Published online Sep 26, 2018. doi: 10.12998/wjcc.v6.i10.398
Peer-review started: April 19, 2018
First decision: June 4, 2018
Revised: June 22, 2018
Accepted: June 28, 2018
Article in press: June 28, 2018
Published online: September 26, 2018
Processing time: 160 Days and 5.6 Hours
A lumbar hernia is a rare entity, and a bilateral lumbar hernia is much rarer. From May 2015 to October 2017, we treated only three patients with bilateral lumbar hernias. One patient came to the hospital presenting with right-sided abdominal pain, and the other two patients presented with bilateral lumbar masses. The previous bilateral lumbar hernia reported in the literature was repaired by open surgery. The laparoscopic approach via the transabdominal preperitoneal (TAPP) procedure with the self-gripping Parietex ProGrip™ mesh was performed at our center. The laparoscopic repair was conducted by a skilled hernia surgeon, and was successfully performed in the three patients. The patients resumed a semi-liquid diet and had no activity restriction after six hours following the operation. No antibiotics were used after the surgery. The operative times of the three patients were 120 min, 85 min, and 130 min. The blood loss volumes of the three patients were 20 mL, 5 mL, and 5 mL. The visual analogue scale pain scores of the three patients were 1, 2, and 2 on postoperative day 1, and were 1, 2, and 1 on postoperative day 3. No perioperative complications, such as bulge, wound infection and hematoma, occurred after the surgery. All of the patients were discharged on the third day after the operation. There was no chronic pain and no hernia recurrence during the follow-up. This study showed that the laparoscopic TAPP approach with the self-gripping mesh is safe and feasible, and can be considered an alternative method for the treatment of bilateral lumbar hernias.
Core tip: This study reports the successful implementation of a transabdominal preperitoneal procedure with self-gripping mesh for the management of a bilateral lumbar hernia. There were no adverse events, chronic pain or recurrence occurring in any of the patients. The findings confirm the safety and feasibility of the technique, and support the application of the laparoscopic approach for bilateral lumbar hernia repair.
- Citation: Huang DY, Pan L, Chen MY, Fang J. Laparoscopic repair via the transabdominal preperitoneal procedure for bilateral lumbar hernia: Three cases report and review of literature. World J Clin Cases 2018; 6(10): 398-405
- URL: https://www.wjgnet.com/2307-8960/full/v6/i10/398.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i10.398
Lumbar hernias, which are rare abdominal wall hernias, are the protrusion of the extraperitoneal fat or intra-abdominal contents through a defect in the posterolateral abdominal wall. The existence of lumbar hernias was first described by Cavallaro et al[1], and the first case was reported by Moreno-Egea et al[2] in 1731. The proportion of lumbar hernias to all abdominal hernias is less than 1.5%, and most of them are unilateral[3,4]. To date, approximately 300 cases of lumbar hernias have been reported in the world[2], and cases of bilateral lumbar hernias are even rarer[5,6]. Open hernia repair, which is used as the conventional approach, has been proven to be a safe and effective treatment option. Currently, with the development of laparoscopic technology, laparoscopic herniorrhaphy is increasingly used for the treatment of lumbar hernias[7,8]. Compared with the conventional approach, laparoscopic lumbar hernia repair has several advantages, such as mild postoperative pain, fewer perioperative complications, a shorter hospital stay, a faster recovery to normal activity, and a similar recurrence rate[9]. Nevertheless, there is no relevant standard in the detailed procedures of laparoscopic lumbar hernia surgery, nor in the type and fixation of meshes, due to the limited number of laparoscopic surgeries that have been performed. All of the currently reported bilateral lumbar hernias were repaired by open surgery[10,11]. As with inguinal hernias, the laparoscopic technique in bilateral lumbar hernia repair is expected to be superior compared with open surgery, as long as the technique is available. Recently, we completed three cases of laparoscopic bilateral lumbar hernia repair via the transabdominal preperitoneal (TAPP) procedure using self-gripping mesh, and demonstrated the feasibility of this technique. To the best of our knowledge, this is the first report of the laparoscopic approach for the treatment of bilateral lumbar hernias. In addition, this report is followed by a literature review of lumbar hernias with regard to their etiologies, anatomical characteristics, clinical features, diagnoses, and surgical treatments.
