Published online Nov 6, 2018. doi: 10.12998/wjcc.v6.i13.679
Peer-review started: April 13, 2018
First decision: June 4, 2018
Revised: July 12, 2018
Accepted: October 11, 2018
Article in press: October 12, 2018
Published online: November 6, 2018
Processing time: 207 Days and 1.1 Hours
To study a more micro-invasive procedure for patients having pancreatic duct stones (PDS). Till now, there has been no report of laparoscopic pancreatic duct incision and stone removal and T-type tube drainage for PDS in the English literature. An 82-year-old man suffered from subxiphoid pain associated with a dilated pancreatic duct (7 mm) containing one stone, but without a mass in the head of the pancreas. Laparoscopic pancreatic duct incision, stone removal, and T-type tube drainage were successfully performed without intraoperative or postoperative complications. An uneventful operation was performed with laparoscopically completed procedures in 160 min. The intraoperative loss of blood was around 50 mL. After patient a discharge on day 11, complete relief from the subxiphoid pain was reported at a follow-up visit 15 mo later. Laparoscopic pancreatic duct incision with stone removal and T-type tube drainage is applicable in carefully selected patients and can be effectively and safely used for the treatment of the abdominal pain of chronic pancreatitis.
Core tip: With improvements in laparoscopic surgery, patients with pancreatic duct stones (PDS) are increasingly undergoing laparoscopic treatment. However, no report is available of laparoscopic pancreatic duct incision, stone removal, and T-type tube drainage for PDS in the English literature. We applied this approach in such a case and suggest that this procedure is applicable and can be effectively and safely used for the treatment of the abdominal pain of chronic pancreatitis in strictly selected patients.
- Citation: Bai Y, Yu SA, Wang LY, Gong DJ. Laparoscopic pancreatic duct incision and stone removal and T-type tube drainage for pancreatic duct stone: A case report and review of literature. World J Clin Cases 2018; 6(13): 679-682
- URL: https://www.wjgnet.com/2307-8960/full/v6/i13/679.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i13.679
Pancreatic duct stone (PDS) is considered to be a complication of chronic pancreatitis (CP) that occur in approximately 50% of the cases[1]. Lateral pancreaticojejunostomy (LPJ) is a commonly performed procedure in pancreatic operations used for the treatment of CP that is usually endorsed in patients experiencing concomitant pain, with dilated and obstructed pancreatic duct, and inflammation in the left side’s proximity to the gastroduodenal artery[2,3]. LPJ is advantageous over other surgical techniques in that it allows better preservation of the endocrine and exocrine functions of the pancreas. However, minimally invasive surgery is rarely used for its completion due to the technical difficulties and anatomic intricacy which require advanced laparoscopic surgery competence. Nevertheless, with advancements in laparoscopic surgery, approximately 40 patients globally have undergone laparoscopic LPJ[4].
However, there is no report on laparoscopic pancreatic duct incision, stone removal, and T-type tube drainage for pancreatic duct stone treatment. Herein, we report our preliminary experience with this procedure.
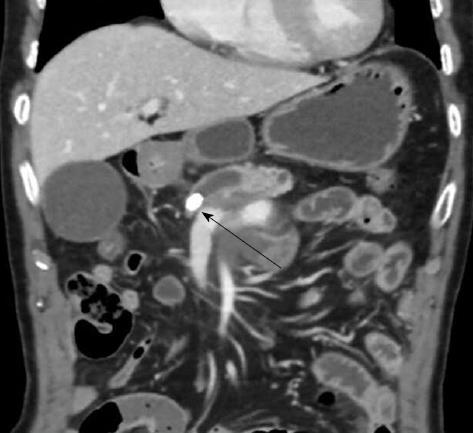
An 82-year-old man with a history of hypertension was referred to our Department of Hepatobiliary Pancreatic Surgery with a persisting subxiphoid pain of 12 h duration. There was no positive sign, except for tenderness in the epigastric region. The results of the laboratory tests, including determination of blood glucose levels, were almost within the normal range. Computed tomography of the upper abdomen revealed an atrophic pancreas with a dilated pancreatic duct containing a single stone located at the pancreatic neck; no mass in the pancreatic gland head or biliary dilatation was detected (Figure 1). The size of the stone was approximately 1.0 cm × 0.6 cm. Based on the clinical signs and test result, a diagnosis of pancreatic duct stone with CP was established.
Given the presence of only one stone in the pancreatic main duct, we elected to perform laparoscopic pancreatic duct incision and stone removal, followed by T-type tube drainage, under general anesthesia after obtaining informed consent from the patient.
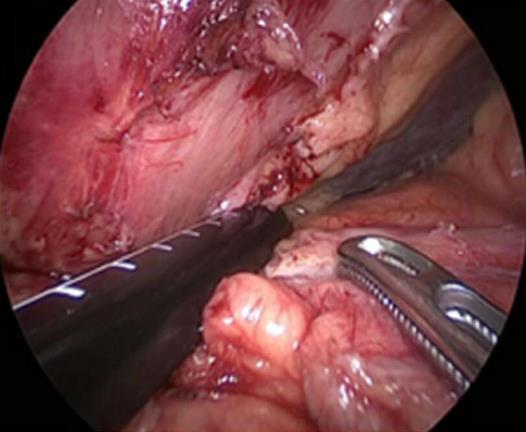
During the operation, the patient received prophylactic antibiotics intravenously, and intermittent pneumatic compression therapy and graduated compression stockings were applied to the lower limbs. After catheterization of patient, he was installed in a flat Lloyd-Davies position. The patient was tilted in a 30-degrees reverse Trendelenberg position during the operation by the use of two 5-mm ports, two 10-mm ports, and one 12 mm port (Figure 2).
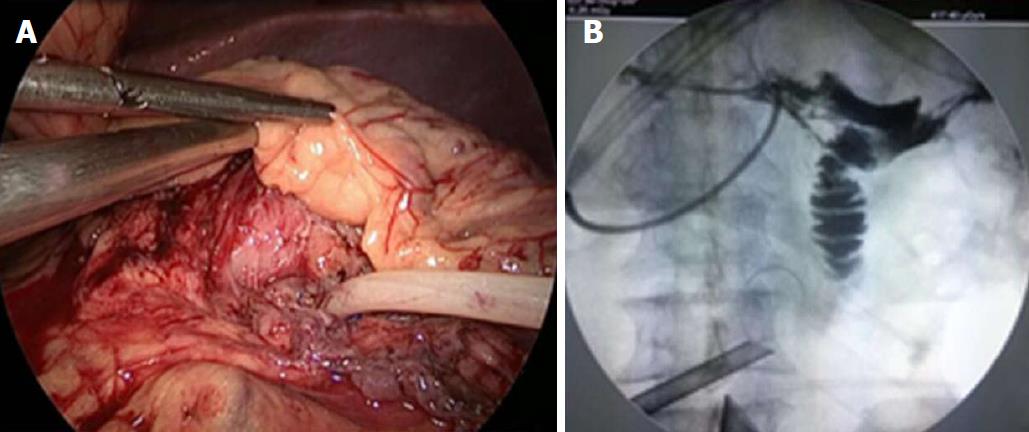
By an ultrasonically activated scalpel, the lesser sac was opened via the gastrocolic omentum. Then, mobilization of the gastric antrum was performed, followed by upward retraction of the stomach to expose the front surface of the pancreatic head to the gland body. The duct of the pancreas was located by ultrasound laparoscopy and opened (Figure 3). An initial opening was made above the gland neck by the joint use of an electrocoagulation and an ultrasonically activated scalpel, which was then prolonged further downstream and upstream to perform fillet opening from the head to the body of the pancreas. Next, the pancreatic duct was explored, and one stone was removed. One Fr14 T-type tube was inserted into the pancreatic main duct, of which the incised section was sutured discontinuously with a 4-0 Prolene stitch. Further, the pancreatic proximal duct was unobstructed, and no stone was present, as verified by intraoperative X-ray radiography through a T-type tube with 30% iohexol solution (Figure 4).
An uneventful operation was performed, and the laparoscopic procedures were concluded in 160 min with an approximate 50-mL intraoperative loss of blood. Neither intraoperative nor postoperative blood transfusion was necessary. Furthermore, the oral intake of fluids began on the first postoperative day (POD). The volume of pancreatic juice drained was about 150 mL per day. No complications occurred peri- or postoperatively. Eventually, the patient was discharged on day 11 postoperatively. The result of postoperative X-ray radiography through the T-type tube was identical to that obtained intraoperatively (Figure 5). The T-type tube was withdrawn two months after the operation. At the 15-mo post-operative follow-up, neither the subxiphoid pain nor the pancreatic duct stone had recurred.
LPJ is frequently performed for CP management, and laparoscopically performed LPJ is reported in previously published English-language specialized literature. However, laparoscopic pancreatic duct incision and stone removal with subsequent T-type tube drainage for pancreatic duct stone treatment has not been reported to date. Herein, we report the case of a patient suffering from PDS, who was treated using this approach successfully. The novel procedure described in the present paper has the following advantages: It allows a clear visual field, reduces tissue trauma, provides an easier operation course, shortens the operation time, and accelerates patient recovery.
The diverse etiology of CP is characterized by irreversible progressive pancreatic changes that result in the loss of its endocrine and exocrine functions. Continuous or episodic pain is the principal and most severe symptom of this disease which drastically lowers patient’s life quality. PDS aggravates or produces the distinctive pancreatic pain through pancreatic duct obstruction, upstream duct hypertension, and the sequential parenchymal hypertension. Surgical or endoscopic therapy aims at calculi elimination and ductal hypertension reduction, which results in pain relief and improved life quality.
Surgery, extracorporeal shock wave lithotripsy (ESWL), and endoscopic therapy are the present options for PDS treatment, although continuous disputes that have hampered the achievement of a unanimous endorsement.
A large number of investigations have supported that surgery is the most preferable and advantageous therapeutic option owing to its shorter continuation and lower hospitalization recurrence and expenses, along with promoted pain relief and easier repeated intervention. On the other hand, endoscopic treatment is considered a less invasive and effective modality despite its limitations for use in all patients. Nevertheless, the combination of endoscopic therapy and ESWL can be regarded as first-line treatment in high-risk patients for surgery or such with relevant indications[5].
Our initial experience with this case shows that laparoscopic pancreatic duct incision, stone removal, and T-type tube drainage is optimally used when a single stone is present in the pancreatic main duct. Laparoscopic ultrasonography is beneficial for locating the stone, and verification by intraoperative X-ray radiography through a T-type tube that the pancreatic duct is unobstructed is important. However, this study is a preliminary report; hence, further investigations including greater sample sizes and more prolonged follow-up periods are required to improve the surgical technique described herein and verify our initial results.
Surgery is the superior treatment modality of pancreatic duct stones (PDS). Patients with PDS have been increasingly undergoing laparoscopic lateral pancreaticojejunostomy over the last years. However, no report exists of laparoscopic pancreatic duct incision, stone removal, and T-type tube drainage for PDS.
Pancreatic duct stone.
Pancreatic tumor.
Chronic pancreatitis.
Pancreatic duct stone.
This case will enhance the use of more micro-invasive procedures by surgeons for carefully selected patients suffering from pancreatic duct stones.
The authors would like to thank Xian-zhong Qian and Bin Yang for their support provided during the present study.
CARE Checklist (2013) statement: We have adopted the guidelines of the CARE checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Han JH, Iqbal S, Richardson WS S- Editor: Cui LJ L- Editor: A E- Editor: Tan WW
| 1. | Rösch T, Daniel S, Scholz M, Huibregtse K, Smits M, Schneider T, Ell C, Haber G, Riemann JF, Jakobs R. Endoscopic treatment of chronic pancreatitis: a multicenter study of 1000 patients with long-term follow-up. Endoscopy. 2002;34:765-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 288] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 2. | Ceppa EP, Pappas TN. Modified puestow lateral pancreaticojejunostomy. J Gastrointest Surg. 2009;13:1004-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Tantia O, Jindal MK, Khanna S, Sen B. Laparoscopic lateral pancreaticojejunostomy: our experience of 17 cases. Surg Endosc. 2004;18:1054-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Khaled YS, Ammori MB, Ammori BJ. Laparoscopic lateral pancreaticojejunostomy for chronic pancreatitis: a case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 2011;21:e36-e40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Kim YH, Jang SI, Rhee K, Lee DK. Endoscopic treatment of pancreatic calculi. Clin Endosc. 2014;47:227-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |