Published online Mar 16, 2017. doi: 10.12998/wjcc.v5.i3.82
Peer-review started: July 18, 2016
First decision: September 30, 2016
Revised: October 13, 2016
Accepted: December 1, 2016
Article in press: December 3, 2016
Published online: March 16, 2017
There is arguably no less understood or more intriguing problem in hypertension that the “white coat” condition, the standard concept of which is significantly blood pressure reading obtained by medical personnel of authoritative standing than that obtained by more junior and less authoritative personnel and by the patients themselves. Using hospital-initiated ambulatory blood pressure monitoring, the while effect manifests as initial and ending pressure elevations, and, in treated patients, a low daytime profile. The effect is essentially systolic. Pure diastolic white coat hypertension appears to be exceedingly rare. On the basis of the studies, we believe that the white coat phenomenon is a common, periodic, neuro-endocrine reflex conditioned by anticipation of having the blood pressure taken and the fear of what this measurement may indicate concerning future illness. It does not change with time, or with prolonged association with the physician, particularly with advancing years, it may be superimposed upon essential hypertension, and in patients receiving hypertensive medication, blunting of the nighttime dip, which occurs in about half the patients, may be a compensatory mechanisms, rather than an indication of cardiovascular risk. Rather than the blunted dip, the morning surge or the widened pulse pressure, cardiovascular risk appears to be related to elevation of the average night time pressure.
Core tip: White coat hypertension is a poorly understood and significantly common ambulatory blood pressure finding. This study defines blood pressure during various periods of the day and night, analyzes nighttime dip and morning surge, provides insight into the triggers of the episode, and discusses the possible neuro-endocrine causes. It is a permanently conditioned reflex from anticipation and fear that blood pressure measurement may indicate future illness. Recognition of this condition reduces the patient’s worry, relieves them both of a lifetime of unnecessary medication and the side effects of the otherwise ever-increasing dosages, and diminishes the frustration of the attending physician.
- Citation: Bloomfield DA, Park A. Decoding white coat hypertension. World J Clin Cases 2017; 5(3): 82-92
- URL: https://www.wjgnet.com/2307-8960/full/v5/i3/82.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i3.82
There is arguably no less understood or more intriguing problem in hypertension than the “white coat” condition, the standard concept of which is a significantly higher blood pressure reading obtained by medical personnel of authoritative standing than that obtained by more junior and less authoritative personnel and by the patients themselves.
The whole subject is infused with uncertainties and contradictions beginning with the lack of a clear enunciation of the definition upon which the diagnosis rests. This presently depends on a strict definition, recognized by the international cardiological community narrowly as “an office pressure of greater than 140/90 mmHg with a home or ambulatory measurement of less than 135/85 mmHg”, although some authorities recognize wider limits[1-5]. The measurements are based largely on recognition of the Korotkof sounds, a technique unchanged for over a century and rarely measured over a period greater than 10 s. Moreover, the recorded pressure is subject to diurnal variation, activity, rest, emotional state and current medications as well as individual measurement technique, size of cuff, personal auditory acuity and environmental noise levels. Such variety exists in the methods of defining white coat hypertension (WCH)[2,5-8] that the incidence is quoted as low as 10% of the hypertensive population and as high as 40%[9-12].
Almost all adults have a higher systolic blood pressure when taken in a doctor’s office than when taken by ambulatory blood pressure monitoring (ABPM) or by the patients themselves[3]. It has been recognized for two decades that averaged multiple office readings are as much as 10/5 mmHg higher than ABP measurements. Some of these pressures will reduce to normal values with repeated office measurements following rest. Generally, the difference is so small that it lies within the normal daily variation, does not influence the diagnosis in regard to the blood pressure or require a change in management[3].
It is only when the pressure difference is significant and the ABPM configuration is characteristic, that a diagnosis of WCH is warranted. The degree of pressure elevation in susceptible patients is also physician dependent, some physicians causing a higher white coat effect than others.
To add further confusion to the concept, a recent recommendation of the British Heart Society suggested that patients originally thought to have elevated pressures but were found to be normotensive on ambulatory monitoring be classified as “white coat hypertensives” while true hypertensives with further elevation in the presence of the doctor be considered to show the “white coat effect”. A more understandable distinction would be to designate the elevation of pressure as the “white coat effect” and the person manifesting this effect as a “white coat hypertensive”.
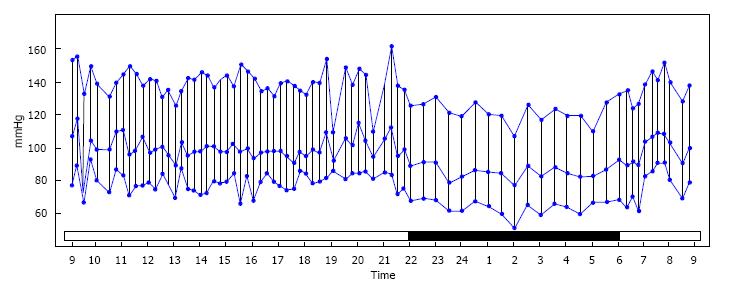
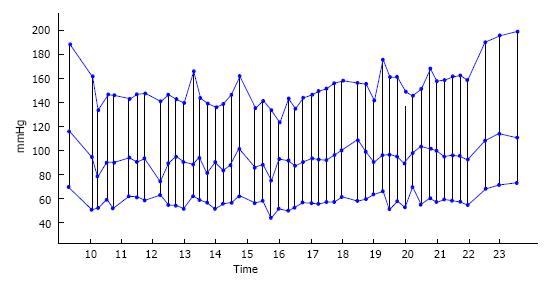
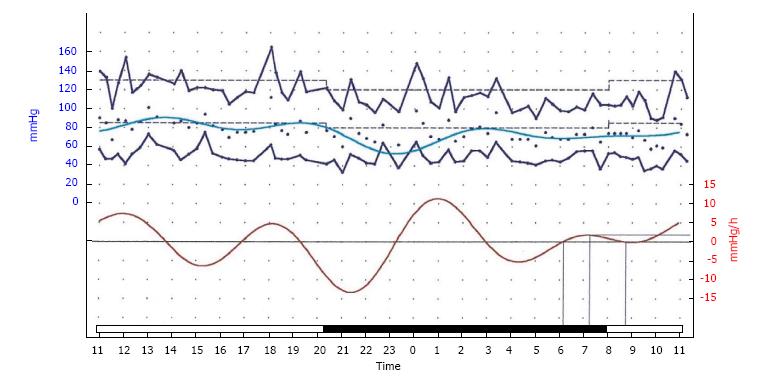
A representative graphic printout of a typically normal 24 h ABPM recording is shown in Figure 1 and the advent of this diagnostic tool has drastically altered the appreciation and understanding of hypertension as a whole and WCH in particular. The use of ABPM has demonstrated that the generally accepted definition of WCH is far too narrow and superficial and does not recognize the complexities revealed by analysis of this technique in susceptible persons. The present review examines the data from decades of ambulatory recording, providing a more comprehensive description of the four characteristic periods in the 24 h recordings, exploring the triggers of the white coat episode, considering the complex implications of the night-time pressure dip and postulating the continuing benign nature of the white coat experience.
Greater understanding of clinical hypertension will only evolve from widespread utilization of 24 h blood pressure monitoring, which is not yet current practice in the United States. It is as important to clinical hypertension as the 24 h Holter has become to clinical arrhythmia and it is indispensable for the understanding of WCH.
The recognition of the inherent inaccuracy of the definition in both clinical practice and hypertension research necessitated the search for other clinical and laboratory measures to describe WCH. A “slow breathing test” causing a fall in pressure after one minute[13], was supposed to indicate WCH. A rise in pressure determined by an unknown and un-introduced physician (the White Coat Test) or the response to public speaking to an audience of strangers[14], were to also confirm the white coat diagnosis. None of these tests have become standards.
In the clinical setting, repeated office pressures in the severe hypertensive range for many years without the evidence of left ventricular hypertrophy, retinal arterial changes or albuminuria, strongly suggests that the recorded pressure is not sustained. Furthermore, office measurements of systolic pressure are known to quickly settle to reduced values on repeated estimation[4] while white coat systolic pressures tend to vary up-and-down by large amounts on repeated measurements.
The vast proportion of patients referred for ABPM have been unsuccessfully treated for office-perceived hypertension and present while taking usually large amounts of medication. A further clue that the elevated pressure may be due to the white coat effect is the observation that, despite increasing medication, generally little change is elicited in the office in the systolic and diastolic pressures. In true recalcitrant hypertension, by comparison, the medication usually affects some lowering of pressure although not to an acceptable level. The majority of patients in our study were taking between one and four hypertensive medications at the time of their ABP measurement.
The ambulatory recordings can be analyzed to identify almost 30 specific measurements and provide a profile of the white coat effect that greatly expands the understanding of the conditions that define it.
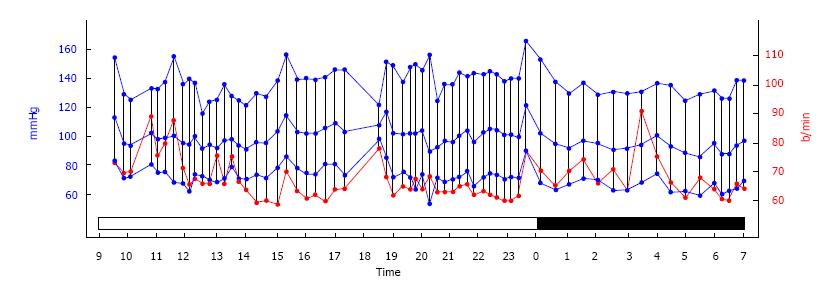
The figures used to illustrate this review were obtained using the Spacelabs equipment (Del Mar-Pressurometer P6 and more recently Sentinal). The studies begin in the morning with the recorder attached in the EKG department of the community hospital. Pressures are recorded continually through the day, through sleep and in the following morning up until the time that the recorder is removed again in the same hospital department. The data is analyzed using the Spacelabs reporting software.