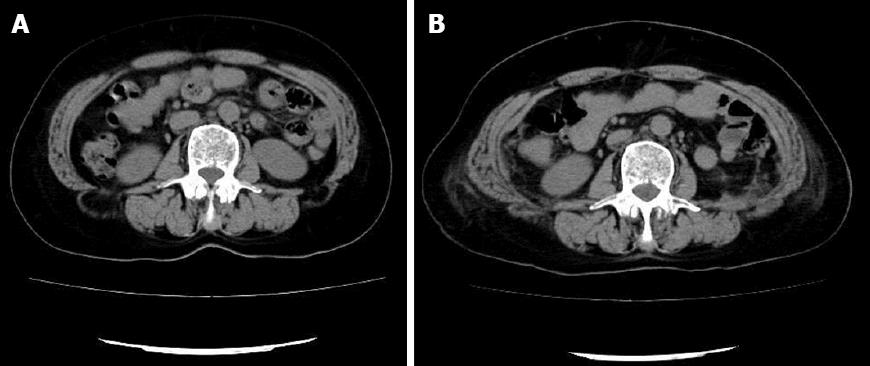
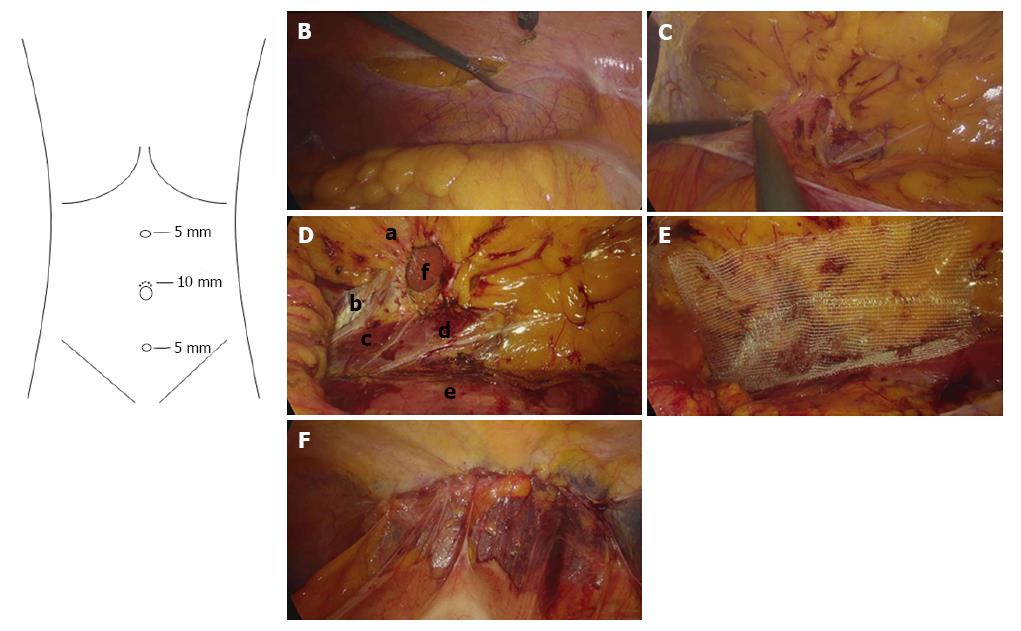
From May 2015 to October 2017, three patients were diagnosed with bilateral lumbar hernias and treated. The baseline characteristics of the patients are shown in Table 1. Computed tomography imaging demonstrated the existence of bilateral lumbar hernias (Figure 1A). For the operation, the patient was placed under general anesthesia in a 60° lateral position. The first 10 mm trocar was introduced by a mini-incision above the umbilicus for insufflation of carbon dioxide and for a 30° angled laparoscope. The other trocars were placed under direct vision. The second 5 mm trocar was introduced at the midpoint of the xiphoid and umbilicus, and the third 5 mm trocar was introduced at the midpoint of the umbilicus and pubic symphysis (Figure 2A). The ascending colon or descending colon was clamped off with non-injury clamps to maintain tension. The peritoneum was cut above the paracolic sulci, and the extraperitoneal tissue was separated to fully expose the defect and hernia contents (Figure 2B). The hernia contents, such as the colon and mesentery from the defect, were carefully divided and then returned completely (Figure 2C). Subsequently, the preperitoneal space along the midline was freed to expose the psoas major. The head and tail sides of the psoas major were freed to approximately 6 cm in length (Figure 2D). A 15 cm × 9 cm self-gripping Parietex ProGrip ™ mesh (Sofradim Production, Trévoux, France) was fully unfolded and placed onto the psoas major (Figure 2E). The long axis of the patch was consistent with the direction of the psoas major, and the center of the patch was consistent with the defect. The margin of the patch overlapped with the defect for at least 3 cm in every direction. Next, 2-0 Prolene was used to suture and reinforce the four corners of the patch when the defect was relatively large, and a 3-0 absorbable suture-line was used to close the peritoneum with a continuous suture (Figure 2F). Carbon dioxide was released, each trocar was pulled out, and the patient’s position was adjusted to the contralateral position. Then, the contralateral lumbar hernia was repaired in the same manner. Finally, no intraperitoneal or retroperitoneal drain was placed. All of the operations were successful, and none of the patients required a conversion to laparotomy. The patients resumed a semi-liquid diet and had unlimited activity at six hours following the operation. No antibiotics were used either before or after the surgery. The relative perioperative data are shown in Table 2. All of the patients were discharged on the third day after the operation. There was no chronic pain and no hernia recurrence during the six month follow-up.
| Case No. | Age (yr) | Sex | BMI (kg/m2) | Chief complaint | Physical examination | Past history |
| 1 | 70 | F | 23.3 | Finding bilateral lumbar masses for approximately 1 mo | Bilateral lumbar masses (left: 5 cm × 4 cm; right: 4 cm × 4 cm), reducible | No surgery and/or trauma of the abdomen and waist |
| 2 | 68 | F | 31.1 | Right-sided abdominal pain for 1 mo | No abnormal signs | |
| 3 | 69 | F | 24.0 | Finding bilateral lumbar masses for approximately 8 mo | Bilateral lumbar masses (left and right: 3 cm × 2 cm), irreducible |
| Case No. | ASA | Hernia content | Operative time (min) | Blood loss (mL) | VAS/POD1 | VAS/POD3 | Complications | Hospital stay (d) | Chronic pain | Recurrence |
| 1 | II | Colon, mesentery | 120 | 20 | 1 | 1 | No | 3 | No | No |
| 2 | II | Colon, mesentery | 85 | 5 | 2 | 2 | No | 3 | No | No |
| 3 | II | Mesentery | 130 | 5 | 2 | 1 | No | 3 | No | No |
Here, we reported the first case of performing the laparoscopic approach for the treatment of bilateral spontaneous lumbar hernias. Considering the rarity of spontaneous lumbar hernias, we included a literature review of lumbar hernias to better understand the disease. We have conducted a literature search on PubMed and found 14 papers about laparoscopic repair of spontaneous lumbar hernias, which are presented in Table 3.
| Ref. | Size | Technique | Mesh | Fixation |
| 1997, Heniford et al[12] | 4 × 3 | TAPP | PTFE | Sutures |
| 1997, Bickle et al[3] | 3 × 3 | TAPP | PPL | Tacks |
| 2002, Postema et al[13] | - | TEP | PPL | Tacks |
| 2003, Habib[14] | 3 × 4 | TAPP | PPL | Tacks |
| 2004, Grauls et al[15] | 3 × 5 | TAPP | PPL | Tacks |
| 2005, Ipek et al[16] | 8 × 10 | TAPP | PTFE | Tacks + sutures |
| 2011, Lim et al[17] | 5 × 6 | TEP | PPL | Tacks + sutures |
| 2011, Nam et al[18] | 3 × 5 | TAPP | PPL | Tacks |
| 2013, Suarez et al[19] | - | TAPP | - | Tacks |
| 2014, Wei et al[20] | 3 × 3 | TEP (Single incision) | PPL | Tacks |
| 2015, Walgamage et al[4] | 5 × 5 | TAPP | PPL | Tacks |
| 2016, Agresta et al[21] | - | TAPP | Composite PPL | Tacks |
| 2017, Claus et al[22] | 1.5 × 2 | TAPP | PPL | Tacks |
| 2018, Sarwal et al[23] | 3 × 3 | TAPP | PPL | Tacks + fibrin sealent |
According to the underlying cause, lumbar hernias can be divided into primary lumbar hernias and secondary lumbar hernias. Primary lumbar hernias mostly occur in infancy and are often associated with an abnormal development of bones and abdominal muscles[24]. The majority of secondary lumbar hernias occur in middle-aged and elderly people, and the causes of secondary lumbar hernias include trauma, infection, surgery, etc. Surgery is the main cause of secondary lumbar hernias, especially surgeries using a back approach, such as nephrectomy, latissimus dorsi muscle transplantation and lumbar incision[25]. If some important anatomical structures of the back are not protected well, or anatomical structures of man-made destruction are not closed during the operation, postoperative lumbar hernias form relatively easily[19]. In addition, long-term cough, constipation, and other factors that cause increased intra-abdominal pressure are high-risk factors for secondary lumbar hernias[26-28].
Spontaneous lumbar hernias can be divided into the superior lumbar triangle hernias (Grynfeltt) and inferior lumbar triangle hernias (Petit), according to the location of the abdominal defect, both of which are naturally weakened areas in the dorsal abdominal wall[1]. Grynfeltt’s triangle is located below the 12th rib, and is limited laterally by the internal oblique muscle and medially by the erector spinae muscle, with the transversus abdominis aponeurosis serving as its floor[29]. Sometimes, the serratus posterior inferior is also involved in the formation of the upper edge of Grynfeltt’s triangle. Petit’s triangle is limited medially by the latissimus dorsi, laterally by the external abdominal oblique muscle, and inferiorly by the iliac crest, with the internal oblique aponeurosis serving as its floor[29]. Due to the protective effect of internal oblique aponeurosis on Petit’s triangle, the incidence of a Petit hernia is lower in comparison with a Grynfeltt hernia[1]. Additionally, the hernia contents may be extraperitoneal adipose tissue or various intraperitoneal organs, such as the colon, small intestine, kidney, liver, stomach, etc.[30,31]. During the operations, especially during fixation, more attention should be paid to protecting nerves near the superior lumbar triangle, such as the ilioinguinal nerve, lateral femoral cutaneous nerve and genitofemoral nerve, to avoid chronic pain after surgery[19].
The majority of patients arrive at the hospital because of a protruding bulge in the posterior abdominal wall without having any subjective symptoms. A small subgroup of patients has some atypical symptoms, such as a backache and intercostal neuralgia, due to the oppression of the inner contents of the lumbar hernia. Very few patients with lumbar hernias show specific symptoms, such as bowel obstruction, hydronephrosis and hydroureter, because the contents are relevant to the abdominal organ[32-34]. In our study, two patients presented with a semispherical bulge in the back, while one patient presented with unexplained abdominal pain. A lumbar hernia should be distinguished from a lipoma, fibroma, hematoma, abscess and retroperitoneal tumor[16]. The main differences are that a lumbar hernia is reducible and that it will become larger when patients hold their breath to increase intra-abdominal pressure, while the mass in patients with the other diseases mentioned above is commonly unchanged. Nowadays, with the rapid development of radiation technology, an abdominal CT scan is playing an increasing role in assessing the complexity, actual contents, site and size of the hernia to formulate a suitable operative plan, although the diagnosis of lumbar hernias is based on clinical manifestation[2,35].
Although lumbar hernias are a rare clinical entity, the surgical procedure for lumbar hernias is constantly evolving and changing ever since lumbar hernia repair was first reported by Owen in 1888. Open surgery for a lumbar hernia involves the following stages: direct suture repair, the Dowd technique, and mesh repair. Direct suture repair: after the contents of the hernia are returned and the hernia sac is ligated, the adjacent fascia and muscle are directly overlapped with a nonabsorbable suture. Direct suture repair is suitable for lumbar hernias with a defect < 2.5 cm in diameter, and is mainly used for the repair of primary lumbar hernias in children[36,37]. When the diameter of the defect is too large, a direct suture will create great tension, which can easily lead to the postoperative recurrence of hernias[38].
In this method, the transversalis fascia is imbricated, and the defect is covered with a flap from the fascia and muscle[39]. This method effectively relieves local tension and reduces the recurrence rate of large lumbar hernias. However, the disadvantages of this method are that the operation is pretty complicated and the damage to the surrounding tissue is large. Complications, such as local hematoma and ischemic necrosis of the flaps, easily occur and will affect the overall success of the operation[38].
The creation of an artificial patch has changed the surgical method of traditional hernia repair. In 1963, Hafner et al[40] first used Marlex mesh to repair Petit’s lumbar hernia with an uneventful postoperative course. Mesh repair reduces the tension during the repair of large hernias and avoids flap transplantation, which is quite traumatic and complicated, thus improving the success rate of herniorrhaphy and decreasing the postoperative recurrence rate. Nevertheless, mesh repair also has its disadvantages. Synthetic materials do not have the ability to resist infection. When the strangulated hernia combines with intestinal necrosis, artificial patches easily cause infection. Once the infection occurs, the patches must be removed.
Upon reviewing the English literature, tension-free open herniorrhaphy with a synthetic mesh is currently the most widely-accepted surgery for lumbar hernia repair, and the optimal location for mesh placement is the preperitoneal space[38]. As with most abdominal wall hernias, the same principles apply to a lumbar hernia. The mesh should overlap the defect by 3-5 cm and should be fixed with nonabsorbable sutures. Although laparoscopic techniques are increasingly being used to repair hernias, open surgery still has advantages. For example, when the defect is very large, open surgery can use the stitches to directly close the abdominal wall defect for reinforcement. In addition, two meshes can be respectively placed on the peritoneum and muscle. The mesh can be fixed onto the iliac crest to decrease recurrence.
With the development of the laparoscopic technique, surgeons began to use a minimally-invasive surgery approach to repair lumbar hernias. Since Burick et al[7] reported the first case of laparoscopic lumbar hernia repair in 1996, relevant reports are increasing in number[41]. The patient is commonly placed in a lateral position with 45° elevation of the same side as the hernia to allow for the abdominal viscera to fall due to gravity to increase the exposure. As with open surgery, the placement of the patch through the laparoscopic approach is also in the preperitoneal space. Operating under direct vision can create a larger dissection area compared with open surgery, allowing the patch to be placed more accurately and flatter, and reducing the risk for injury to blood vessels and nerves. Laparoscopic lumbar hernia repair can be performed in a variety of ways. Currently, the TAPP and totally extraperitoneal techniques are the major laparoscopic procedures for lumbar hernias[17,22]. Surgeons can directly observe the abdominal viscera via the TAPP approach, thus reducing the possibility of damaging these viscera. Meanwhile, TAPP provides a large operative space for ease of operation, can deal with relatively large defects, and is appropriate for the treatment of bilateral hernias. However, this procedure requires cutting and suturing the peritoneum. Totally extraperitoneal: under some conditions, for example, when the defect is small, totally extraperitoneal seems to be more convenient than TAPP because the incision and suturing of the peritoneum are not required, and because there is less interference with the abdominal cavity[42]. However, when the defect is large, it is difficult to place and fix the patch due to insufficient working space, and if only three ports are placed along the middle line, it is not suitable for bilateral lumbar hernias because of significant surgical injury. Sun et al[43] have performed the transabdominal partial extraperitoneal technique using an expanded polytetrafluoroethylene bilaminar mesh in laparoscopic lumbar hernia repair, which seems to be an alternative choice for the treatment of large lumbar hernias. Regardless of the type of surgical procedure, direct suturing of the defect via the laparoscopic approach is not recommended. The selection and fixation of meshes are currently inconclusive. In the case of ensuring peritoneal integrity, polypropylene meshes are used by most surgeons. When the peritoneum cannot be completely closed and the patch is exposed to the abdominal cavity, a mesh that can prevent intestinal adhesion, such as a composite mesh with expanded polytetrafluoroethylene, must be used. The ways to fix the mesh in lumbar hernia repair are similar to those for fixing anterior abdominal hernias, which include staples, sutures, transmural sutures, and combinations of these tools[9]. Although these methods are effective based on the absence of recurrence, it is difficult to determine which one is the most superior because of the small number of cases. No matter what method is used for the fixation, special attention should be paid to the avoidance of nerve injury.
Bilateral primary lumbar hernias are rare because the bilateral superior and inferior lumbar triangles are generally asymmetrical. At present, all the bilateral lumbar hernias in the cases reported in the literature have been repaired by open surgery. To our knowledge, the laparoscopic procedure is superior for the management of bilateral inguinal hernias compared with open surgery[44,45]. Based on the above consideration, we decided to use TAPP to repair bilateral lumbar hernias, despite the fact that there is no literature reporting the use of laparoscopic surgery for bilateral lumbar hernias. The operation was successfully performed in three patients, with mild postoperative pain, a shorter length of stay, and fewer complications compared with open surgery. We have observed the superiority of laparoscopic technique for bilateral lumbar hernias, its perioperative safety, and postoperative efficacy. The key points for this laparoscopic procedure are the location of the incision and the selection of the patient position. In the reported cases of lumbar hernia repair, the location of the observation ports was commonly in the umbilicus, while the location of the utility ports was not uniform. One method includes the two utility ports being placed along the middle line, approximately 5 cm from the observing port to reach both sides. Another method involves placing the ports along the midclavicular line on the ipsilateral side of the hernia. If the latter is used, five incisions must be performed for the bilateral lumbar hernia repair. Since none of the three patients were obese, we chose the first method in order to reduce the number of incisions. Our operations were successful, and the choice of incisions did not interfere with our surgeries. However, we think that if the patient is obese, this option for the incisions may cause complications for the operation. For obese patients, five incisions may be more appropriate.
As for the patient’s position, if the patient is in a horizontal position, the lateral tilt of the operation table can also be used to partly achieve the effect of the lateral decubitus position, with no re-sterilization or drape required during the operation. However, if all of the trocars are located in the midline, exposing the preperitoneal space can be difficult, especially when the space is dissected toward the midline. Therefore, we decided to use the lateral position that is reported in most of the literature. After a one-sided lumbar hernia was repaired completely, we temporarily bandaged the incision and re-sterilized, draped and inserted trocars to repair the other lumbar hernia. Generally, there is no difference between our operation and the laparoscopic repair of a unilateral lumbar hernia.
In the currently reported laparoscopic lumbar hernia repair literature, meshes need to be fixed with sutures or staples, and in the process of fixing the meshes, the most important thing is to avoid damaging the nerves. Although nerves can be seen directly before the patches are placed, it is not easy to observe when the patches have been placed and partially fixed. At present, there are no reports of chronic pain after laparoscopic lumbar hernia repair, but the result is catastrophic if it does happen. To avoid nerve damage, we used self-gripping meshes in our study, which is also the first report to use this patch for lumbar hernia repair. Birk et al[46] performed TAPP using these self-gripping meshes for 220 inguinal hernias that had a follow-up of 12 mo, and confirmed that the mesh is safe and efficient with low pain and a low recurrence rate. The meshes do not require additional fixation for small defects, and we only needed to sew four stitches at the edges of the mesh for large defects. This not only reduces or avoids the possibility of nerve damage, but also makes the surgeries faster and easier. In addition, the patients in our study only had mild pain after the operation and had no chronic pain or recurrence at follow-up.
In conclusion, a lumbar hernia is considered to be a clinically rare entity, while a bilateral lumbar hernia is even rarer. As with bilateral inguinal hernia repair, laparoscopic bilateral lumbar hernia repair via TAPP is technically feasible. Meanwhile, the use of self-gripping mesh can reduce or even avoid nerve damage and simplify the operation. To the best of our knowledge, this study is the first report of bilateral lumbar hernias that were repaired by the laparoscopic approach using self-gripping mesh without any complications, implying that it is a safe and feasible surgical procedure.
Two patients presented with bilateral lumbar masses without any clinical symptoms. One patient presented with right-sided abdominal pain, but she did not show any abdominal signs.
Most people have a bilateral lumbar bulge with or without symptoms, such as abdominal pain. The bulge will become more apparent after a long period of standing, coughing, or holding one’s breath. A contralateral bulge will shrink after patients are placed in a lateral position.
Lumbar subcutaneous lipoma.
An abdominal computed tomography scan showed that the abdominal wall beside the two kidneys is weak, with part of the abdominal mesentery or colon included.
Laparoscopic repair via the transabdominal preperitoneal procedure for a bilateral lumbar hernia.
A bilateral lumbar hernia was previously repaired by open surgery, which is the first report of the use of laparoscopic technique for the repair of a bilateral lumbar hernia.
Our study demonstrates that it is safe and efficient to use laparoscopic repair via transabdominal preperitoneal for a bilateral lumbar hernia, and provides an alternative way for the repair of bilateral lumbar hernias. Surgeons can use our method as long as they are proficient in laparoscopic repair of a unilateral lumbar hernia.
CASE Checklist (2013): The authors have confirmed that the paper conforms to the guidelines of the CASE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Akbulut S, Demetrashvili Z, Hussain A, Losanoff JE S- Editor: Cui LJ L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Cavallaro G, Sadighi A, Paparelli C, Miceli M, D’Ermo G, Polistena A, Cavallaro A, De Toma G. Anatomical and surgical considerations on lumbar hernias. Am Surg. 2009;75:1238-1241. [PubMed] [Cited in This Article: ] |
| 2. | Moreno-Egea A, Baena EG, Calle MC, Martínez JA, Albasini JL. Controversies in the current management of lumbar hernias. Arch Surg. 2007;142:82-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Bickel A, Haj M, Eitan A. Laparoscopic management of lumbar hernia. Surg Endosc. 1997;11:1129-1130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Walgamage TB, Ramesh BS, Alsawafi Y. Case report and review of lumbar hernia. Int J Surg Case Rep. 2015;6C:230-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Okiemy E, Mackoumbounkounka EL. Hernie lombaire bilaterale du triangle de petit: A propos d’un cas. Médecine Dafrique Noire. 2006;. [Cited in This Article: ] |
| 6. | Lazier J, Mah JK, Nikolic A, Wei XC, Samedi V, Fajardo C, Brindle M, Perrier R, Thomas MA. Bilateral congenital lumbar hernias in a patient with central core disease--A case report. Neuromuscul Disord. 2016;26:56-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Burick AJ, Parascandola SA. Laparoscopic repair of a traumatic lumbar hernia: a case report. J Laparoendosc Surg. 1996;6:259-262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Obregón L, Ruiz-Castilla M, Binimelis MM, Guinot A, García V, Puig O, Barret JP. Laparoscopic repair of non-complicated lumbar hernia secondary to a latissimus dorsi flap. J Plast Reconstr Aesthet Surg. 2014;67:407-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Moreno-Egea A, Alcaraz AC, Cuervo MC. Surgical options in lumbar hernia: laparoscopic versus open repair. A long-term prospective study. Surg Innov. 2013;20:331-344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Radhakrishna V, Tanga SM. Bilateral superior lumbar hernias: a case report and review of literature. Int J Surg. 2017;4:1472-1474. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Parreira JM, Chibata M, Saucedo N, Colatusso RP, Paciornik R. Bilateral spiegelian hernia: case report and literature review. Abcd Arqbrascirdig. 2007;20:208-211. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Heniford BT, Iannitti DA, Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Arch Surg. 1997;132:1141-1144. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 90] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Postema RR, Bonjer HJ. Endoscopic extraperitoneal repair of a Grynfeltt hernia. Surg Endosc. 2002;16:716. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Habib E. Retroperitoneoscopic tension-free repair of lumbar hernia. Hernia. 2003;7:150-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Grauls A, Lallemand B, Krick M. The retroperitoneoscopic repair of a lumbar hernia of Petit. Case report and review of literature. Acta Chir Belg. 2004;104:330-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Ipek T, Eyuboglu E, Aydingoz O. Laparoscopic management of inferior lumbar hernia (Petit triangle hernia). Hernia. 2005;9:184-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Lim MS, Lee HW, Yu CH, Yang DH. Laparoscopic total extraperitoneal repair of lumbar hernia. J Korean Surg Soc. 2011;81:287-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Nam SY, Kee SK, Kim JO. Laparoscopic transabdominal extraperitoneal mesh repair of lumbar hernia. J Korean Surg Soc. 2011;81 Suppl 1:S74-S77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Suarez S, Hernandez JD. Laparoscopic repair of a lumbar hernia: report of a case and extensive review of the literature. Surg Endosc. 2013;27:3421-3429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Wei CT, Chen YS, Sun CK, Hsieh KC. Single-incision laparoscopic total extraperitoneal repair for a Grynfeltt hernia: a case report. J Med Case Rep. 2014;8:16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Agresta F, Marzetti A, Vigna S, Prando D, Porfidia R, Di Saverio S. Repair of primary and incisional hernias using composite mesh fixed with absorbable tackers: preliminary experience of a laparoscopic approach with a newly designed mesh in 29 cases. Updates Surg. 2017;69:493-497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Claus CMP, Nassif LT, Aguilera YS, Ramos EB, Coelho JCU. Laparoscopic repair of lumbar hernia (grynfelt): technical description. Arq Bras Cir Dig. 2017;30:56-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Sarwal A, Sharma A, Khullar R, Soni V, Baijal M, Chowbey P. Primary lumbar hernia: A rare case report and a review of the literature. Asian J Endosc Surg. 2018;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Sharma A, Pandey A, Rawat J, Ahmed I, Wakhlu A, Kureel SN. Congenital lumbar hernia: 20 years’ single centre experience. J Paediatr Child Health. 2012;48:1001-1003. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Reggio E, Sette MJ, Lemos R, Timm O Jr, Junqueira RG. Lumbar hernia following percutaneous nephrolitotomy. Clinics (Sao Paulo). 2010;65:1061-1062. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Xu T, Zhang S, Wang H, Yu W. Lumbar hernia associated with chronic obstructive pulmonary disease (COPD). Pak J Med Sci. 2013;29:874-876. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Woolbert A, Calasanz ER, Nazim M. Traumatic lumbar visceral herniation in a young woman. Int J Surg Case Rep. 2013;4:1061-1063. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P. Lumbar hernia: surgical anatomy, embryology, and technique of repair. Am Surg. 2009;75:202-207. [PubMed] [Cited in This Article: ] |
| 29. | Armstrong O, Hamel A, Grignon B, NDoye JM, Hamel O, Robert R, Rogez JM. Lumbar hernia: anatomical basis and clinical aspects. Surg Radiol Anat. 2008;30:533-537; discussion 609-610. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Kim J, Oh MM, Kim JJ, Moon D G. Delayed repair of a traumatic lumbar hernia with renal rupture. Am Surg. 2012;78:E295-E296. [PubMed] [Cited in This Article: ] |
| 31. | Teo KA, Burns E, Garcea G, Abela JE, McKay CJ. Incarcerated small bowel within a spontaneous lumbar hernia. Hernia. 2010;14:539-541. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Hide IG, Pike EE, Uberoi R. Lumbar hernia: a rare cause of large bowel obstruction. Postgrad Med J. 1999;75:231-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | Presti JC Jr, Narayan P. Lumbar herniation of the kidney. J Urol. 1988;140:586-587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Willcox MJ. Lumbar Herniation of Kidney following Iliac Crest Bone Harvest. Case Rep Surg. 2016;2016:5365647. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Chan K, Towsey K, Cavallucci D, Green B. Traumatic lumbar hernia repair: experience at the Royal Brisbane and Women’s Hospital. Hernia. 2017;21:317-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Wakhlu A, Wakhlu AK. Congenital lumbar hernia. Pediatr Surg Int. 2000;16:146-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Rattan KN, Agarwal A, Dhiman A, Rattan A. Congenital Lumbar Hernia: A 15-Year Experience at a Single Tertiary Centre. Int J Pediatr. 2016;2016:7162475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Cavallaro G, Sadighi A, Miceli M, Burza A, Carbone G, Cavallaro A. Primary lumbar hernia repair: the open approach. Eur Surg Res. 2007;39:88-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 39. | Dowd CN. CONGENITAL LUMBAR HERNIA, AT THE TRIANGLE OF PETIT. Ann Surg. 1907;45:245-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 40. | Hafner CD, WYLIE JH Jr, BRUSH BE. Petit’s lumbar hernia: repair with Marlex mesh. Arch Surg. 1963;86:180-186. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 41. | Links DJ, Berney CR. Traumatic lumbar hernia repair: a laparoscopic technique for mesh fixation with an iliac crest suture anchor. Hernia. 2011;15:691-693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Meinke AK. Totally extraperitoneal laparoendoscopic repair of lumbar hernia. Surg Endosc. 2003;17:734-737. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 43. | Sun J, Chen X, Li J, Zhang Y, Dong F, Zheng M. Implementation of the trans-abdominal partial extra-peritoneal (TAPE) technique in laparoscopic lumbar hernia repair. BMC Surg. 2015;15:118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 44. | Feliu X, Clavería R, Besora P, Camps J, Fernández-Sallent E, Viñas X, Abad JM. Bilateral inguinal hernia repair: laparoscopic or open approach? Hernia. 2011;15:15-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 45. | Wauschkuhn CA, Schwarz J, Boekeler U, Bittner R. Laparoscopic inguinal hernia repair: gold standard in bilateral hernia repair? Results of more than 2800 patients in comparison to literature. Surg Endosc. 2010;24:3026-3030. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Birk D, Hess S, Garcia-Pardo C. Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia. 2013;17:313-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |