Published online Dec 16, 2017. doi: 10.12998/wjcc.v5.i12.419
Peer-review started: March 2, 2017
First decision: May 23, 2017
Revised: September 10, 2017
Accepted: November 22, 2017
Article in press: November 22, 2017
Published online: December 16, 2017
Neurofibromatosis type 1 is a congenital condition affecting neurons and connective tissue integrity including vasculature. On extremely rare occasions these patients present with venous aneurysms affecting the internal jugular vein. If they become large enough there presents a risk of rupture, thrombosis, embolization or compression of adjacent structures. In these circumstances, or when the patient becomes symptomatic, surgical exploration is warranted. We present a case of one of the largest aneurysms in the literature and one of only five associated with Neurofibromatosis type 1. A 63-year-old female who initially presented for a Hinchey III diverticulitis requiring laparotomy developed an incidentally discovered left neck swelling prior to discharge. After nonspecific clinical exam findings, imaging identified a thrombosed internal jugular vein aneurysm. Due to the risks associated with the particularly large size of our patient’s aneurysm, our patient underwent surgical exploration with ligation and excision. Although several techniques have been reported, for similar presentations, we recommend this technique.
Core tip: Neurofibromatosis type 1 is a congenital condition occasionally affecting vascular connective tissue integrity. On extremely rare occasions these patients present with internal jugular venous aneurysms. We present a case of the successful ligation and excision of one of the largest internal jugular vein aneurysms in the literature and one of only five associated with Neurofibromatosis type 1.
- Citation: Delvecchio K, Moghul F, Patel B, Seman S. Surgical resection of rare internal jugular vein aneurysm in neurofibromatosis type 1. World J Clin Cases 2017; 5(12): 419-422
- URL: https://www.wjgnet.com/2307-8960/full/v5/i12/419.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i12.419
Initially described by Gruber[1] in 1875, internal jugular (IJ) aneurysms are rare entities with under 400 reported in the last 100 years in the literature. As described by Lubianca-Neto et al[2] these lesions have historically been described as “congenital venous cyst, venous pseudoaneurysm, venous ectasia, venous aneurysm, venous cyst, venoma, and internal jugular phlebectasia” in the literature, with an average age of under 10 and over 60% under age 40[3,4]. They most commonly occur on the right side, however may be bilateral in as many as 10% of cases[5,6]. These aneurysms classically present as unilateral, asymptomatic, soft, compressible neck swellings that enlarge with Valsalva[1-3]. Due to the relationship of the IJ abutting the vagus nerve within the carotid sheath, patients may complain of hoarseness, dysphagia or foreign body sensation[1,5,7]. Moreover, the absence of bruit or pulsation on physical exam excludes a more ominous arterial pathology[1,8].
While the underlying physiology that makes a particular patient susceptible to aneurysm formation is largely unknown, several inciting factors have been reported in the literature. These include trauma from central venous catheterization, positive-pressure ventilation, inflammation, distal obstruction from a mass, or unknown idiopathic causes[2,7,9]. Additionally, pathological analyses of resected aneurysms have described congenital thinning of the elastic and muscular layers of the venous wall, and/or elastin dysplasia[10,11]. Not surprisingly, disorders of connective tissue, including Ehlers-Danlos and Neurofibromatosis type 1 (NF1), have been linked to these anomalies[4,12-14].
NF1 aka von Recklinghausen’s disease is an autosomal dominant mutation of chromosome 17 occurring in 1 in 3000 people that alters the neurofibromin protein, affecting the structural integrity of connective tissues and nerves[12,13]. Typical presentations include neurofibromas, café au lait macules, Lisch hamartomas, meningiomas, and gliomas[13,14]. Rarer manifestations involve the vasculature which can be present in up to 6.4% of patients, however it primarily involves the arterial system[12,15]. We present a case of the successful ligation and excision of one of the largest IJ vein aneurysms in the literature and one of only five associated with NF1.
A 63-year-old Caucasian female with a medical history significant for Neurofibromatosis presented to the emergency room with bilateral lower quadrant abdominal pain, diarrhea, emesis and complaints of fevers and chills for one day. She was tachycardic and peritoneal on examination and thus taken to the operating room where she underwent sigmoid resection with end colostomy and Hartmann’s pouch for Hinchey III diverticulitis. Postoperatively the patient remained intubated and was admitted to the ICU and had a left subclavian central venous catheter placed for vasopressor support. After a series of setbacks, the patient began to improve significantly around postoperative day (POD) 11 and her subclavian line was able to be removed. By POD 15 the patient was ready for discharge to rehab.
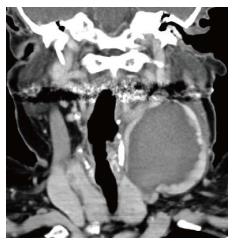
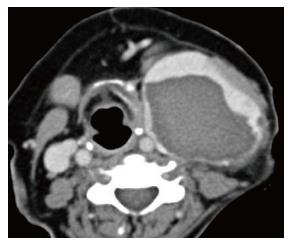
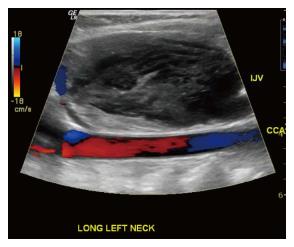
Upon preparing for departure the patient noticed in the mirror a bulge in her left neck that she did not previously feel. The nursing staff and subsequently physicians were notified. Upon examination there was no noticeable mass as the patient had significant submental ptosis. A computed tomography (CT) scan of the neck was performed which showed a 5.8 cm × 6.9 cm × 5.4 cm internal jugular collection with anterior displacement of the sternocleidomastoid (SCM) (Figures 1 and 2). The vascular surgeon was notified and a triplex ultrasound was performed showing a 6.9 cm × 3.8 cm × 6.5 cm internal jugular thrombus with minimal superior flow and a patent subclavian (Figure 3).
On POD 16 the patient was taken to the operating room where she underwent evacuation, resection and ligation of the internal jugular aneurysm via an anterior SCM incision. Small internal branches were ligated and the anterior vein wall was sutured closed. There was an estimated blood loss of 1 liter during dissection due to avulsion of many of these internal branches. The skin was closed and a Jackson-Pratt (JP) drain was left subcutaneously. Postoperatively the JP was removed on day 1 due to minimal output and the patient was able to be discharged home on day 2.
Limitations to our workup include not submitting the aneurysmal wall for pathological analysis as 3 of the 4 described aneurysms associated with NF1 in the literature describe histopathological invasion of NF1 into the wall[12,14,15]. While not necessary for the diagnosis, it could have helped substantiate a more definitive pathological explanation. Additionally, several authors have recommended that the diagnostic workup include bilateral triplex ultrasound performed with Valsalva[4-6]. The importance of a size increase with Valsalva during examinations is underscored by the fact that the majority of differential diagnoses can be ruled out if absent, leaving phlebectasias, laryngoceles and superior mediastinal cyst[4]. The most common of these, laryngocele, can be ruled out with laryngoscopy, whereas mediastinal cysts can be ruled out with CT scan[5]. Although our patient’s diagnosis was easily identified with CT and confirmed with triplex ultrasound, it was not performed with these particular suggestions in mind.
Although clinical exam can provide a significant amount of information, because of the low overall rate of complications there is often adequate time for definitive imaging. As mentioned previously, triplex ultrasound is the current standard for diagnostic accuracy as it will allow for characterization of the aneurysmal size as well as visualization of directional blood flow and thrombosis[2,4,5]. Additionally, Passariello et al[16], described four cases in children that were successfully characterized with endovascular digital subtraction contrast fluoroscopy which has the additional benefit of simultaneous diagnosis and intervention[17].
As described above, a commonly cited etiology of IJ aneurysms is traumatic central venous catheterization[7]. A limitation with our case was the prolonged duration with which her left subclavian line was in place, possibly leading to thrombosis and propagation. It is difficult to definitively determine if the subclavian line was the inciting event, however it is likely it participated in a genetically susceptible patient.
IJ aneurysms have rarely been reported on and only a handful have been described in association with NF1 (Table 1)[12-15]. These lesions typically present much larger than other cases and ours, at 6.9 cm × 5.8 cm × 5.4 cm, is one of the largest described in the literature. Each of these aneurysms were surgically resected and each had significant blood loss[12-15].
| Ref. | Age/sex | Side | Size (cm) | Treatment | Thrombosed | Confirmed NF1 in wall |
| Nopajaroonsri and Lurie[14] (1996) | 62 M | Left | 10 × 5 × 4.5 | Resection | Yes | Yes |
| Oderich et al[13] (2007) | 73 M | Right | “Giant” | Resection | Yes | |
| Belcastro et al[15] (2011) | 60 F | Left | 12 × 12 × 10 | Resection | Yes | Yes |
| Hiraki et al[12] (2014) | 60 M | Left | 5.5 × 5 × 2 | Resection | Yes | Yes |
| The present case | 63 F | Left | 6.9 × 5.8 × 5.4 | Resection | Yes |
With regard to management, because IJ aneurysms are considered to be self-limiting, operative intervention is usually reserved for cosmetic or symptomatic reasons[2,5,10,18]. Although extremely rare, if there is significant concern for thrombosis, embolization or impending rupture, resection is justified[10]. Various approaches have been described which have been largely based on size and location, including anterior SCM, transverse cervical and median sternotomy incisions[4,5,15]. Additionally Chua et al[17], describe a combined endovascular balloon ligation and open resection, allowing for a smaller incision. Regardless of the approach, it is important preoperatively to confirm contralateral patency for cerebral edema prevention[2] as Hu et al[8], reported 2 cases of unilateral ligation of bilateral lesions resulting in 3 d of cerebral swelling. While many IJ vein aneurysms have reportedly been followed successfully without intervention for up to 15 years, no studies have been performed that compare long-term outcomes of any kind[6]. This leads to the suggestion of future randomized trials featuring long-term outcomes of conservative management vs various surgical procedures.
A 63-year-old woman with neurofibromatisis type 1 who developed an incidentally discovered internal jugular vein aneurysm that was surgically resected.
Compressible left-sided neck swelling without dysphagia or respiratory compromise.
Differential diagnoses include phlebectasias, laryngoceles, superior mediastinal cyst, thyroglossal duct cyst, cystic hygroma, branchial cleft cyst, pharyngocele, dermoid cyst, thyroid mass, arteriovenous malformation, carotid body tumor and squamous cell carcinoma of the neck.
All labs were within normal limits.
Computed tomography scan showed a 5.8 cm × 6.9 cm × 5.4 cm internal jugular collection with anterior displacement of the sternocleidomastoid. A triplex ultrasound showed a 6.9 cm × 3.8 cm × 6.5 cm internal jugular thrombus with minimal superior flow and a patent subclavian.
Surgical evacuation, resection and ligation of the aneurysm.
Internal jugular venous aneurysms have historically gone by several names in the literature and despite very few resulting in significant morbidity with expectant management alone, they are frequently surgically resected.
Triplex ultrasound is an imaging method that uses color to highlight direction of vascular flow. It is the recommended diagnostic method to characterize these lesions.
Patients with neurofibromatosis type 1 are particularly susceptible to internal jugular vein aneurysms due to vascular wall abnormalities, which should be noted when inciting etiological events occur such as central venous catheterization.
The information and brief literature review provided was sufficient.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lai V S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Sander S, Eliçevik M, Unal M, Vural O. Jugular phlebectasia in children: is it rare or ignored? J Pediatr Surg. 1999;34:1829-1832. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Lubianca-Neto JF, Mauri M, Prati C. Internal jugular phlebectasia in children. Am J Otolaryngol. 1999;20:415-418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Refson JS, Wolfe JH. An aneurysm of the internal jugular vein. Eur J Vasc Endovasc Surg. 1996;11:371-372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Jianhong L, Xuewu J, Tingze H. Surgical treatment of jugular vein phlebectasia in children. Am J Surg. 2006;192:286-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Hung T, Campbell AI. Surgical repair of left internal jugular phlebectasia. J Vasc Surg. 2008;47:1337-1338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Haney JC, Shortell CK, McCann RL, Lawson JH, Stirling MJ, Stone DH. Congenital jugular vein phlebectasia: a case report and review of the literature. Ann Vasc Surg. 2008;22:681-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Nakayama M, Fujita S, Kawamata M, Namiki A, Mayumi T. Traumatic aneurysm of the internal jugular vein causing vagal nerve palsy: a rare complication of percutaneous catheterization. Anesth Analg. 1994;78:598-600. [PubMed] [Cited in This Article: ] |
| 8. | Hu X, Li J, Hu T, Jiang X. Congenital jugular vein phlebectasia. Am J Otolaryngol. 2005;26:172-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Spiro SA, Coccaro SF, Bogucki E. Aneurysm of the internal jugular vein manifesting after prolonged positive pressure ventilation. Head Neck. 1991;13:450-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Swaika S, Basu S, Bhadra RC, Maitra S. Multiple venous aneurysms of neck. J Indian Assoc Pediatr Surg. 2013;18:25-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Danis RK. Isolated aneurysm of the internal jugular vein: a report of three cases. J Pediatr Surg. 1982;17:130-131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Hiraki T, Higashi M, Goto Y, Kitazono I, Yokoyama S, Iuchi H, Nagano H, Tanimoto A, Yonezawa S. A rare case of internal jugular vein aneurysm with massive hemorrhage in neurofibromatosis type 1. Cardiovasc Pathol. 2014;23:244-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Oderich GS, Sullivan TM, Bower TC, Gloviczki P, Miller DV, Babovic-Vuksanovic D, Macedo TA, Stanson A. Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. J Vasc Surg. 2007;46:475-484. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 250] [Cited by in F6Publishing: 269] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 14. | Nopajaroonsri C, Lurie AA. Venous aneurysm, arterial dysplasia, and near-fatal hemorrhages in neurofibromatosis type 1. Hum Pathol. 1996;27:982-985. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 64] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Belcastro M, Palleschi A, Trovato RA, Landini R, Di Bisceglie M, Natale A. A rare case of internal jugular vein aneurysmal degeneration in a type 1 neurofibromatosis complicated by potentially life-threatening thrombosis. J Vasc Surg. 2011;54:1170-1173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Passariello R, Cozzi F, Casalena G, Colarossi G, Rossi P, Simonetti G. Angiographic diagnosis of jugular venous system dilatation in children. A report of five cases. Pediatr Radiol. 1979;8:247-250. [PubMed] [Cited in This Article: ] |
| 17. | Chua W, Xu G, Cheng SC. Hybrid surgical management of a saccular aneurysm of the internal jugular vein. Singapore Med J. 2012;53:e90-e91. [PubMed] [Cited in This Article: ] |
| 18. | Khashram M, Walker PJ. Internal jugular venous aneurysm. J Vasc Surg Venous Lymphat Disord. 2015;3:94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |