Published online Sep 16, 2016. doi: 10.12998/wjcc.v4.i9.281
Peer-review started: April 29, 2016
First decision: May 17, 2016
Revised: June 3, 2016
Accepted: July 11, 2016
Article in press: July 13, 2016
Published online: September 16, 2016
Processing time: 131 Days and 13.1 Hours
The aim of this study was to present a case of enteric duplication cyst and criteria for a proper differential diagnosis. A 51-year-old male was hospitalized for pancreatic tail neoplasm and distal pancreatectomy with splenectomy was performed. During surgery, a jejunal cystic lesion was incidentally detected and jejunectomy was performed. Microscopically, the cyst was observed to be covered by Keratin 7/Keratin 20 positive intestinal type epithelium and the muscularis layer was shared by the cyst and adjacent jejunum, without a cleavage plane between the cyst wall and jejunal muscularis propria. In the deep muscularis propria, a Heinrich’s type I ectopic pancreas was also noted. In the pancreatic tail, a low grade intraepithelial lesion (panIN-1a) was diagnosed. This case highlights the necessity for a correct differential diagnosis of such rare lesions. Roughly 30 cases of jejunal duplication cysts have been reported to date in the PubMed database.
Core tip: In this paper we presented a very rare case of an incidentally diagnosed jejunal duplication cyst in a patient with a pancreatic tail neoplasm. The association between duplication cyst and ectopic pancreas supports the theory of an embryonal development disorder.
- Citation: Gurzu S, Bara Jr T, Bara T, Fetyko A, Jung I. Cystic jejunal duplication with Heinrich’s type I ectopic pancreas, incidentally discovered in a patient with pancreatic tail neoplasm. World J Clinical Cases 2016; 4(9): 281-284
- URL: https://www.wjgnet.com/2307-8960/full/v4/i9/281.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i9.281
Cystic subepithelial lesions of the gastrointestinal (GI) tract are uncommon in adults and can be indicators of an ectopic pancreas, Meckel’s diverticulum, duplication cysts, cystic GI stromal tumors, neuroendocrine tumors and lymphangiomas[1-6]. An ectopic pancreas, which is defined as the presence of pancreatic tissue in abnormal locations without anatomical and vascular continuity with the pancreas, can occur as a nodular or cystic lesion confined to the submucosa and muscularis propria[1]. Based on the von Heinrich classification (1909), the ectopic pancreas can be composed of ducts, acini and Langerhans islands (Heinrich’s type I), duct and acini without islands (Heinrich’s type II), or only several ducts, some of them cystically dilated without exocrine or endocrine components (Heinrich’s type III heterotopy)[3]. Meckel’s diverticulum occurs as a result of cystic dilatation of the omphalomesenteric duct remnants and arises from the antimesenteric border of the small intestine[4].
Enteric duplication cysts are primarily diagnosed during early childhood and supposedly the result of developmental anomalies[4-7]. They represent 60% of all the cystic lesions of the GI tract[4]. Roughly 75% of the duplication cysts have been reported in the abdominal cavity, the most frequent location being the ileum (22%-60% of abdominal cavity duplication cysts), followed by the jejunum (8%-16%), colon (7%), stomach (2%-9%) and appendix[1,2,5-8]. The remaining 25% of cysts can involve the intrathoracic or thoracoabdominal organs[7]. In contrast to Meckel’s diverticulum, it develops along the mesenteric border of the adjacent intestine and shares the mesenteric blood supply[4,6]. Macroscopically, the duplication cysts are classified as spherical or tubular cysts that can communicate (or not) with the GI lumen[4,8].
In this paper, we present a rare case of a spherical, communicating duplication cyst of the jejunum associated with pancreatic heterotopy.
A 51-year-old male with chronic alcohol abuse was admitted to hospital with intermittent abdominal pain that increased in intensity after meals and jaundice of the mucosae and skin. He had a two-year history of steatohepatitis, chronic pancreatitis, as well as secondary insulin-dependent diabetes mellitus.
The ultrasonographic examination revealed enlargement of the pancreatic tail. Blood analysis showed slight anemia (hemoglobin 9.8 g/dL; hematocrit 29.2%), normal glycemia, and slightly increased serum levels of amylase (141 u/L).
Due to magnetic resonance imaging (MRI)-based suspecting a pancreatic tumor and mechanical jaundice, it was decided to perform a laparotomy. A splenectomy and pancreatic tail resection was performed. No gallstones were identified. The intraoperative exploration of the abdominal cavity also revealed a well-defined jejunal cystic swelling. The resection of the jejunum (135 mm in lenght) and end-to-end anastomosis was performed.
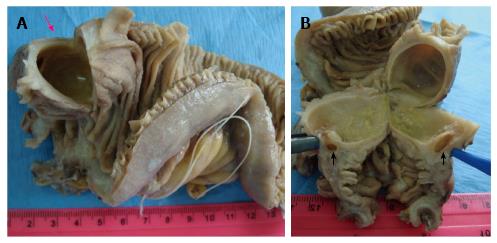
Gross examination of the surgical specimens showed a fibrotic pancreatic tail. The round-shaped cystic lesion of the jejunum had a diameter of 20 mm and was covered by intact jejunal mucosa. The serosal surface was intact. On the cut section, the monolocular cyst was filled with serous fluid and had a smooth inner surface. The cystic wall thickness was roughly 2-3 mm (Figure 1).
Histopathological examination revealed large fibrotic areas in the pancreatic tail and pancreatic ducts with focal dysplasia (panIN-1a). The jejunal cyst was covered by Keratin 20 positive intact jejunal mucosa. It was located in the submucosa and muscularis propria. A cystic denuded inner surface with fragmented flat epithelium, marked by both Keratin 20 and Keratin 7 was noted and the capillary rich granulation tissue dissociated the underlying smooth muscle fibers. The muscularis layer was shared by the cyst and adjacent jejunum. The communication area was also lined by granulation tissue. In the deep muscularis propria, proliferation of pancreatic-type Keratin 7 positive/Keratin 20 negative ducts and acini, without cytological atypia, as well as rare Langerhans islands were also observed. No positivity for c-KIT or DOG-1 was noted.
Based on the macroscopic and microscopic findings, the final diagnosis was “jejunal duplication cysts, with synchronous Heinrich’s type I ectopic pancreas[3] and low grade intraepithelial neoplasia of the pancreatic tail”.
Postoperative evolution was uneventful. The patient refused to stop alcohol consumption. At 27 mo after surgery he was admitted to hospital with scleral jaundice and a 7 mm large gallstone was found in the common bile duct. Laparoscopic choledochoduodenostomy was performed without postoperative complications.
Due to its unusual occurrence, no diagnosis guidelines or therapy have been elaborated for GI cystic duplications. Most of these are found incidentally during surgery for other abdominal conditions[1,4-7], similar to the present case.
In the intestine, spherical type cysts are predominate[4,6]. They have thick walls and are filled with clear secretions or mucus and generally do not communicate with the intestinal lumen[6]. Tubular duplications are long cystic lesions, involving more than one GI segment, with possible communication with the adjacent intestine[6]. In the present case, the spherical cyst contained serous fluid and there was communication with the intestinal lumen that favored the inflammatory process.
Where the jejunum is concerned, the first two reports of cystic lesions were published in 1950[9,10] and roughly 30 cases of jejunal duplication cysts have been reported to date in the PubMed database.
The microscopic diagnosis of a GI duplication cyst is based on the following features: A well-defined cyst firmly attached to the adjacent GI segment, lined by gastric or intestinal mucosa, surrounded by at least one well-developed smooth muscle layer, without a cleavage plane between the cyst and muscularis propria[4-7].
Pathogenesis appears to be related to embryonic development disorders. Due to frequent localization of these lesions in the stomach on the greater curvature (95% of all gastric cysts), it was assumed that they develop during embryogenesis dorsally to the primitive gut[4]. In some patients, heterotopic gastric, intestinal, or respiratory mucosa, but also annular or an ectopic pancreas (similar to the present case) was associated[4-6,8]. In other cases, communication between the cyst and the vertebral canal, spina bifida, or involvement of the mesenteric arteries was seen[8]. Based on these facts, etiopathogenetic theories include disorders of the embryonal development of the digestive system similar to the persistence of embryonic diverticula, partial twinning, vascular malformations, a split notochord (which explains association of spina bifida) and aberrant re-canalization following the solid phase of fetal enteric mucosal development[6,7]. Intrauterine hypoxia- or trauma-related division of the intestinal lumen can also be involved[6,7].
In the present case, the asymptomatic jejunal duplication cyst was incidentally found intraoperatively in a patient diagnosed with intraepithelial neoplasia of the pancreatic tail, developed as part of a background that included chronic alcoholic pancreatitis. The association between duplication cyst and ectopic pancreas supports the theory of an embryonal development disorder.
A 51-year-old male with recurrent abdominal pain.
Pancreatic tail neoplasm in a patient with chronic alcohol-related pancreatitis.
Other cystic lesions of the gastrointestinal (GI) tract including ectopic pancreas in the jejunum.
Non-specific - slight anemia and increased level of amylases.
Computed tomography-scan-pancreatic tail neoplasia.
Intraepithelial neoplasia of the pancreas associated with incidentally discovered jejunal cystic duplication with Heinrich’s type I ectopic pancreas.
Splenectomy, pancreatic tail resection and resection of the jejunum.
About 30 cases of jejunal duplication cysts.
Enteric duplication cyst is a well defined cystic malformation, which can involve any of the GI segments. It is firmly attached to the adjacent GI segment, lined by gastric or intestinal mucosa, and surrounded by at least one well developed smooth muscle layer, without a cleavage plane between the cyst and muscularis propria.
This case report shows the criteria used for differential diagnosis of cystic lesions of the jejunum and summarizes the hypotheses about the origin of these cysts.
The case is very well presented.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: Romania
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lassandro F, Wani IA S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Hirasaki S, Kubo M, Inoue A, Miyake Y, Oshiro H. Jejunal small ectopic pancreas developing into jejunojejunal intussusception: a rare cause of ileus. World J Gastroenterol. 2009;15:3954-3956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Deesomsak M, Aswakul P, Junyangdikul P, Prachayakul V. Rare adult gastric duplication cyst mimicking a gastrointestinal stromal tumor. World J Gastroenterol. 2013;19:8445-8448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | von Heinrich H. Ein Beitrag zur Histologie des sogen: Akzessorischen Pankreas. Virchows Arch A Pathol Anat Histopathol. 1909;198:392-401. [RCA] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 33] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Ogino H, Ochiai T, Nakamura N, Yoshimura D, Kabemura T, Kusumoto T, Matsuura H, Nakashima A, Honda K, Nakamura K. Duplication cyst of the small intestine found by double-balloon endoscopy: a case report. World J Gastroenterol. 2008;14:3924-3926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Scatizzi M, Calistri M, Feroci F, Girardi LR, Moraldi L, Rubio CA, Moretti R, Nesi G. Gastric duplication cyst in an adult: case report. In Vivo. 2000;19:975-978. [PubMed] |
| 6. | Curci MR, Compton CC. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 8-2000. An 8 1/2 year-old girl with a painful abdominal mass. N Engl J Med. 2000;342:801-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Sharma S, Yadav AK, Mandal AK, Zaheer S, Yadav DK, Samie A. Enteric Duplication Cysts in Children: A Clinicopathological Dilemma. J Clin Diagn Res. 2015;9:EC08-EC11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Stringer MD, Spitz L, Abel R, Kiely E, Drake DP, Agrawal M, Stark Y, Brereton RJ. Management of alimentary tract duplication in children. Br J Surg. 1995;82:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 107] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Oyama Valenzuela E. [Obstruction of the jejunum by a chyliferous cyst of the mesentery]. Rev Med Chil. 1950;78:280-281. [PubMed] |
| 10. | van der Hal I, Mooy GS. [Intra-abdominal and intrathoracic macrodiverticulum of the jejunum of gastrogenic origin; relation to mediastinal gastrogenic cysts]. Ned Tijdschr Geneeskd. 1950;94:2533-2538. [PubMed] |