Published online Jul 16, 2017. doi: 10.12998/wjcc.v5.i7.299
Peer-review started: November 13, 2016
First decision: February 17, 2017
Revised: March 2, 2017
Accepted: March 21, 2017
Article in press: March 22, 2017
Published online: July 16, 2017
Cerebral abscess is a potentially fatal neurosurgical condition, despite improvements in technology, new antimicrobial agents and modern neurosurgical instruments and techniques. I report the case of a 64-year-old woman, affected by a right frontobasal brain abscess, compressing the homolateral frontal horn of lateral ventricle, with a second mass partially occupying the right orbital cavity. She presented also with inflammatory sinusopathy involving the right maxillary, ethmoid and frontal sinuses. After 14 d of clinical observation and antimicrobial therapy, the patient received a computed tomography scan, which showed growth of the cerebral mass, with a ring of peripheral contrast enhancement and surrounding edema. She promptly underwent neurosurgical treatment and recovered well, except for the sight in her right eye, which remained compromised, as before the operation. This is believed to be the first case of cryptogenic cerebral abscess caused by Raoultella ornithinolityca isolated from the brain, with more than 1-year follow-up.
Core tip: Brain abscess is a focal intracranial infection that evolves in a collection of pus. It could have cryptogenic origin in 10%-35% of cases. I present a 64-year-old woman affected by a frontal brain abscess that was surgically treated, from which Raoultella ornithinolytica (R. ornithinolytica) was isolated. The patient, after > 1 year, is doing well, except for her right eye that had already lost its visual power before surgery. This is believed to be the first case of cryptogenic cerebral abscess caused by R. ornithinolytica.
- Citation: Luongo M. Rare case of cryptogenic brain abscess caused by Raoultella ornithinolityca. World J Clin Cases 2017; 5(7): 299-302
- URL: https://www.wjgnet.com/2307-8960/full/v5/i7/299.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i7.299
Brain abscess is a focal intracranial infection characterized as an area of cerebritis that evolves in a collection of pus surrounded by a vascularized capsule. Organisms can reach the central nervous system by spreading from a contiguous source of infection, hematogenous dissemination, or trauma, but there are cryptogenic brain abscesses in 10%-35% of cases. The frontal lobe is the predominant site of cerebral abscess in patients with paranasal sinusitis. Raoultella ornithinolytica (R. ornithinolytica) is an encapsulated Gram-negative bacterium and member of the Enterobacteriaceae. Human infections caused by Raoultella are rare. I describe a case of cryptogenic cerebral abscess caused by R. ornithinolytica, with good recovery after > 1 year after surgery.
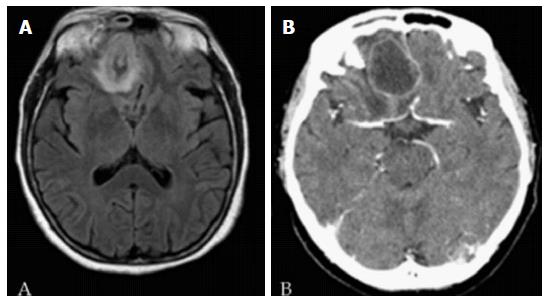
A 64-year-old woman was admitted to our hospital for fever and headache. She was hospitalized in the Infectious Disease Department for observation and study. Chest X-ray and abdominal ultrasound examination were normal. Magnetic resonance imaging (MRI) with gadolinium revealed a right frontobasal brain abscess, compressing the homolateral frontal horn of the lateral ventricle, with a second mass partially occupying the right orbital cavity (Figure 1A). She presented also with inflammatory sinusopathy involving the right frontal, ethmoid and maxillary sinuses. After 14 d of clinical observation and intravenous broad-spectrum antibiotic therapy, nasal culture was performed on day 14 of hospitalization, which showed evidence of low levels of Candida albicans. Ophthalmological consultation revealed visual loss from her right eye, and contrast computed tomography (CT) showed an increase in abscess size, so the patient underwent prompt surgery with right frontobasal craniotomy (Figure 1B). Thanks to neuronavigation and under operative microscopy, the abscessual capsule was opened widely, in order to drain its content, and it was coagulated to avoid damage to nervous structures, given that the cerebral parenchyma in the right orbit appeared to be involved in an inflammatory reaction. Some of the mass content was sent for microbiological examination in Bactec broth and, 8 d after surgery, R. ornithinolytica was isolated by conventional microbiological tests. On the basis of an antibiogram, determined according to the European Committee on Antimicrobial Susceptibility Testing, and after consulting an infectious diseases specialist, the patient started intravenous therapy with metronidazole and ceftriaxone, four times and twice daily, respectively (Table 1). She received a basal CT scan that showed no residual or recurrent brain abscess.
| Drug | Dosage | Administration route | Duration of therapy, d | Frequency of administration, d |
| Ceftriaxone | 2 g | Intravenous | 50 | 2 |
| Amphotericin b | 50 mg | Intravenous | 20 | 1 |
| Amikacin | 500 mg | Intravenous | 12 | 1 |
| Ciprofloxacin | 200 mg | Intravenous | 11 | 2 |
Her general clinical conditions were improved but, on day 30 in hospital (approximately 2 wk after surgery) she developed right-side pneumonia with pleural effusion, caused by Klebsiella pneumoniae, which was treated by intravenous ceftriaxone and ciprofloxacin twice daily, together with amphotericin B and amikacin once daily (Table 1). During the last month she was free from antimicrobial therapy, without infectious problems, but it was necessary to correct persistent hypokalemia, presented by the patient from the first time. The patient was discharged after approximately 3 mo of hospitalization and she is currently well.
R. ornithinolytica is an encapsulated, aerobic, nonmotile, blood-borne Gram-negative bacterium belonging to the Enterobacteriaceae, which is frequently misidentified as Klebsiella spp. It was first described by Sakazaki et al[1] in 1989 and it can be isolated from aquatic environments, insects, fish and brackish water. It can cause fish poisoning because of its capacity to produce histamine and it can cause headache, flushing, abdominal cramps, pruritus, and rarely, bradycardia, bronchospasm and hypotension. Over the years, R. ornithinolytica has emerged as an infrequent cause of human infections, with about 10 cases reported linking the bacterium to bacteremia, sepsis, and soft tissue and other infections, as described by Nakasone et al[2] in their article about a case of community-acquired urinary infection.
An important study on clinical characteristics of R. ornithinolytica bacteremia focused on its unfavorable outcomes, compared to bacteremia caused by other Raoultella spp. The study analyzed 16 patients (11 male and 5 female) over 10 years, with a mean age of 55.7 years; all but one had an underlying malignant condition and seven had infections associated with the biliary tract. They found that the overall mortality of R. ornithinolytica bacteremia could be compared to that of Klebsiella spp., and it was reported to be 20%-25%. In addition, suggested an increased risk of R. ornithinolytica bacteremia in patients affected by underlying malignant conditions extending to the biliary tract[3]. Even though some cases of biliary tract infection, urinary infection and bacteremia have been reported, there is not much information about clinical features and outcomes of R. ornithinolytica. A recent review by Seng and colleagues discusses the largest series reported to date of 86 cases from four French universities over 12 years (with half of cases in 2015), and emphasizes different important characteristics such as a high rate of hospital-acquired infection (49%). Besides comorbidity and risk factors previously reported such as solid tumor, post-urethra trauma, and post invasive procedures, Seng et al[4] found that half of the patients had diabetes or immunodeficiency, and they described infections not previously reported, including pleural effusion, meningitis and cerebral abscess. The cerebral abscess described by Seng et al[4] was secondary to a craniotomy for head trauma and not spontaneous as in the present case[4].
The frontal lobe is the predominant site in patients with brain abscess secondary to paranasal sinusitis, so I thought that the cerebral abscess in my patient was secondary to sinusopathy, but nasal culture only isolated a low number of C. albicans. The patient has diabetes and experienced pleural effusion caused by K. pneumoniae during hospitalization, > 2 wk after surgery, so this case was not related to any condition previously described.
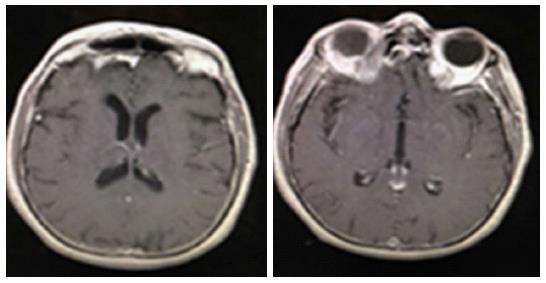
In summary this is the report of a rare case of brain abscess caused by R. ornithinolytica that was successfully treated by intravenous antibiotics and prompt surgical intervention. This is believed to be the first cryptogenic brain abscess caused by R. ornithinolytica, with MRI showing complete surgical removal and no recurrence after > 1 year (Figure 2). It could be important to focus attention on this bacterium in order to understand better and eventually prevent occurrence of this potentially fatal condition.
The author thanks Dr. Luigi Armignacco, Department of Infectious Diseases, San Carlo Hospital, Potenza (Italy), for his help, willingness and expertise in treating the patient. Special thank goes to Noreen Turyn for her support.
A 64-year-old woman with inflammatory sinosupathy and, a few days later, visual loss in the right eye.
Fever and headache with visual disturbance.
Central nervous system inflammatory conditions, cerebral abscess, meningitis, and brain tumor.
Nasal culture and microbiological examination of the surgically removed cerebral mass.
Magnetic resonance imaging with gadolinium revealing the presence of a right frontobasal brain abscess and a second mass partially occupying the right orbital cavity.
Some of the mass content was sent for microbiological examination and Raoultella ornithinolytica was isolated by conventional microbiological tests.
Right frontobasal craniotomy was performed and the abscessual capsule was opened widely and coagulated. On the basis of an antibiogram and after consulting an infectious diseases specialist, the patient started intravenous therapy with antibiotics.
R. ornithinolytica is a Gram-negative bacterium belonging to the family Enterobacteriaceae that is frequently misidentified as Klebsiella spp.. It has potent virulence and is rare in clinical situations but results in a high risk of bacteremia in patients affected by underlying malignant conditions extending to the biliary tract.
R. ornithinolytica brain abscess is a rare condition because, over the years, the bacterium has mainly been responsible for infrequent but important human urinary tract infections.
Brain abscess caused by R. ornithinolytica is a rare condition to be aware of in daily clinical practice in order to understand, prevent and treat it, through a combination of prompt surgical intervention and intravenous antibiotics.
This is a very interesting presentation about a rare etiology for brain abscess. It is a case that reminds us to be aware of this condition in the daily practice. The paper is well structured and written.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Grigoriadis S, Hall WA, Nagashima G, Nedelcuta RM S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Sakazaki R, Tamura K, Kosako Y, Yoshizaki E. Klebsiella ornithinolytica sp. nov., formerly known as ornithine-positive Klebsiella oxytoca. Curr Microbiol. 1989;18:201-206. [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Nakasone ES, Kaneshiro R, Min K, Tokeshi J. Emergence of Raoultella ornithinolytica on O’ahu: a case of community-acquired R. ornithinolytica urinary tract infection. Hawaii J Med Public Health. 2015;74:174-175. [PubMed] [Cited in This Article: ] |
| 3. | Chun S, Yun JW, Huh HJ, Lee NY. Clinical characteristics of Raoultella ornithinolytica bacteremia. Infection. 2015;43:59-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Seng P, Boushab BM, Romain F, Gouriet F, Bruder N, Martin C, Paganelli F, Bernit E, Le Treut YP, Thomas P. Emerging role of Raoultella ornithinolytica in human infections: a series of cases and review of the literature. Int J Infect Dis. 2016;45:65-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 88] [Article Influence: 11.0] [Reference Citation Analysis (0)] |