Published online Feb 16, 2017. doi: 10.12998/wjcc.v5.i2.40
Peer-review started: June 3, 2016
First decision: July 5, 2016
Revised: September 29, 2016
Accepted: October 17, 2016
Article in press: October 18, 2016
Published online: February 16, 2017
Processing time: 259 Days and 15.5 Hours
A 54-year-old black African woman, 22 years human immunodeficiency virus (HIV)-positive, presented with an acute coronary syndrome. She was taking two nucleoside reverse transcriptase inhibitors and two protease inhibitors. Viral load and CD4 count were stable. Angiography revealed a right coronary artery lesion, which was treated with everolimus eluting stent. She also underwent balloon angioplasty to the first diagonal. She re-presented on three different occasions and technically successful coronary intervention was performed. The patient has reported satisfactory compliance with dual anti platelet therapy throughout. She was successfully treated with surgical revascularisation. The patient did not experience any clinical recurrence on follow up. This case demonstrates exceptionally aggressive multifocal and recurrent instent restenosis in a patient treated for HIV infection, raising the possibility of an association with HIV infection or potentially components of retro viral therapy.
Core tip: With an increasing burden of cardiovascular disease in patients with human immunodeficiency virus (HIV), a subgroup of patients may emerge in whom this represents a significant clinical challenge. Better understanding of the responsible mechanisms may allow more tailored pharmacotherapy for susceptible individuals. We report an exceptionally aggressive and recurrent case of coronary stent restenosis in HIV positive patient. Numerous percutaneous interventions were performed but eventually patient was treated successfully with surgical revascularisation.
- Citation: Alkhalil M, Conlon CP, Ashrafian H, Choudhury RP. Aggressive restenosis after percutaneous intervention in two coronary loci in a patient with human immunodeficiency virus infection. World J Clin Cases 2017; 5(2): 40-45
- URL: https://www.wjgnet.com/2307-8960/full/v5/i2/40.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i2.40
Restenosis is encountered after coronary revascularisation and it is attributed as part of the arterial healing process in response to stents[1]. It had been a major drawback when using balloon angioplasty and bare metal stents but was reduced using drug eluting stents[2]. Procedural-related factors, such as stent malposition, coronary anatomy (e.g., ostial disease) and patient-specific considerations (e.g., diabetes) increase risk of instent restenosis (ISR)[1].
Human immunodeficiency virus (HIV) has been linked to increase risk of future cardiovascular events[3,4]. Contrary to earlier reports[5], restenosis was found to be comparable between patients with and without HIV infection[3,4]. The increase use of drug eluting stents may have contributed to the reduction in ISR in HIV population[6].
We have encountered a case of aggressive and recurrent restenosis in HIV patient despite using second-generation drug eluting stent. Below we described the details of this case with brief review of the literature.
A 54-year-old black African female was diagnosed HIV-positive 22 years prior to presentation with an acute coronary syndrome (ACS). She had been managed with combination of two nucleoside reverse transcriptase inhibitors (Lamivudine and Abacavir) in addition to two protease inhibitors (Lopinavir and Ritonavir). The CD4 count had been stable of 250 cells/mm3 with a viral load of 150-250 copies/mL. There was a history of treated hypertension and treated hypercholesterolemia.
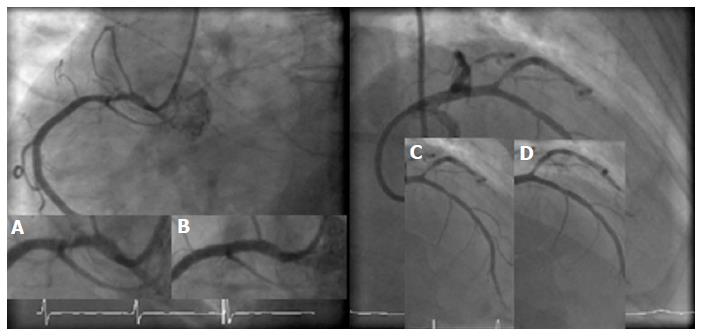
Her cardiac history (below) spans 20 mo. Initial presentation was with an episode of chest pain at rest associated with inferolateral ST segment depression on the ECG. Angiography revealed a 70% right coronary artery (RCA) lesion, which was treated with a 3.0 mm × 23 mm Xience (Abbott Vascular) Everolimus drug eluting stent (DES), post dilated with a 3.0 Quantum non-compliant balloon (Boston Scientific) (Figure 1A and B). In addition, she underwent balloon angioplasty to the first diagonal branch with 3.0 × 12 Maverick balloon (Boston Scientific) (Figure 1C and D).
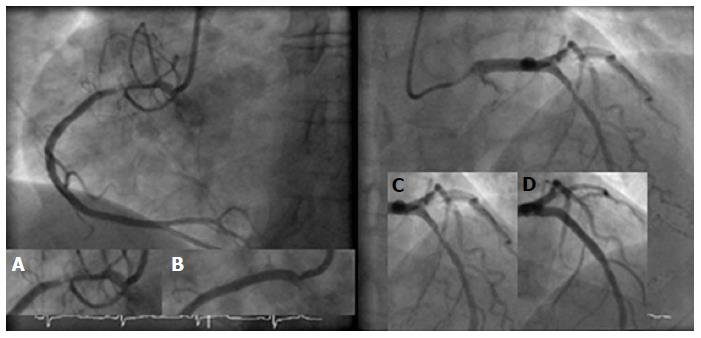
She represented 7 mo later with stable angina and was found to have a de novo lesion in the mid left anterior descending artery (LAD) with satisfactory result to the diagonal branch but severe in stent restenosis (ISR) in the previously stented RCA. The ISR segment was predilated with Maverick balloon (Boston Scientific) and a paclitaxel-eluting balloon was inflated to 18 atmosphere for 45 s (Figure 2A and B). The LAD lesion was stented with 3.5 mm × 23 mm Xience stent and post dilated with 3.5 × 12 Quantum non-complaint balloon (Figure 2C and D).
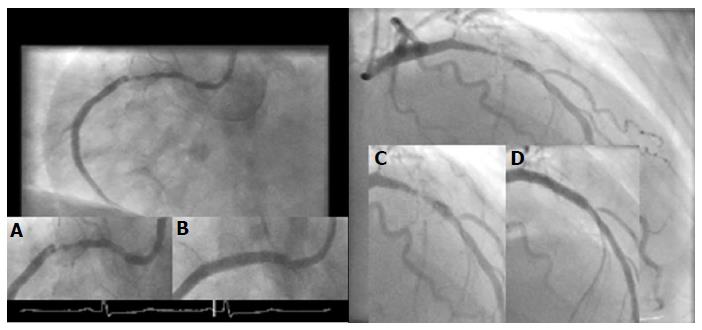
Eight months later, she presented again with an acute coronary syndrome. Repeat angiography demonstrated severe ISR in both the RCA and LAD stents. Following lesion preparation with a 3.0 cutting balloon, both RCA and LAD were stented - with 3.0 mm × 28 mm and 3.5 mm × 28 mm Xience stents respectively (Figure 3). Stents were post dilated to high pressure with 3.5 Quantum balloon. The end angiographic result was excellent in both arteries.
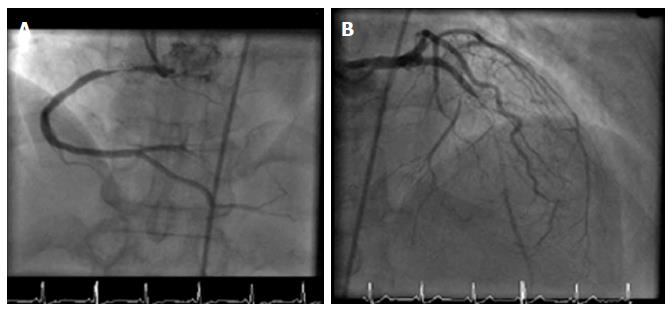
Yet, within 4 mo she was experiencing recurrent exertional chest discomfort. A further coronary angiogram showed subtotal occlusion of the LAD with TIMI2 flow and both antegrade and retrograde filling, from RCA. The occluded segment was within the distal portion of the stent. The RCA was sub totally occluded by severe ISR in the stented segment (Figure 4). It is worth noting that patient has reported satisfactory compliance with her dual anti platelets therapy throughout her multiple interventional procedures. She was referred for surgical revascularisation.
This case demonstrates exceptionally aggressive multifocal and recurrent instent restenosis in a patient treated for HIV infection. Restenosis can occur as part of an arterial healing response after injury following coronary stenting[1]. Neointimal hyperplasia occurs due to proliferation of smooth muscle cells and has been successfully ameliorated by the use of drug-eluting stents[2]. In contemporary series, the restenosis rate in first generation DES ranged between 0% and 16% depending on complexity of targeted lesions[7], while the rate of recurrent restenosis was 11%[8]. Factors associated with increased risk of ISR include: Diabetes mellitus, small calibre vessel disease, ostial disease and vein graft stenosis[1].
Treatment options are balloon catheter angioplasty, implantation of a second, coated or uncoated stent, mechanical debulking (e.g., rotablation), intracoronary irradiation (brachytherapy) and drug eluting balloon. These approaches have various rates of success[9].
In an HIV-positive population, a higher rate of ischemic heart disease compared to general population has been reported[10]. Although there was no difference in morbidity or mortality during hospital admission between HIV and general population, it was noted that on long term follow up there was an increased risk of recurrent ischemic events in HIV compared to non HIV presenting with ACS[3,4]. There was no difference in the rate of clinical restenosis between two groups[4]. Although it has previously been reported that target vessel revascularization and ISR were higher in HIV population[5], this trend was diminished in more contemporary studies[3,4]. This may be explained by the high rate of stenting in the latter studies with drug eluting stents leading to 60% fewer major adverse cardiovascular events in HIV population[6].
Antiretroviral therapy (ART) is a potential atherosclerotic risk in HIV patients[11]. Although this therapy has improved the care of HIV infection, metabolic side effects have been observed, including dyslipidaemia and insulin resistance[11]. The combination therapy was independently associated with increased rate of myocardial infarction[11]. Moreover, the incidence of myocardial infarction rose after the introduction of protease inhibitors[12]. This risk was still significant for protease inhibitor after adjustment for lipid concentration[10].
Nucleoside reverse transcriptase inhibitors did not show similar cardiovascular risk profile as protease inhibitors[13]. No associations between the rate of myocardial infarction and cumulative or recent use of zidovudine, stavudine, or lamivudine. On the other hand, recent, but not cumulative, use of Abacavir or Didanosine was associated with increase rate of myocardial infarction[14]. Interestingly, neither drug is thought to have substantial effect on metabolic profile[14].
In this case, patient was non-diabetic and both LAD and RCA stents were deployed at high pressure with satisfactory angiographic results. Everolimus eluting stents were persistently used to treat the restenosis in this case. It is unlikely that using another stent with different drug such as zotarolimus or biolimus may have changed the outcome. Recent meta-analysis demonstrated that although second generation stents carry lower risk of target vessel revascularisation compared to first generation stents (which eluted sirolimus or paclitaxel), there was no difference among everolimus, zotarolimus or biolimus drug eluting stents[15]. Whether HIV status may have influence on drug eluting stent outcome is not well documented and further research is warranted.
In this case, the HIV therapy had been stable and has not changed over the period of coronary intervention, and nor had the viral load or CD4 count. Yet, we observed aggressive restenosis raising the possibility of an association with her HIV infection or potentially components of her ART therapy. Although HIV infection causes attenuated inflammatory response to infections, it causes profound functional alterations of the endothelium, resembling the subclinical inflammation in atherosclerosis[16]. Leukocyte adherence to endothelium is enhanced as the expression of cell adhesion molecules increases[16]. Higher levels of soluble adhesion molecules have been found before the introduction of ART[17]. Moreover, ART has a stimulator effect on some of these molecules, enhancing HIV effect on endothelial function[17]. Furthermore, HIV infection can stimulate proliferation of human vascular smooth muscle cells and therefore promote atherosclerosis[10]. Although it has been reported that risk of restenosis in HIV corresponds to level of viral load[18], it is not clear whether smooth muscle cell proliferation and the accumulation of extracellular matrix, which are the main processes involved in in-stent restenosis, may be induced by protease inhibitors or by the HIV itself[19]. The chronic low-level inflammation in HIV patients may also contribute to their high rate of restenosis[5]. HIV patients have higher levels of C-reactive protein than their age and sex-matched controls[5].
This case shows exceptionally aggressive restenosis after PCI. As cardiovascular disease becomes more prevalent in patients with HIV, a subgroup of patients may emerge in whom this represents a significant clinical challenge. Better understanding of the responsible mechanisms may allow more tailored pharmacotherapy for susceptible individuals.
A 54-year-old lady with 22 years history of human immunodeficiency virus (HIV) on antiretroviral therapy.
Coronary artery disease with recurrent in-stent restenosis.
Stent thrombosis.
Rise in cardiac enzymes, including troponin.
Diagnostic angiogram confirming restenosis of coronary stents.
Despite attempts with percutaneous revascularisation, patient was eventually and successfully treated with surgical revascularisation.
ISR: In-stent restenosis.
The authors report a clinical case of a patient with HIV infection on antiretroviral therapy with recurrent in-stent restenosis requiring several percutaneous intervention and finally coronary artery bypass graft. The case is interesting and well written.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sabate M, Said SAM, Ueda H S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Lowe HC, Oesterle SN, Khachigian LM. Coronary in-stent restenosis: current status and future strategies. J Am Coll Cardiol. 2002;39:183-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 250] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 2. | Stettler C, Wandel S, Allemann S, Kastrati A, Morice MC, Schömig A, Pfisterer ME, Stone GW, Leon MB, de Lezo JS. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370:937-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1154] [Cited by in RCA: 1080] [Article Influence: 60.0] [Reference Citation Analysis (0)] |
| 3. | Boccara F, Teiger E, Cohen A, Ederhy S, Janower S, Odi G, Di Angelantonio E, Barbarini G, Barbaro G. Percutaneous coronary intervention in HIV infected patients: immediate results and long term prognosis. Heart. 2006;92:543-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Boccara F, Mary-Krause M, Teiger E, Lang S, Lim P, Wahbi K, Beygui F, Milleron O, Gabriel Steg P, Funck-Brentano C. Acute coronary syndrome in human immunodeficiency virus-infected patients: characteristics and 1 year prognosis. Eur Heart J. 2011;32:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Hsue PY, Giri K, Erickson S, MacGregor JS, Younes N, Shergill A, Waters DD. Clinical features of acute coronary syndromes in patients with human immunodeficiency virus infection. Circulation. 2004;109:316-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 155] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Ren X, Trilesskaya M, Kwan DM, Nguyen K, Shaw RE, Hui PY. Comparison of outcomes using bare metal versus drug-eluting stents in coronary artery disease patients with and without human immunodeficiency virus infection. Am J Cardiol. 2009;104:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Farooq V, Gogas BD, Serruys PW. Restenosis: delineating the numerous causes of drug-eluting stent restenosis. Circ Cardiovasc Interv. 2011;4:195-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 8. | Alfonso F, Pérez-Vizcayno MJ, Hernandez R, Bethencourt A, Martí V, López-Mínguez JR, Angel J, Mantilla R, Morís C, Cequier A. A randomized comparison of sirolimus-eluting stent with balloon angioplasty in patients with in-stent restenosis: results of the Restenosis Intrastent: Balloon Angioplasty Versus Elective Sirolimus-Eluting Stenting (RIBS-II) trial. J Am Coll Cardiol. 2006;47:2152-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 131] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 9. | Scheller B, Hehrlein C, Bocksch W, Rutsch W, Haghi D, Dietz U, Böhm M, Speck U. Treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. N Engl J Med. 2006;355:2113-2124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 580] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 10. | Boccara F, Lang S, Meuleman C, Ederhy S, Mary-Krause M, Costagliola D, Capeau J, Cohen A. HIV and coronary heart disease: time for a better understanding. J Am Coll Cardiol. 2013;61:511-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 207] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 11. | Friis-Møller N, Sabin CA, Weber R, d’Arminio Monforte A, El-Sadr WM, Reiss P, Thiébaut R, Morfeldt L, De Wit S, Pradier C. Combination antiretroviral therapy and the risk of myocardial infarction. N Engl J Med. 2003;349:1993-2003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1212] [Cited by in RCA: 1224] [Article Influence: 55.6] [Reference Citation Analysis (0)] |
| 12. | Holmberg SD, Moorman AC, Williamson JM, Tong TC, Ward DJ, Wood KC, Greenberg AE, Janssen RS. Protease inhibitors and cardiovascular outcomes in patients with HIV-1. Lancet. 2002;360:1747-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 337] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 13. | Sabin CA, Worm SW, Weber R, Reiss P, El-Sadr W, Dabis F, De Wit S, Law M, D’Arminio Monforte A, Friis-Møller N. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D: A: D study: a multi-cohort collaboration. Lancet. 2008;371:1417-1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 636] [Cited by in RCA: 661] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 14. | Anastos K, Lu D, Shi Q, Tien PC, Kaplan RC, Hessol NA, Cole S, Vigen C, Cohen M, Young M. Association of serum lipid levels with HIV serostatus, specific antiretroviral agents, and treatment regimens. J Acquir Immune Defic Syndr. 2007;45:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Palmerini T, Benedetto U, Biondi-Zoccai G, Della Riva D, Bacchi-Reggiani L, Smits PC, Vlachojannis GJ, Jensen LO, Christiansen EH, Berencsi K. Long-Term Safety of Drug-Eluting and Bare-Metal Stents: Evidence From a Comprehensive Network Meta-Analysis. J Am Coll Cardiol. 2015;65:2496-2507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 375] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 16. | Sudano I, Spieker LE, Noll G, Corti R, Weber R, Lüscher TF. Cardiovascular disease in HIV infection. Am Heart J. 2006;151:1147-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | de Gaetano Donati K, Rabagliati R, Tumbarello M, Tacconelli E, Amore C, Cauda R, Lacoviello L. Increased soluble markers of endothelial dysfunction in HIV-positive patients under highly active antiretroviral therapy. AIDS. 2003;17:765-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Matetzky S, Domingo M, Kar S, Noc M, Shah PK, Kaul S, Daar E, Cercek B. Acute myocardial infarction in human immunodeficiency virus-infected patients. Arch Intern Med. 2003;163:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Segev A, Cantor WJ, Strauss BH. Outcome of percutaneous coronary intervention in HIV-infected patients. Catheter Cardiovasc Interv. 2006;68:879-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |