Published online Mar 16, 2017. doi: 10.12998/wjcc.v5.i3.124
Peer-review started: June 29, 2016
First decision: August 5, 2016
Revised: November 2, 2016
Accepted: November 21, 2016
Article in press: November 23, 2016
Published online: March 16, 2017
Processing time: 258 Days and 14.2 Hours
We are reporting the case of a 32-year-old female who had suffered from fecal incontinence (FI). She was born with an imperforate anus and a recto-vaginal fistula; she underwent repair at 6 mo of age. At 29 years of age, she was still fecally incontinent despite extensive pelvic floor reeducation. A magnetic resonance imaging and an anal electromyography were performed. Because her symptoms were considered to be probably due to extra-sphincteric implantation of the neo-anus, a redo was performed of the recto-neo-anal intra-sphincteric anastomosis. A neurostimulator device was subsequently implanted for persistent incontinence. Solid and liquid FI resolved, and her quality of life improved markedly. Combining surgery to correct the position of the neo-anus within the anal sphincter complex and neurostimulation could thus become a new approach in cases of refractory FI for patients with imperforate anus as a newborn. Follow-up into adulthood after pediatric imperforate anus surgery should be recommended for adult patients with persistent FI.
Core tip: Fecal incontinence is frequent among young adults who have suffered from an imperforate anus. This condition needs to be better understood by adult surgeons, and evaluation of the repair is necessary. This case report describes exams done to confirm the abnormal position of the anus in relation to the sphincter complex and what was done to improve the condition of the patient. Surgery and neurostimulation were complementary and dramatically improved the quality of life of this patient.
- Citation: Bougie A, McFadden N, Mayer S, Lebel M, Devroede G. Neurostimulation for fecal incontinence after correction of repair of imperforate anus. World J Clin Cases 2017; 5(3): 124-127
- URL: https://www.wjgnet.com/2307-8960/full/v5/i3/124.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i3.124
Surgeries in the first years of life for imperforate anus can lead to lifelong problems with fecal incontinence (FI) with a great impact on quality of life[1], largely due to the neo-anus in relation to the anal sphincter position and integrity. Despite successful surgery, results for fecal continence and quality of life can be disappointing.
Sacral neurostimulation (SNS) is a new modality to help restore fecal continence when patients are refractory to standard treatment[2]. The feasibility of SNS has been explored for adult patients with anorectal malformations[3]. To continue to advance the indications for SNS within the context of FI, we describe how a patient’s continence was fully restored with SNS, subsequent to a second intra-sphincteric bowel re-transposition, 30 years after the first attempt.
A 24-year-old woman presented herself to the perineology unit for a history of FI, soiling, uncontrolled flatulence and urgent defecation worsening for 2 years and recent symptoms of dyschezia. She complained of constipation, the longest period without stools being 3 d. For at least 1 year, bowel emptying of small stools was always incomplete.
She was born by vaginal delivery as a full-term baby with an imperforate anus and a recto-vaginal fistula. She was treated with dilatations until definitive surgery. She was brought to surgery at the age of 6 mo and anal transposition with repair of the fistula was performed. She was brought back to surgery 2 mo later for a recurrence of the fistula, and an anoplasty with repair of the fistula was performed. After the second surgery, the fistulous tract remained patent for days and eventually closed spontaneously without diversion.
Initial manometry showed that the resting pressure of the anal canal was normal: In cmH2O, rectal pressure was 12; upper anal canal (UAC) pressure was 67; and lower anal canal (LAC) pressure was 51. Voluntary contractions were very weak (only 21 in the UAC, and 13 in the LAC) and of short duration. There was also a decrease in the amplitude of the recto-anal inhibitory reflex (RAIR). Its presence indicated, in retrospect, that the initial congenital lesion was probably a low rather than a high lesion[4]. The recto-anal contractile reflex was absent up to 50 mL of rectal distension by inflating a rectal balloon. She also had a micro-rectum: The maximum tolerable volume was only 90 mL (normal adult values are between 140 and 320 mL).
Pelvic magnetic resonance imaging was performed and showed a normal internal sphincter but a narrow external sphincter and puborectalis on the left side only. There was also a suspicion of a fistulous tract to the vagina (without any clinically evident symptoms). An anal echo-endoscopy was performed, which showed a distorted anus with a narrow recto-vaginal space with the same observations for the external sphincter and a possible fistulous tract. Despite extensive pelvic floor reeducation, the symptoms remained and her quality of life was poor for the following 5 years.
She was referred to surgery for an evaluation for SNS. She was wearing daily protective pads and her Jorge-Wexner score for FI was 15/20[5]. A rectal examination showed that the anal cutaneo-sphincteric reflex was absent, anal tone was poor, and a superficial contraction posterior to the surgical neo-anus was elicited by voluntary anal contraction.
Percutaneous nerve stimulation (PNS) was performed for 1 wk (model 3057, Medtronic). The term PNS is used by analogy to SNS with a permanent InterStim device but with a temporary electrode for Percutaneous Nerve Evaluation (PNE) that can last, with care, for up to three weeks. Unfortunately, successful results were not achieved. After left stimulation, her Jorge-Wexner score remained at 15/20. She had no liquid stools, wore a pad daily (which was constantly dirty) and leaked solid stools almost daily. Similar results were obtained with PNS on the right. Anal electromyography (EMG) showed no response on the right side, where the external sphincter should be located, poor activity on the left and anterior sides, and a better response on the posterior part. There were polyphasic motor units potentials. The neurologist performed the EMG twice, before and after the PNS; he made the additional and previously unreported remark that, anteriorly, he only found scar tissue and very few muscle fibers, in contrast to posterior to the anus. The pudendal nerve latency (PNTML) was normal (1.8 ms) on both sides, as well as the sacral arc at 33 ms.
Because her symptoms were considered to be probably due to extra-sphincteric implantation of the neo-anus, she was brought back to surgery at the age of 30. A dissection of her neo-anus was carried out proximally for 10 cm passing along the posterior vaginal wall. Resection of the neo-anus, which had visibly been implanted anterior to the sphincter, was completed until normal rectal mucosa was found. Intra-operative neuro-stimulation was used to implant the recto-neo-anal intra-sphincteric anastomosis. A loop colostomy was performed to protect the repair. Post-operative manometry showed a normal, unchanged (12, 59 and 60 cmH2O) resting pressure of the anal canal with persistently (even if slightly stronger) weak voluntary contractions, despite a subjective improvement based on a digital examination by the surgeon. EMG showed significantly better results with clear activity of the external sphincter on both sides of the anus. Motor units, however, were still polyphasic and prolonged at 30-40 ms. There was evidence of satellite potentials and conduction block indicating re-innervation. The sacral arc and PNTML remained normal. There was no anismus (recto-sphincteric dyssynergia). The colostomy was later closed. The Jorge-Wexner score for FI was still 11/20 at 4 mo after surgery, and she still complained of losing stools at least once a week and of remaining constipated.
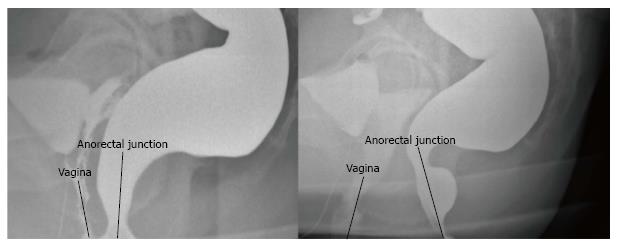
Post-operative defecography showed an impressive difference with her pre-operative defecography (Figure 1). There was a marked widening of the space between the vagina and the anal canal and an improvement of the anorectal angle.
PNS was thus reattempted for 1 wk on the right side without improvement of her score of 11/20, but solid FI stopped. On the left side, her score dropped to 10/20, and stimulation also worked for solid FI. Offered with a choice, she opted for a left permanent SNS.
The first stage of SNS was performed, implanting the tined lead electrode (Medtronic Model 3093-28) on the left side. The neurostimulator device (Medtronic Model 3023, InterStim Neurostimulator) was implanted 3 wk later. One month after definitive surgery her Jorge-Wexner score for FI fell to 2/20; the 2 points were for wearing pads out of fear of soiling. Solid and liquid FI resolved, and her quality of life improved markedly. On her own, she decided to shut off the InterStim at night.
Her remaining complaints were skin tags at the anal margin impeding defecation. Even if she defecated daily, radiopaque markers were not all defecated 1 wk after ingestion of 20 markers. Removal of skin tags partially solved the problem. Slight anismus was corrected by biofeedback. She also scored, understandably with her life history, positive for constipated irritable bowel syndrome (IBS-C) on the basis of the Rome III criteria; this was addressed and solved through long interviews with the treating surgeon (GD). Her Jorge-Wexner score, 2 years after SNS, was 0/20 with only 0.7 V of stimulation. The active electrode was the 0 electrode as the negative pole, and electrode 3 was the positive one. Impedance was 1026 ohms.
Her next visit to check the electronic system was at age 33 and she claimed she had remained fully continent. However, impedance of two of the four electrodes was unacceptably high, above 4000 ohms. She denied any fall or trauma to the buttock, but spontaneously expressed the fact that, encouraged by her full continence, she had become much more physically active. Before, because of her poor quality of life, she was very sedentary. She also complained of some persistent IBS symptoms. Her program was modified. Electrode 2 was selected as the negative pole. The InterStim case became the positive pole. Impedance was 523 ohms; the amplitude of stimulation was slightly higher at 1.65 V. The frequency was set at 21 Hz; on and off stimulation were 25 and 5 s respectively. The current was below 15 µA.
Intensive pelvic floor reeducation is the main treatment for FI in patients who had imperforate anus surgery. Unfortunately, FI frequently persists in adulthood[1]. Adult colorectal surgeons do not see these patients very often, as follow-up may not be recommended by pediatric surgeons.
Despite intensive pelvic floor reeducation, the quality of life of the patient described in this report remained poor until recognition of an extra-sphincteric implantation of her bowel into the neo-anus. The evaluation process took many years as she presented first at the perineology unit for pelvic floor reeducation, which was 5 years before a transfer to surgery.
A first attempt, with neurostimulation only, failed to correct the problem. Her Jorge-Wexner score improved, but she was left with frequent episodes of FI and persistent constipation.
Correction of the surgical error failed to restore fecal continence. Pudendal neuropathy is often present in patients with FI, and this established the basis for successful treatment of this patient. It is our belief that because her external sphincter never worked correctly, resection of the neo-anus and re-implantation of the rectum in the external sphincter did not achieve optimal results, showing the complexity of the problem. As a second PNS attempt showed better results, SNS was performed. Improvement was beyond the surgeon’s expectations and the patient’s quality of life improved dramatically.
Neurostimulator settings need to be personalized to each patient. The first electrode selected may not be optimal for the entire lifespan of the neurostimulator. Dislodgment of the electrode because of physical activity or fibrosis may alter the contact of the electrode with sacral nerves. Resistance and settings are usually periodically verified: The position on the electrode is selected that offers the best sensation at the anus to improve anal function; and the lowest voltage possible is selected to extend the battery life of the neurostimulator.
The patient could turn off her neurostimulator at night without interfering with the functional results. We always suggest that patients do so to increase the battery life of the neurostimulator.
This report shows that not only should the initial surgical treatment be followed up years later but, in addition, the electrical activity of the anus should be evaluated.
Indications of SNS for FI are growing. We demonstrate here a successful case to correct FI in an adult female in the context of chronic problems of congenital origin. Combining surgery to correct the position of the neo-anus in relation to the anal sphincters and SNS could thus become a new approach in cases of refractory FI. Follow-up into adulthood after pediatric imperforate anus surgery is recommended for adult patients with persistent FI; patients who respond to SNS could then be treated accordingly.
A 32-year-old female born with an imperforate anus who suffered from fecal incontinence (FI) despite extensive pelvic floor reeducation.
She complained of FI, soiling, uncontrolled flatulence, urgent defecation and constipation.
Her FI was considered to be due to extra-sphincteric implantation of the neo-anus and to be neurogenic.
An anal electromyography helped for repositioning of the neo-anus and concluded in the neurogenic aspect of the sphincters.
Magnetic resonance imaging and pre-operative defecography demonstrated the erroneous position of the anus. Post-operative defecography showed the widening of the space between the vagina and the anal canal and an improvement of the anorectal angle.
A redo was performed of the recto-neo-anal intra-sphincteric anastomosis. A neurostimulator device was subsequently implanted for persistent incontinence.
Few studies reported use of neurostimulation in case of FI in patients with a history of imperforate anus.
Sacral neurostimulation stimulates the pudendal nerve which is responsible for perineal sensitivity and motor response of the anus.
Follow-up into adulthood after pediatric imperforate anus surgery should be recommended for adult patients with persistent FI.
This is a very interesting case report showing sacral neuromodulation works in a fecal incontinence patient after erroneous repair of imperforate anus. The case report is well written.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Chan KWE, Su X, Tai CF S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Mantoo S, Meurette G, Wyart V, Hardouin J, Cretolle C, Capito C, Sarnacki S, Podevin G, Lehur PA. The impact of anorectal malformations on anorectal function and social integration in adulthood: report from a national database. Colorectal Dis. 2013;15:e330-e335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Wexner SD, Coller JA, Devroede G, Hull T, McCallum R, Chan M, Ayscue JM, Shobeiri AS, Margolin D, England M. Sacral nerve stimulation for fecal incontinence: results of a 120-patient prospective multicenter study. Ann Surg. 2010;251:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 3. | Zurbuchen U, Groene J, Otto SD, Kreis ME, Maerzheuser S. Sacral neuromodulation for fecal incontinence and constipation in adult patients with anorectal malformation--a feasibility study in patients with or without sacral dysgenesis. Int J Colorectal Dis. 2014;29:1297-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Arhan P, Faverdin C, Devroede G, Dubois F, Coupris L, Pellerin D. Manometric assessment of continence after surgery for imperforate anus. J Pediatr Surg. 1976;11:157-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2089] [Cited by in RCA: 1955] [Article Influence: 61.1] [Reference Citation Analysis (1)] |