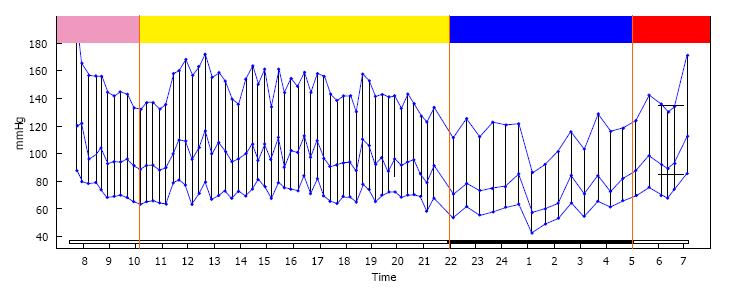
The 24 h blood pressure recordings can be considered in a number of segments: The initial recordings taken at the time of attachment of the recording device and extending for three or four hours, a second segment encompassing the remaining morning hours and through the afternoon and evening until bedtime, a third segment during sleep and a final segment, upon awakening and until the recorder is removed. Each segment has a unique pattern defining its white coat character (Figure 2).
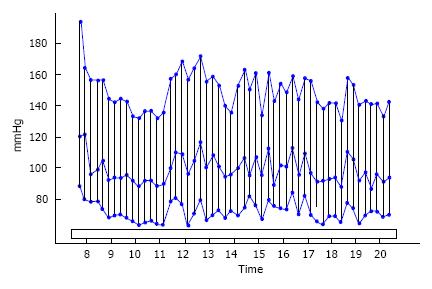
The hospital department and the application of the recorder in that setting provide the environment to trigger the white coat effect. Precipitated by the attachment of the ABP monitor, the pressure is usually high and is recorded at or near the office pressure. The hook-up is not performed by a white-coated physician but by a casually dressed technician so the stimulus appears to be related to the hospital environment and the patient’s concern about what the test results might portend. These conditions and its effect have been reported elsewhere[15,16], identifying this response to be universal and not specific for this particular hospital.
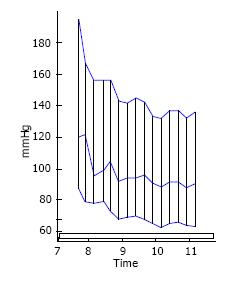
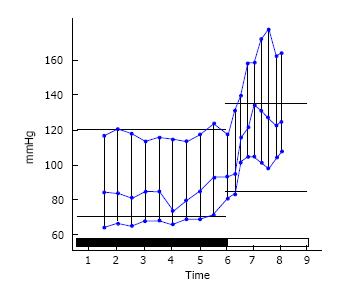
In the first minutes of recording, the systolic and diastolic pressures usually reach the highest levels in the entire 24 h. The next 30 min shows the steepest fall of pressure but it rarely falls to the eventual daytime values. This pattern, illustrated in Figure 3, has been recognized and used by others as a supplemental factor in the diagnosis[17]. During the next 2 to 3 h, the pressure falls more slowly to usually the lowest daytime value[18].
This bimodal pattern suggests that either the sympathetic stimulus responsible for the initial pressure elevation does not quickly dissipate or that it is accompanied by an endocrine stimulus with a slower rate of decline. This neuro-endocrine mechanism may not be only specific for blood pressure as a case has been reported of a white coat hypertensive who was also a white coat hyperglycemic as his laboratory-obtained blood sugar was always elevated while his home level and his Hemoglobin A1C were always normal[19].
In this initial segment, the pulse pressure tends to be wider as the systolic pressure is elevated disproportionately to the diastolic. This observation has also been used as an indicator of the white coat effect[20-22]. Using the standard office/home pressure difference to identify the white coat effect, a positive correlation was found with pulse pressures of 60 mmHg or greater.
This segment is characterized by a plateau which is sustained with only minor variations. As the vast majority of the patients were receiving multiple hypertensive medications, this level may, in fact, be below normal. Three variations have been seen in this segment.
The first variation occurs when the patient exercises. The response is normal for exercise with elevation of the systolic and less elevation of the diastolic pressure. Following the exercise, the pressure falls back rapidly (unlike the dissipation of the white coat elevation) to the previous plateau level (Figure 4). This pattern probably mimics that of recovery after a stress test, when the heart rate and the blood pressure normally fall to the resting level within 12 min. However, the recording frequency of the ABPM is usually set at no shorter than 30 min in the daytime so this information is often not recorded. A similar rise and fall of the pressure can be seen with episodes of anxiety, excitement and anger but neither these nor the exercise elevations reach the magnitude of the white coat episodes.
A second variation occurs when the patient experiences another incident which provokes the white coat response. An expanded discussion of the “triggers” of the white coat episodes will be presented and discussed later.
A third variation occurs when the patient actually has essential hypertension complicated by the white coat effect. With a relatively high occurrence of these two conditions in the older adult population, the coincidence is not unusual. In this instance, pressure rises through the afternoon and evening in the normal diurnal manner and the pressures eventually reach abnormally high levels (Figure 5). In the past, WCH has been described as part of a continuous spectrum, beginning with normal blood pressure, ending with true essential hypertension with white coat intermediate between the two[23-25]. This was part of the widely held concept that WCH was not a benign disorder, retaining the capacity to morph into true, sustained hypertension[7,26-32]. Interestingly, the vast majority of papers supporting this concept have used the narrow and possibly contentious definition (> 140 mmHg office with < 135 mmHg home) to diagnose WCH.
Our present view is that as both benign white coat and pathological essential hypertension are common conditions, the occasion frequently arises when the two will exist together and, as time passes, the true pressure elevation of older age eventually dominates but does not obscure the white coat effect (Figure 6). This concept is supported by many authors[33-39].
The circadian fall in blood pressure during sleep has been fully examined only since the advent of ABP monitoring and its occurrence in WCH has not been generally elucidated.
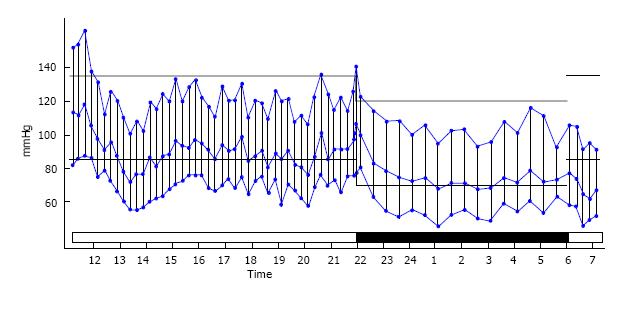
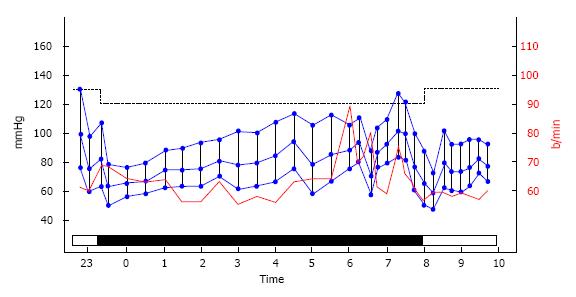
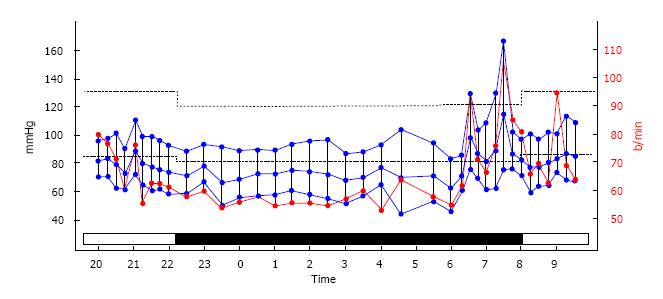
This physiological nighttime dip in pressure occurs in approximately half of the hypertensive adult population[40]. It occurs in approximately the same proportion in treated white coat hypertensives. When this happens, the pressure may be significantly lowered by the medication but this tends to be without symptoms or complications (Figure 7). The understanding of the “night-time dip” is complex and its significance is controversial. Although no definition of its calculation is standardized, the generally utilized method is to subtract the average night-time systolic pressure from the average daytime systolic pressure and express that value as a percentage of the daytime figure. It is generally agreed that it is normal for the mean systolic pressure to fall to a level 10%-20% lower than the mean daytime systolic pressure. Those whose pressure falls less than 10% are known as “non-dippers” or as having a “blunted” dip. Essential hypertensive patients are understood to lose the night time dip.
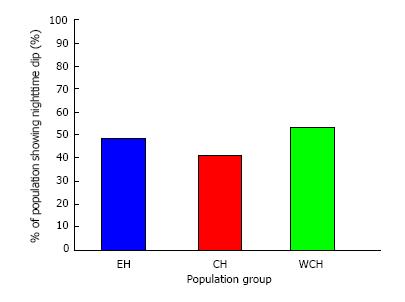
The concept of “blunted” dipping of the pressure (Figure 8) has been linked to the increased risk of cardiovascular disorders[41-45] but these studies have almost always been conducted in patients not on hypertensive medication[46]. Half of the white coat patients in this series had blunting or absence of the nighttime dip, but because they had neither sustained hypertension, left ventricular hypertrophy, albuminuria or optic fundal arterial changes for many years, it was difficult to believe that they were at enhanced cardiovascular risk. To further elucidate this issue, medicated but uncontrolled essential hypertensives, medicated controlled hypertensives and medicated white coat hypertensives were compared in regard to the nighttime dip. While the three groups were significantly different in multiple modalities of blood pressure, they were not significantly different in regards to their percentage of nighttime dippers (Figure 9)[46]. It was concluded that, in contrast to the reported findings in un-medicated white coat hypertensives, the nighttime dip could not be used as a predictor of cardiovascular risk in medicated white coat patients although this cannot be substantiated due to the lack of follow up information.
One possible explanation of benign non-dipping in medicated patients is that the body’s auto-regulatory systems may not permit the night-time pressure to “dip” further when it is already reduced to very low levels with hypertensive drugs. In both treated and untreated hypertensives, blunting was associated with advanced age, obesity, diabetes mellitus and overt cardiovascular or renal disease, suggesting that blunting may be merely a marker of high cardiovascular risk rather than a cause[40]. However, if the actual average night-time systolic pressure is considered rather than the “dip”, a strong correlation with cardiovascular risk has been shown[47].
Pressures may also rise during the night (Figure 10). This can be caused by episodes of obstructive sleep apnea and superimposed essential hypertension. Dreams and particularly nightmares are also implicated (Figure 11). Waking to empty the bladder does not usually cause a significant elevation. None of these pressure elevations mimic the white coat episode.
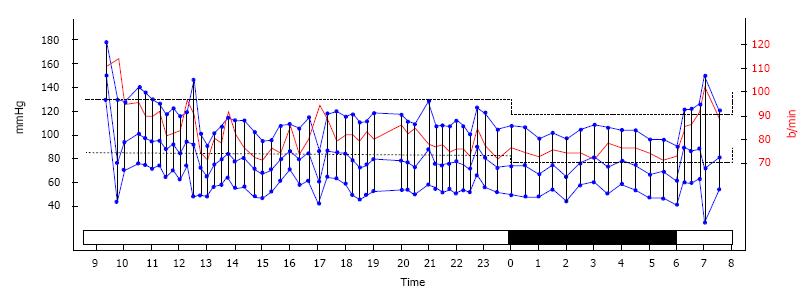
This segment, representing the time of awakening and the subsequent couple of hours, is characterized by a normal circadian rise in pressure continuing until the recording device is removed. In our series, this provoked another white coat episode. In most cases the pressure does not reach the same peak as was recorded when the monitor was initially attached at the beginning of the study and, on rare occasions, it is not seen at all. When exaggerated, this pressure rise is designated “the morning surge” (Figure 12) and it has been considered the cause of the increased incidence of acute myocardial infarction in the morning hours. In treated white coaters with pre-awakening depressed pressure, this rise may be further exaggerated. However in our series, there were frequent instances at other times during the day when the blood pressure “surge” was greater than in the morning (Figure 13), but no myocardial infarction was experienced in the whole series while the ABPM was recording.
In non-dippers, the morning rise may be diminished. Clearly the “dip” and the “surge” are dependently linked and while they share the time course of increased cardiovascular episodes, the cause of these events seems to have been shown to be due principally to the average nighttime systolic pressure[47].
Widening of the pulse pressure has been recognized as a risk factor in cardiovascular disease, particularly as it is usually associated with systolic hypertension, aortic regurgitation or thyrotoxicosis, risk factors in themselves. The white coat effect raises the systolic pressure either exclusively or by a far greater magnitude than the diastolic and widening of the pulse pressure occurs with every episode. As such, it has been recognized as a marker of this condition[20-22]. The relationship or interdependence of the systolic and diastolic pressures in WCH, as measured by the correlation coefficient, has not been shown to be unique or different from that of regular essential hypertension. No cases of acute myocardial infarction occurred while the patients were being monitored and no symptoms of angina were reported during the white coat periods.
White coat elevation in blood pressure is essentially systolic and another feature of the white coat effect is the apparent rarity of pure diastolic WCH which we can define as a significant diastolic difference between office and home or ABPM pressure with a sustained normal systolic pressure. There is a modest related increase in the diastolic pressure during a white coat episode, such as happens with an exercise stress test, but no case of pure and isolated diastolic WCH with sustained normal systolic pressure has been previously reported. Only two such cases have been observed in this series. One example is shown in Figure 14. The other patient had office diastolics 25-30 mmHg higher than on the ABP monitor. This may result from diastolic pressure being related to a different proportion of neuro and endocrine control of the peripheral arteriolar constriction than systolic WCH. However, both patients, post menopausal women, had prior strokes, one due to undiagnosed atrial fibrillation, the other with temporal arteritis and both fully recovered at the time of white coat diagnosis. The relationship of the neurological and cardiac conditions is unknown. A relationship with diastolic WCH has been demonstrated with polymorphisms of angiotensinogen, angiotensin-converting enzyme and protein G[45].
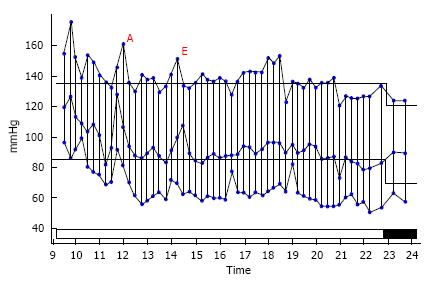
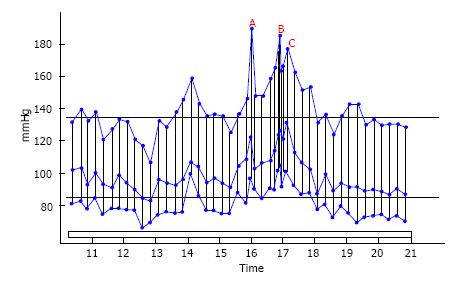
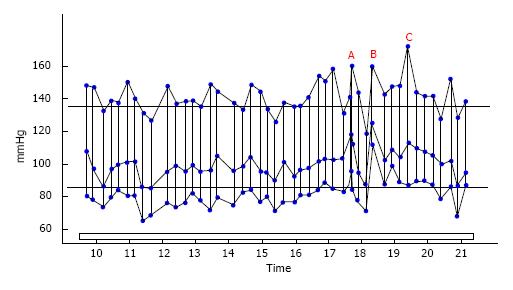
Apart from Mancia’s study[48] observing the appearance of the physician at the patient’s bedside, no detailed examination of the process that triggers the white coat event has been reported. Possible factors include anxiety linked to anticipation of having the blood pressure measured, arriving at the doctor’s office, entering into the examining room, undergoing the preceding physical examination, or the actual recording of the blood pressure. In a study to clarify this issue, known white coat hypertensives were recruited and underwent the aforementioned sequence of events while wearing an ambulatory blood pressure recording device[49].
Attachment of the monitor in the hospital setting and each of the afore-mentioned stages of a doctor’s visit provoked a white coat episode. Anticipation of the visit evoked some blood pressure elevation but arrival at the doctor’s office produced a full-blown white coat episode, indicated by the letter A in the subsequent figures. While waiting for the doctor, this peak tended to resolve to some extent. This time course has been previously reported and has been suggested as a characteristic of the episodes. Admission to the consulting room (letter B in the figures) caused another pressure rise and manually taking the blood pressure by cuff and mercury manometer produced the highest peak (letter C). Placement of the cuff but not inflating it to record a manual pressure produced the same blood pressure response as if it had actually been taken, reinforcing the “anticipation” concept. Recorded episodes of exercise, aggravation (Figure 15) and anxiety (Figure 16) produced less pressure elevations than the white coat episodes.
Much has been written concerning the mechanism of WCH in terms of pathophysiology, personality, interpersonal interactions and the influence of authority. Anxiety elevates blood pressure but does not appear to be the trigger for the white coat episodes[50] as white coat patients have been subjected to anxiety testing and have not been shown to be different to non-white coat persons[51,52]. Mental stress has been considered as a trigger for the white coat episode[53], but this could not be confirmed by other researchers[54]. Reactivity to public peaking has been advanced as a cause[55] but this clearly could not be a trigger for real life office pressure measurement. Anticipation not only of actually taking the blood pressure but the interpretation of the result by the doctor and its imagined significance on the health status seems to be the main stimulus of the white coat effect. Anticipation ranks more highly than anxiety.
Jhalani et al[56] considered the mechanism to be due to a conditioned reflex that, once established persisted for visit after doctor’s visit, year upon year. Even when the fear of an adverse finding was eliminated by repeated examinations over the years, the white coat response persisted[56]. This process has been described with severe, prolonged nausea, provoking anticipation about further cyclical vomiting attacks, facilitating conditioning in a self-perpetuating manner.
On the basis of the studies, we believe that the white coat phenomenon is a common, periodic, neuro-endocrine reflex conditioned by anticipation of having the blood pressure taken and the fear of what this measurement may indicate concerning future illness. It does not change with time or with prolonged association with the physician.
Particularly with advancing years, it may be superimposed upon essential hypertension and, in patients receiving hypertensive medication, blunting of the night-time dip, which occurs in about half the patients, may be a compensatory mechanism rather than an indication of cardiovascular risk. Rather than the blunted dip, the morning surge or the widened pulse pressure, cardiovascular risk appears to be related to elevation of the average night time pressure.
On hospital initiated ABPM, the white coat effect manifests as initial and ending pressure elevations and, in treated patients, a low daytime profile. The effect is essentially systolic. Pure diastolic WCH appears to be exceedingly rare.
Recognition of this condition reduces patient’s worry, relieves them both of a lifetime of unnecessary medication and the side effects of the otherwise ever-increasing dosages and diminishes the frustration of the attending physician.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sanchez R, Tan XR S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Verdecchia P, Schillaci G, Boldrini F, Zampi I, Porcellati C. Variability between current definitions of ‘normal’ ambulatory blood pressure. Implications in the assessment of white coat hypertension. Hypertension. 1992;20:555-562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 125] [Cited by in F6Publishing: 116] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Verdecchia P, Staessen JA, White WB, Imai Y, O’Brien ET. Properly defining white coat hypertension. Eur Heart J. 2002;23:106-109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Rasmussen SL, Torp-Pedersen C, Borch-Johnsen K, Ibsen H. Normal values for ambulatory blood pressure and differences between casual blood pressure and ambulatory blood pressure: results from a Danish population survey. J Hypertens. 1998;16:1415-1424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 78] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Khan TV, Khan SS, Akhondi A, Khan TW. White coat hypertension: relevance to clinical and emergency medical services personnel. MedGenMed. 2007;9:52. [PubMed] [Cited in This Article: ] |
| 5. | Agarwal R, Sinha AD, Light RP. Toward a definition of masked hypertension and white-coat hypertension among hemodialysis patients. Clin J Am Soc Nephrol. 2011;6:2003-2008. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Kario K, Pickering TG. Survey of white coat hypertension. Definition differs from others. BMJ. 1999;318:535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Muscholl MW, Hense HW, Bröckel U, Döring A, Riegger GA, Schunkert H. Changes in left ventricular structure and function in patients with white coat hypertension: cross sectional survey. BMJ. 1998;317:565-570. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Porcellati C. White-coat hypertension. Lancet. 1996;348:1444-1445; author reply. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 61] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Hwang ES, Choi KJ, Kang DH, Nam GB, Jang JS, Jeong YH, Lee CH, Lee JY, Park HK, Park CH. Prevalence, predictive factor, and clinical significance of white-coat hypertension and masked hypertension in Korean hypertensive patients. Korean J Intern Med. 2007;22:256-262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988;259:225-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 669] [Cited by in F6Publishing: 666] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 11. | Helvaci MR, Seyhanli M. What a high prevalence of white coat hypertension in society! Intern Med. 2006;45:671-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Martínez MA, García-Puig J, Martín JC, Guallar-Castillón P, Aguirre de Cárcer A, Torre A, Armada E, Nevado A, Madero RS. Frequency and determinants of white coat hypertension in mild to moderate hypertension: a primary care-based study. Monitorización Ambulatoria de la Presión Arterial (MAPA)-Area 5 Working Group. Am J Hypertens. 1999;12:251-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 73] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Thalenberg JM, Póvoa RM, Bombig MT, Sá GA, Atallah AN, Luna Filho B. Slow breathing test increases the suspicion of white-coat hypertension in the office. Arq Bras Cardiol. 2008;91:243-249, 243-249. [PubMed] [Cited in This Article: ] |
| 14. | Saladini F, Benetti E, Malipiero G, Casiglia E, Palatini P. Does home blood pressure allow for a better assessment of the white-coat effect than ambulatory blood pressure? J Hypertens. 2012;30:2118-2124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | O'Brien E, Fitzgerald D. The history of blood pressure measurement. J Hum Hypertens. 1994;8:73-84. [PubMed] [Cited in This Article: ] |
| 16. | Owens P, Atkins N, O’Brien E. Diagnosis of white coat hypertension by ambulatory blood pressure monitoring. Hypertension. 1999;34:267-272. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | van der Wel MC, Buunk IE, van Weel C, Thien TA, Bakx JC. A novel approach to office blood pressure measurement: 30-minute office blood pressure vs daytime ambulatory blood pressure. Ann Fam Med. 2011;9:128-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | O'Brien E, Beevers G, Lip GY. ABC of hypertension. Blood pressure measurement. Part III-automated sphygmomanometry: ambulatory blood pressure measurement. BMJ. 2001;322:1110-1114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Benmoussa JA, Clarke M, Bloomfield D. White Coat Hyperglycemia: The Forgotten Syndrome. J Clin Med Res. 2016;8:567-568. [PubMed] [Cited in This Article: ] |
| 20. | Yoon HJ, Ahn Y, Kim KH, Park JC, Park JB, Park CG, Youn HJ, Choi DJ, Shin JH, Kim DW. Can pulse pressure predict the white-coat effect in treated hypertensive patients? Clin Exp Hypertens. 2012;34:555-560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Hermida RC, Ayala DE, Calvo C, Lopez JE, Fernandez JR, Mojon A, Dominguez MJ, Covelo M. P-31: Pulse pressure differences between normotensive and white coat hypertensive subjects. Am J Hypertens. 2003;16:50A. [Cited in This Article: ] |
| 22. | Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Pede S, Porcellati C. Ambulatory pulse pressure: a potent predictor of total cardiovascular risk in hypertension. Hypertension. 1998;32:983-988. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 260] [Cited by in F6Publishing: 271] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 23. | Morcos H, Bloomfield DA. The illusion of white coat hypertension. J of Heart Disease. 2003;3:14. [Cited in This Article: ] |
| 24. | Ihm SH, Youn HJ, Park CS, Kim HY, Chang K, Seung KB, Kim JH, Choi KB. Target organ status in white-coat hypertensives: usefulness of serum procollagen type I propeptide in the respect of left ventricular diastolic dysfunction. Circ J. 2009;73:100-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Spence JD. White-coat hypertension is hypertension. Hypertension. 2008;51:1272. [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Muldoon MF, Nazzaro P, Sutton-Tyrrell K, Manuck SB. White-coat hypertension and carotid artery atherosclerosis: a matching study. Arch Intern Med. 2000;160:1507-1512. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 62] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Mallion JM, Baguet JP, Siché JP, Tremel F, De Gaudemaris R. Clinical value of ambulatory blood pressure monitoring. J Hypertens. 1999;17:585-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Glen SK, Elliott HL, Curzio JL, Lees KR, Reid JL. White-coat hypertension as a cause of cardiovascular dysfunction. Lancet. 1996;348:654-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 29. | Gustavsen PH, Høegholm A, Bang LE, Kristensen KS. White coat hypertension is a cardiovascular risk factor: a 10-year follow-up study. J Hum Hypertens. 2003;17:811-817. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 142] [Cited by in F6Publishing: 145] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 30. | Chang NC, Lai ZY, Chan P, Wang TC. Left ventricular filling profiles in young white-coat hypertensive patients without hypertrophy. Hypertension. 1997;30:746-752. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Puato M, Palatini P, Zanardo M, Dorigatti F, Tirrito C, Rattazzi M, Pauletto P. Increase in carotid intima-media thickness in grade I hypertensive subjects: white-coat versus sustained hypertension. Hypertension. 2008;51:1300-1305. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 32. | Kario K, Shimada K, Schwartz JE, Matsuo T, Hoshide S, Pickering TG. Silent and clinically overt stroke in older Japanese subjects with white-coat and sustained hypertension. J Am Coll Cardiol. 2001;38:238-245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 168] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Khattar RS, Senior R, Lahiri A. Cardiovascular outcome in white-coat versus sustained mild hypertension: a 10-year follow-up study. Circulation. 1998;98:1892-1897. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 198] [Cited by in F6Publishing: 200] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 34. | Himmelmann A, Hansson L, Hedner T. Blood pressure measurement: a century of achievements and improvements in the year 2002. Blood Press. 2002;11:325-327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Iqbal P, Stevenson L. Cardiovascular outcomes in patients with normal and abnormal 24-hour ambulatory blood pressure monitoring. Int J Hypertens. 2010;2011:786912. [PubMed] [Cited in This Article: ] |
| 36. | Pickering TG. White coat hypertension: time for action. Circulation. 1998;98:1834-1836. [PubMed] [DOI] [Cited in This Article: ] |
| 37. | Marchi-Alves LM, Carnio EC. Is There Any Correlation between Insulin Resistance and Nitrate Plasma Concentration in White Coat Hypertensive Patients? Cardiol Res Pract. 2009;2009:376735. [PubMed] [Cited in This Article: ] |
| 38. | Dawes MG, Bartlett G, Coats AJ, Juszczak E. Comparing the effects of white coat hypertension and sustained hypertension on mortality in a UK primary care setting. Ann Fam Med. 2008;6:390-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Ng CM, Yiu SF, Choi KL, Choi CH, Ng YW, Tiu SC. Prevalence and significance of white-coat hypertension and masked hypertension in type 2 diabetics. Hong Kong Med J. 2008;14:437-443. [PubMed] [Cited in This Article: ] |
| 40. | de la Sierra A, Redon J, Banegas JR, Segura J, Parati G, Gorostidi M, de la Cruz JJ, Sobrino J, Llisterri JL, Alonso J. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 254] [Cited by in F6Publishing: 260] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 41. | Koroboki E, Manios E, Psaltopoulou T, Vemmos K, Michas F, Alexaki E, Zakopoulos N. Circadian variation of blood pressure and heart rate in normotensives, white-coat, masked, treated and untreated hypertensives. Hellenic J Cardiol. 2010;53:432-438. [PubMed] [Cited in This Article: ] |
| 42. | O'Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2:397. [PubMed] [Cited in This Article: ] |
| 43. | Mousa T, el-Sayed MA, Motawea AK, Salama MA, Elhendy A. Association of blunted nighttime blood pressure dipping with coronary artery stenosis in men. Am J Hypertens. 2004;17:977-980. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 44. | Bellelli G, Frisoni GB, Lucchi E, Guerini F, Geroldi C, Magnifico F, Bianchetti A, Trabucchi M. Blunted reduction in night-time blood pressure is associated with cognitive deterioration in subjects with long-standing hypertension. Blood Press Monit. 2004;9:71-76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 45. | Winnicki M, Somers VK, Hoffmann M, Accurso V, D’Este D, Zanatta G, Bartolazzi A, Pawlowski R, Semplicini A, Siffert W. P-122: Is white-coat effect a uniform phenomenon? Am J Hypertens. 2003;16:82A-83A. [Cited in This Article: ] |
| 46. | Yogendran L, Abdelqader A, Mohamed M, Schuler T, Bloomfield D. Nighttime pressure dip in white coat hypertension. J Heart Diesease. 2014;11:72. [Cited in This Article: ] |
| 47. | Hermida RC, Moya A, Crespo JJ, Otero A, Dominguez M, Rios MT, Castineira C, Mojon A, Fernandez JR, Ayala DE. Asleep blood pressure is an independent predictor of cardiovascular events: the Hygia project. J Heart Disease. 2014;11:36. [Cited in This Article: ] |
| 48. | Mancia G, Bertinieri G, Grassi G, Parati G, Pomidossi G, Ferrari A, Gregorini L, Zanchetti A. Effects of blood-pressure measurement by the doctor on patient’s blood pressure and heart rate. Lancet. 1983;2:695-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 511] [Cited by in F6Publishing: 453] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 49. | Bloomfield DA. Decoding white coat hypertension. J Heart Dis. 2014;11:38. [Cited in This Article: ] |
| 50. | Giorgini P, Striuli R, Petrarca M, Petrazzi L, Pasqualetti P, Properzi G, Desideri G, Omboni S, Parati G, Ferri C. Long-term blood pressure changes induced by the 2009 L’Aquila earthquake: assessment by 24 h ambulatory monitoring. Hypertens Res. 2013;36:795-798. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Nakao M, Shimosawa T, Nomura S, Kuboki T, Fujita T, Murata K. Mental arithmetic is a useful diagnostic evaluation in white coat hypertension. Am J Hypertens. 1998;11:41-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Siegel WC, Blumenthal JA, Divine GW. Physiological, psychological, and behavioral factors and white coat hypertension. Hypertension. 1990;16:140-146. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 73] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Lantelme P, Milon H, Gharib C, Gayet C, Fortrat JO. White coat effect and reactivity to stress: cardiovascular and autonomic nervous system responses. Hypertension. 1998;31:1021-1029. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 72] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 54. | Parati G, Pomidossi G, Casadei R, Ravogli A, Groppelli A, Cesana B, Mancia G. Comparison of the cardiovascular effects of different laboratory stressors and their relationship with blood pressure variability. J Hypertens. 1988;6:481-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 80] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 55. | Palatini P, Palomba D, Bertolo O, Minghetti R, Longo D, Sarlo M, Pessina AC. The white-coat effect is unrelated to the difference between clinic and daytime blood pressure and is associated with greater reactivity to public speaking. J Hypertens. 2003;21:545-553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 56. | Jhalani J, Goyal T, Clemow L, Schwartz JE, Pickering TG, Gerin W. Anxiety and outcome expectations predict the white-coat effect. Blood Press Monit. 2005;10:317-319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |