Published online Nov 16, 2017. doi: 10.12998/wjcc.v5.i11.403
Peer-review started: July 26, 2017
First decision: August 16, 2017
Revised: August 25, 2017
Accepted: September 12, 2017
Article in press: September 13, 2017
Published online: November 16, 2017
Cervical inlet patch (CIP), also referred to as esophageal heterotopic gastric mucosa, is regarded as the residue of columnar epithelium of the embryonic esophagus. Narrow band imaging increases the detection rate of CIP. Herein, we present a 55-year-old man with symptomatic circumferential inlet patch. He exhibited globus and dysphagia, and esophagogastroduodenoscopy found cir-cumferential CIP, where im-munohistochemistry revealed the existence of pro-ton pumps (H+, K+-ATPase). His throat symptoms were relieved by acid suppressive therapy with pump inhibitors. This case indicated that CIP should be considered as a differential diagnosis for the cause of globus symptoms in rare cases.
Core tip: Cervical inlet patch (CIP) is the esophageal heterotopic gastric mucosa in the cervical esophagus. We present a 55-year-old man exhibiting circumferential CIP with globus and dysphagia. Proton pump inhibitors relived these throat symptoms. Immunohistochemistry revealed existence of proton pumps in the CIP lesion. The throat symptoms were suggested to be related with CIP and acid secretion.
- Citation: Yamada T, Tsuji A, Onoue S, Kaneko M, Tanioka F, Osawa S, Saida Y. Acid suppressive therapy improved symptoms due to circumferential cervical inlet patch with proton pumps (H+/K+-ATPase). World Journal of Clinical Cases 2017; 5(11): 403-406
- URL: https://www.wjgnet.com/2307-8960/full/v5/i11/403.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i11.403
Esophageal heterotopic gastric mucosa (HGM), also referred to as cervical inlet patch (CIP), is considered to be the residue of columnar epithelium of the embryonic esophagus[1,2]. The diagnosis rate of CIP is increasing because of the recent development and spread of image-enhanced endoscopy, including narrow band imaging (NBI)[3,4]. Patients with CIP rarely require treatment as most cases of CIP are asymptomatic. However, some reports indicated complications associated with acid secretion from CIP[5-7]. Herein, we present a patient with circumferential CIP in whom proton pump in-hibitors (PPI) were effective and proton pump existence was confirmed by immunohistochemistry.
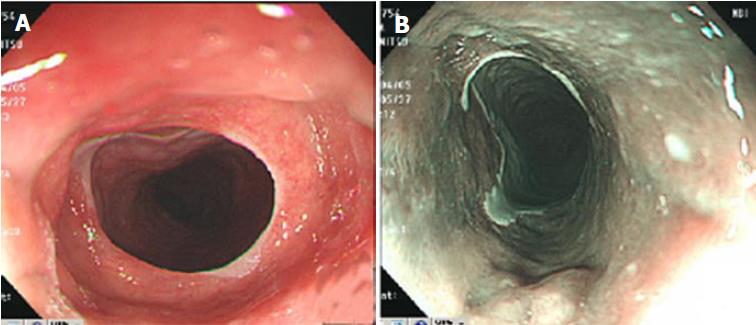
A 55-year-old man visited the department of otolaryngology exhibiting globus and dysphagia without heartburn or epigastric pain. His past medical history only included an operation for appendicitis. Physical examination and laboratory findings were unremarkable. Laryngoscopy did not reveal the cause of the throat symptoms. He was then introduced to the department of gastroenterology and esophagogastroduodenoscopy (EGD) was performed to determine the cause. EGD revealed circular HGM in the cervical esophagus, the HGM was 19 to 21 cm from the incisor. The lesion appeared reddish by white light imaging (Figure 1A), whereas by NBI, it appeared as a dark brown lesion clearly distinguished from light green squamous epithelium (Figure 1B). There was only mild reflux esophagitis (Los Angeles grade A), but no esophageal hiatus hernia at the esophagogastric junction. His throat symptoms improved quickly by acid suppression therapy with PPI.
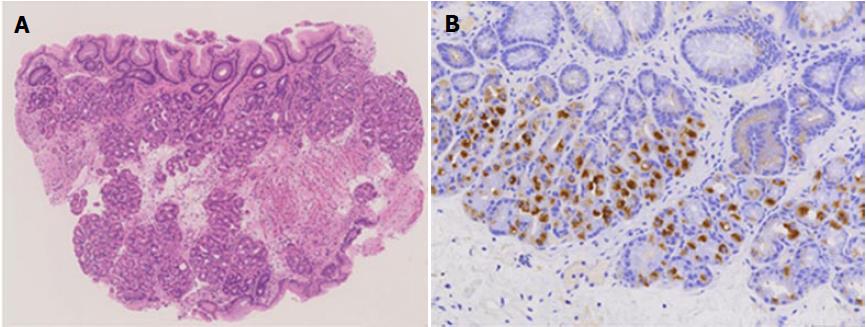
Endoscopic biopsy from the circumferential CIP lesion demonstrated foveolar epithelium and fundic glands (Figure 2A). Furthermore, to confirm the relationship between the throat symptoms and acid secretion from the CIP, we performed immunohistochemistry and found proton pump, H+, K+-ATPase alpha subunits. Immunohistochemical staining was concentrated in the glands of CIP (Figure 2B).
CIP, also referred to as cervical esophageal HGM, is generally regarded as a congenital condition that results from an incomplete replacement by squamous epithelium, and the differentiation of persistent columnar-lined mucosa into cervical HGM[1,2]. The incidence of CIP was reported as 0.1% to 13.8%[3,8]. Using NBI endoscopy, there was increase in the detection of CIP[4].
Some reports demonstrated acid secretion from CIP using pH monitoring[5-7]. Here, we demonstrated the existence of proton pumps (H+, K+-ATPase) in CIP in a symptomatic patient by immunohistochemistry. The efficacy of PPI also supports the theory that acid secretion from proton pumps in CIP is the cause of throat symptoms. In the present case, the patient had mild esophagitis. Although there is a possibility that gastroesophageal reflux disease was one of the causes of the globus symptoms, we considered cervical CIP to be the main cause of his globus symptoms because of the existence of proton pumps in the large CIP and the previous reports of the relationship between throat symptoms and acid secretion from CIP. However, this case report did not directly show the relationship between existence of proton pumps and their acid secretion function in CIP. Further studies are needed to demonstrate the usefulness of immunohistochemistry for proton pump to predict PPI efficacy in patients with symptomatic CIP.
Recently, argon plasma coagulation and radio-frequency ablation were reported to be effective for symptomatic CIP[9-11]. However, these endoscopic ablation techniques are not available in all countries, including Japan. PPI treatment is more widely available than endoscopic ablation. PPI should be selected first in such situations. Furthermore, the detection of proton pumps by immunohistochemistry may predict the efficacy of PPI for throat symptoms in patients with CIP.
In summary, we reported a 55-year-old man with circumferential CIP where immunohistochemistry revealed proton pump existence. His throat symptoms were relieved by acid suppressive therapy with PPI. This case indicated that CIP should be considered as a differential diagnosis for the cause of globus symptoms in rare cases.
A 55-year-old man visited to complaint globus and dysphagia without heartburn or epigastric pain.
Endoscopy revealed circumferential cervical inlet patch (CIP).
Gastroesophageal reflux and globus hystericus.
Esophagogastroduodenoscopy revealed circumferential CIP, where appeared reddish by white light imaging and appeared as a dark brown clearly distinguished from light green squamous epithelium by narrow band imaging.
Immunohistochemistry for proton pump alpha subunit demonstrated concentration of staining in glands of CIP.
Acid suppressive therapy with proton pump inhibitors (PPI) improved globus and dysphagia in a patient with CIP.
Although some reports demonstrated acid secretion from CIP using pH monitoring, this is the first report that demonstrated the existence of proton pumps (H+, K+-ATPase) in CIP in a symptomatic patient by immunohistochemistry. The relationship should be elucidated between the existence of proton pump and acid secreting function in CIP.
CIP is esophageal heterotopic gastric mucosa, which is considered to be the residue of columnar epithelium of the embryonic esophagus.
CIP should be considered as a differential diagnosis for the cause of globus symptoms in rare cases.
This case report clearly presented a case of CIP which expressed the proton pump and was successfully treated by PPI.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chen XX, Guo YM, Watson DI S-Editor: Chen K L-Editor: A E-Editor: Zhao LM
| 1. | von Rahden BH, Stein HJ, Becker K, Liebermann-Meffert D, Siewert JR. Heterotopic gastric mucosa of the esophagus: literature-review and proposal of a clinicopathologic classification. Am J Gastroenterol. 2004;99:543-551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Chong VH. Clinical significance of heterotopic gastric mucosal patch of the proximal esophagus. World J Gastroenterol. 2013;19:331-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 55] [Cited by in F6Publishing: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Hori K, Kim Y, Sakurai J, Watari J, Tomita T, Oshima T, Kondo C, Matsumoto T, Miwa H. Non-erosive reflux disease rather than cervical inlet patch involves globus. J Gastroenterol. 2010;45:1138-1145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Cheng CL, Lin CH, Liu NJ, Tang JH, Kuo YL, Tsui YN. Endoscopic diagnosis of cervical esophageal heterotopic gastric mucosa with conventional and narrow-band images. World J Gastroenterol. 2014;20:242-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Galan AR, Katzka DA, Castell DO. Acid secretion from an esophageal inlet patch demonstrated by ambulatory pH monitoring. Gastroenterology. 1998;115:1574-1576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Kim EA, Kang DH, Cho HS, Park DK, Kim YK, Park HC, Kim JH. Acid secretion from a heterotopic gastric mucosa in the upper esophagus demonstrated by dual probe 24-hour ambulatory pH monitoring. Korean J Intern Med. 2001;16:14-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Korkut E, Bektaş M, Alkan M, Ustün Y, Meco C, Ozden A, Soykan I. Esophageal motility and 24-h pH profiles of patients with heterotopic gastric mucosa in the cervical esophagus. Eur J Intern Med. 2010;21:21-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Maconi G, Pace F, Vago L, Carsana L, Bargiggia S, Bianchi Porro G. Prevalence and clinical features of heterotopic gastric mucosa in the upper oesophagus (inlet patch). Eur J Gastroenterol Hepatol. 2000;12:745-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 77] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Meining A, Bajbouj M, Preeg M, Reichenberger J, Kassem AM, Huber W, Brockmeyer SJ, Hannig C, Höfler H, Prinz C. Argon plasma ablation of gastric inlet patches in the cervical esophagus may alleviate globus sensation: a pilot trial. Endoscopy. 2006;38:566-570. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Bajbouj M, Becker V, Eckel F, Miehlke S, Pech O, Prinz C, Schmid RM, Meining A. Argon plasma coagulation of cervical heterotopic gastric mucosa as an alternative treatment for globus sensations. Gastroenterology. 2009;137:440-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 72] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 11. | Dunn JM, Sui G, Anggiansah A, Wong T. Radiofrequency ablation of symptomatic cervical inlet patch using a through-the-scope device: a pilot study. Gastrointest Endosc. 2016;84:1022-1026.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |