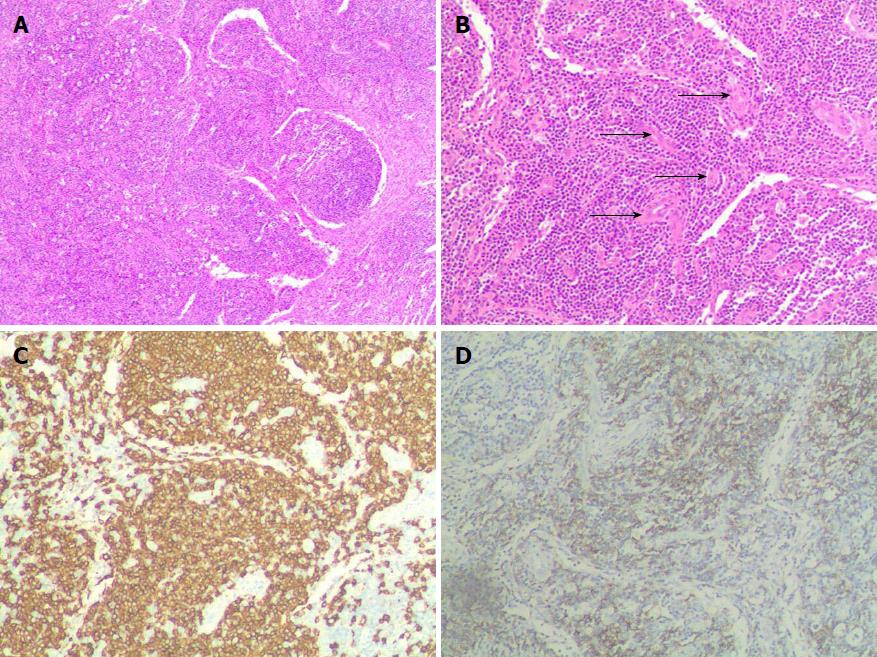
Through laparotomy, the tumor was removed. The size of the adrenal tumor was approximately 4 cm × 3 cm, with a hard texture and unclear lesion margins. The adrenal tumor was adherent to the peritoneum as well as the renal artery and vein. Microscopically, hematoxylin and eosin staining showed angiofollicular lymph node hyperplasia, interstitial edema, cystic changes and hyperplasia of collagen fibers (Figure 2A and B). Immunohistochemistry staining showed that the tumor cells were positive for CD20, CD79α, Pax5, CD2, CD3, CD5, CD21, CD23 and CD68. The tumor was negative for cyclinD1, Bcl2, CD15, CD30, syn, ck and cga (Figure 2C and D). Through the analysis of morphological pattern and immunohistochemical markers, a diagnosis of CD was made.
During a 12-mo follow-up, there was no evidence of metastasis or recurrence.
CD was first reported by Castleman in 1954 in a patient with a large mediastinal mass. It is a highly heterogeneous clinicopathological entity belonging to the family of lymphoproliferative disorders[1-3].
The etiology and pathogenesis of CD is largely unexplored. The crucial function of interleukin-6 (commonly known as IL-6) has been revealed in lymphovascular proliferation and systemic symptoms of CD. Some studies showed that abnormal expression of IL-6 in CD may explain several clinical manifestations of CD, including autoimmune manifestations and hyperglobulinemia, acute-phase reaction, and hypodermic microcytic anemia[11]. Other researchers reported that the constitutive over-expression of IL-6 in mice led to the CD phenotype. Therefore, IL-6 may play an important part in the pathogenesis of CD, and anti-IL-6 receptor antibody could be a therapeutic strategy for CD[12].
Histological evaluation plays a vital role in the exact diagnosis of CD. Histologically, the disease is primarily subclassified into three types: Hyaline vascular type, plasma cell variant, and mixed type. The characteristics of the hyaline vascular type include considerable enlarged lymphoid follicular proliferation at various levels of maturity[13]. In addition, lymphoid follicles are normally scattered throughout the tissue. The plasma cell type is almost related to the multicentric form of CD. This type shows less vascularity and is characterized by sheets of mature plasma cells within the interfollicular tissues surrounding larger germinal centers[14].
CD is ubiquitous but predominates at lymph node sites. The localized form is the most frequent. Localized CD of the hyaline vascular type is commonly asymptomatic. As in this case, adrenal CD has no specific presenting symptoms, including flank pain and hypertension[15]. In another study, the clinical manifestations of adrenal CD patients included poor appetite and weight loss[8]. However, the plasma cell type of localized CD and multicentric CD present systemic symptoms, including fever, night sweats, peripheral lymphadenopathy, weight loss, anemia, hepatosplenomegaly, and renal insufficiency. Disseminated CD has been described in association with polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes (known as POEMS) syndrome that results from a disorder of underlying plasma cells. It often displays aggressive behavior, including autoimmune anemia, sarcoidosis and amyloidosis[16].
The radiological appearance of CD is nonspecific. A homogeneous hypoechogenic formation is commonly shown on ultrasound[17]. Masses that are smaller than 5 cm have a homogeneous vascular appearance on CT, while larger masses are often mixed with the central low presence of fibrosis and necrosis[18]. According to the literature, on CT, adrenal CD often is rounded, well circumscribed and possesses some small calcifications without cystic or fatty areas. After intravenous injection of iodinated contrast agent, the tumor did not enhance and the adrenal gland was not visualized[19]. There are rare descriptions of MRI characteristics of CD. The signal characteristics of adrenal CD were similar to those reported for adrenal lymphoma: Hypointense compared with hepatic parenchyma on T1-weighted images and hyperintense on T2-weighted image[20]. Because the hyaline vascular type has three patterns of manifestation on CT, including solitary noninvasive mass, dominant infiltrating mass accompanied by lymphadenopathy and matted lymphodenopathy[21], it is difficult to distinguish CD from other malignant diseases solely on the basis of radiological methods.
Adrenal diseases include classic endocrine syndrome diseases, including Cushing syndrome, hyperaldosteronism and pheochromocytoma. Tumors of the adrenal gland may be accompanied by abdominal pain or an abdominal mass. The diagnosis of these diseases requires cautious endocrine assessment, and in many patients adrenal anatomy must be defined using adrenal imaging methods. If the examination of pulse, renal function, serum cortisol, electrolytes and urinary catecholamines are normal, the adrenal tumor may be diagnosed as nonfunctional. Under these circumstances, adrenal CD should be considered during the process of evaluating an adrenal mass[22]. Nevertheless, diagnosis of adrenal CD relies on histopathological examination.
Localized CD is primarily benign[23]. Localized CD usually requires surgical excision of the enlarged lymph node without additional treatment and it always responds well to surgical excision[24]. A systematic review of the role of surgical resection in localized CD showed that surgical resection was the most effective treatment for localized CD[25]. All general symptoms disappear after surgery and there were almost no relapses postoperatively[26].
CD is a rare disorder that is hard to diagnose early because of its nonspecific manifestations and radiological characteristics. Adrenal CD is extraordinarily rare and should be considered in the process of evaluating an adrenal mass.
This patient was referred to our department due to left flank pain for 1 wk, with no additional symptoms.
A 4 cm × 3 cm mass was found in the left adrenal region.
The findings of biochemical and hormone measurements were within the normal range.
Abdominal computed tomography (CT) of this patient revealed a 4 cm × 3 cm mass in the left adrenal region, and CT enhancement scan showed a mass in the left adrenal with no enhanced uniform.
Through the analysis of morphological pattern and immunohistochemical markers (the tumor cells were positive for CD20, CD79α, Pax5, CD2, CD3, CD5, CD21, CD23 and CD68), a diagnosis of CD was made.
The patient was treated by laparotomy.
CD was first reported by Castleman in 1954, in a patient with a large mediastinal mass. Adrenal CD is very rare. Interleukin-6 may play an important part in the pathogenesis of CD and anti-interleukin-6 receptor antibody could be a therapeutic strategy for CD.
CD is a rare disorder, for which is hard to achieve early diagnosis due to its nonspecific manifestation and radiological characteristics. Adrenal CD is extraordinarily rare and should be considered in the process of evaluating adrenal mass.
CARE Checklist (2013): The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): E
P- Reviewer: Coskun A, Demirbilek H, Dong AS, Kishimoto T S- Editor: Cui LJ L- Editor: Filipodia E- Editor: Tan WW
| 1. | Castleman B, Iverson L, Menendez VP. Localized mediastinal lymphnode hyperplasia resembling thymoma. Cancer. 1956;9:822-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 2. | Frizzera G. Castleman’s disease: more questions than answers. Hum Pathol. 1985;16:202-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 131] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Wilczak M, Kampioni MG, Szmeja J. Castleman’s disease-a case report. Videosurgery and Other Miniinvasive Techniques. 2011;551-553. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Dispenzieri A, Armitage JO, Loe MJ, Geyer SM, Allred J, Camoriano JK, Menke DM, Weisenburger DD, Ristow K, Dogan A. The clinical spectrum of Castleman’s disease. Am J Hematol. 2012;87:997-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 5. | Farruggia P, Trizzino A, Scibetta N, Cecchetto G, Guerrieri P, D’Amore ES, D’Angelo P. Castleman’s disease in childhood: report of three cases and review of the literature. Ital J Pediatr. 2011;37:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Zhong LP, Wang LZ, Ji T, Hu YH, Hu YJ, Ye WM, Li J, Sun J, Zhu HG, Li J. Clinical analysis of Castleman disease (hyaline vascular type) in parotid and neck region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:432-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Rabinowitz MR, Levi J, Conard K, Shah UK. Castleman disease in the pediatric neck: a literature review. Otolaryngol Head Neck Surg. 2013;148:1028-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Chen JH, Yu CY, Pai CY, Chan DC, Chen CJ, Yu JC, Liu YC. Castleman’s disease in the left upper retroperitoneal space mimicking an adrenal neoplasm: report of a case and literature review. Jpn J Clin Oncol. 2005;35:353-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Madan R, Chen JH, Trotman-Dickenson B, Jacobson F, Hunsaker A. The spectrum of Castleman’s disease: mimics, radiologic pathologic correlation and role of imaging in patient management. Eur J Radiol. 2012;81:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Modi P, Trivedi A, Gupta R, Rizvi SJ. Retroperitoneal pararenal Castleman’s tumor in an adolescent managed laparoscopically. J Endourol. 2008;22:2451-2454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Leger-Ravet MB, Peuchmaur M, Devergne O, Audouin J, Raphael M, Van Damme J, Galanaud P, Diebold J, Emilie D. Interleukin-6 gene expression in Castleman’s disease. Blood. 1991;78:2923-2930. [PubMed] |
| 12. | Katsume A, Saito H, Yamada Y, Yorozu K, Ueda O, Akamatsu K, Nishimoto N, Kishimoto T, Yoshizaki K, Ohsugi Y. Anti-interleukin 6 (IL-6) receptor antibody suppresses Castleman’s disease like symptoms emerged in IL-6 transgenic mice. Cytokine. 2002;20:304-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 103] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Iyer S, Bhatti MI, Halliday M. Castleman’s disease-A case report. Int J Surg Case Rep. 2010;1:25-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Roganović J, ĆOZA , Petra , Jonjić N. Castleman’s disease-case report. Pedijatrija Danas Pediatrics Today. 2013;44:551-553. |
| 15. | Frazier AA. Unicentric versus Multicentric Castleman Disease. Radiographics. 2016;36:1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Andhavarapu S, Jiang L. POEMS syndrome and Castleman disease. Blood. 2013;122:159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Bucher P, Chassot G, Zufferey G, Ris F, Huber O, Morel P. Surgical management of abdominal and retroperitoneal Castleman’s disease. World J Surg Oncol. 2005;3:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Meador TL, McLarney JK. CT features of Castleman disease of the abdomen and pelvis. AJR Am J Roentgenol. 2000;175:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Irsutti M, Paul JL, Selves J, Railhac JJ. Castleman disease: CT and MR imaging features of a retroperitoneal location in association with paraneoplastic pemphigus. Eur Radiol. 1999;9:1219-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Debatin JF, Spritzer CE, Dunnick NR. Castleman disease of the adrenal gland: MR imaging features. AJR Am J Roentgenol. 1991;157:781-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | McAdams HP, Rosado-de-Christenson M, Fishback NF, Templeton PA. Castleman disease of the thorax: radiologic features with clinical and histopathologic correlation. Radiology. 1998;209:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 122] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Müssig K, Horger M, Wehrmann M. Adrenal Castleman’s disease. Ann Hematol. 2007;86:63-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Saeed-Abdul-Rahman I, Al-Amri AM. Castleman disease. Korean J Hematol. 2012;47:163-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Aygun C, Tekin MI, Demirhan B, Peskircioglu CL, Agildere M, Ozkardes H. A case of incidentally detected Castleman’s disease with retroperitoneal paravertebral localization. Int J Urol. 2000;7:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Mitsos S, Stamatopoulos A, Patrini D, George RS, Lawrence DR, Panagiotopoulos N. The role of surgical resection in Unicentric Castleman's disease: a systematic review. Adv Respir Med. 2018;86:36-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Ren N, Ding L, Jia E, Xue J. Recurrence in unicentric castlemanâs disease postoperatively: a case report and literature review. Bmc Surgery. 2018;18:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |