Published online Aug 16, 2016. doi: 10.12998/wjcc.v4.i8.229
Peer-review started: March 29, 2016
First decision: May 16, 2016
Revised: May 26, 2016
Accepted: June 1, 2016
Article in press: June 3, 2016
Published online: August 16, 2016
Processing time: 136 Days and 23.5 Hours
This case report describes an extraordinary case of the spontaneous transmaxillary-transnasal discharge of a dental implant, which occurred during a sneeze. The patient was complained of symptoms of acute sinusitis. She underwent a computed tomography scan that revealed a dental implant dislocated in the maxillary sinus. Medical treatment based on antibiotics and mucolytics was administered to the patient in order to prepare her for endoscopic endonasal surgery. The implant was spontaneously discharged two days after during a sneeze. Mucociliary clearance in combination with a local osteolytic inflammatory process and mucolytics therapy are the likely causes of this unusual discharge.
Core tip: Iatrogenic dislocation of dental implants into paranasal sinuses is not a rare pathological finding. Dental implants dislocation are commonly related to a wrong operating procedure or diagnostic clinical planning. Functional endoscopic sinus surgery has been widely described as the first option to remove foreign bodies from the paranasal sinuses, while the Caldwell-Luc approach to the maxillary sinuses still represents an option if the patients wants to avoid general anesthesia. Up-today just one case of spontaneous nasal discharge was reported in the literature. Therefore this case report describes a really uncommon clinical finding.
- Citation: Procacci P, De Santis D, Bertossi D, Albanese M, Plotegher C, Zanette G, Pardo A, Nocini PF. Extraordinary sneeze: Spontaneous transmaxillary-transnasal discharge of a migrated dental implant. World J Clin Cases 2016; 4(8): 229-232
- URL: https://www.wjgnet.com/2307-8960/full/v4/i8/229.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i8.229
Implant-supported prosthetic rehabilitation represents one of the most common procedures in dental clinical practice[1]. In surgical dental treatment that includes the posterior maxillary region, such as implant placement or impacted third molar extraction, the maxillary sinus should be taken into account because of its anatomical position[2,3]. Implant displacement into paranasal sinuses has been reported frequently in the literature[4-9]. According to the associated complications (implant displacement, implant displacement with or without reactive sinusitis and/or with or without associated oro-antral communication), such approaches as functional endoscopic sinused surgery (FESS), intraoral approach to the sinus, or FESS associated with an intraoral approach could be considered[10]. To the authors’ knowledge, this is the second report of a migrated dental implant spontaneous transnasal-transmaxillary discharge[11].
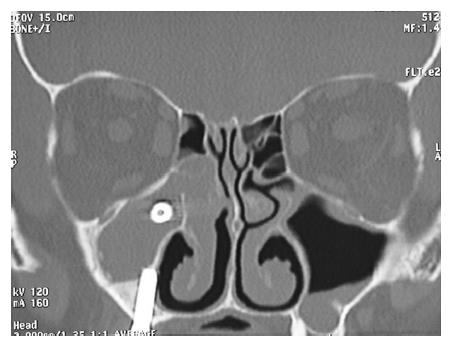
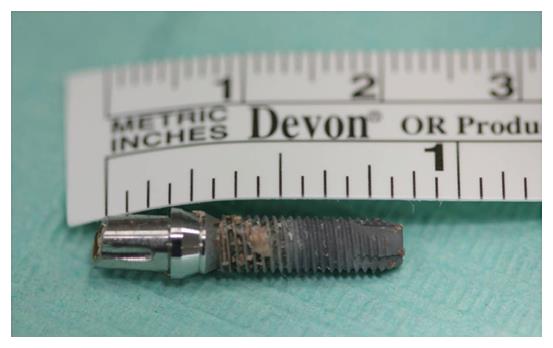
A 63-year-old woman was referred to our Department complaining of pain in the right cheek, malar rubor and edema, fever and nasal purulent discharge. Symptoms and signs appeared one week before her first visit. When the patient visited her private dentist with those symptoms, he promptly performed a radiological examination. The panoramic radiography revealed that an endosseous dental implant previously located at the posterior aspect of the right upper maxillary alveolar ridge had disappeared (Figure 1). On her arrival in our department, the patient immediately underwent a computed tomography scan which revealed that the dental implant was located inside the right maxillary sinus. The anterior aspect of the implant was completely inside the maxillary sinus while the posterior part was positioned throughout the osteomeatal complex. A massive right odontogenic sinusitis with ethmoid involvement was noticed (Figures 2 and 3). The clinical examination did not show any kind of oroantral communication at the superior aspect of the right maxillary ridge and the implant-supported prosthesis was stable without evidence of any kind of pathological signs. An endoscopic endonasal removal of the implant was then planned. A preoperative medical treatment [Ciprofloxacin (500 mg) and Acetylcysteine (600 mg)] twice a day for 7 d was administered in order to prepare her for surgery. Unexpectedly, 2 d after she reported that she had discharged the dental implant in the early morning during a sneeze (Figure 4). No bleeding took place. Surgery was then cancelled and the patient completed her medical treatment. Signs and symptoms disappeared without any kind of late complications within 7 d.
Foreign body dislocation in the paranasal sinuses is a common event[12-14]. The presence of a foreign body inside a paranasal sinus often causes an acute inflammatory reaction of the Schneider membrane with a possible consequent obstruction of the sinus ostium. The occlusion of the osteomeatal complex and the edema of the sinusal membrane could lead to a severe alteration of the mucociliary function and, as a direct complication, an acute or recurrent sinusitis[15]. When foreign body displacement occurs, it has to be removed in order to avoid sinus pathology[10,12]. Although several different approaches to remove a foreign body from the maxillary sinus have been described, all of those should be associated with preoperative and postoperative antibiotic, mucolytics and corticosteroid treatment. The first aim of the medical therapy is to reduce the edema of the sinonasal mucosa and to limit the infection.
In the present case the patient underwent preoperative medical therapy that probably stimulated the reactivation of the mucociliary function of the maxillary sinus with a consequent dislocation of the migrated dental implant from the maxillary sinus to the osteomeatal complex. The dental implant then acted like a trigger causing subsequent multiple sneezing and the final extraordinary transnasal discharge of the foreign body.
The paper describes an extraordinary case of an ectopic implant spontaneously discharged during a sneeze.
The case describes an acute maxillary sinusitis due to a dislocated dental implants into maxillary sinus.
Maxillary sinusitis vs rhinosinusitis.
Computed tomography scans clearly describe the position of the ectopic implant located between the maxillary ostium and the medial meatus.
Malar rubor and malar oedema associated with severe nasal discharge and nasal dripping allowed to make diagnosis of acute maxillary sinusitis.
The patients was candidated to functional endoscopic sinuses surgery in order to remove the foreign body but immediately before the surgical procedure she discharge the ectopic dental implant.
Please provide other contents related to the case report to help readers better understand the present case.
To the authors’ knowledge, this is the second report of a migrated dental implant spontaneous transnasal-transmaxillary discharge.
The present case showed clearly how competent could be the mucociliary clearance and helps to understand that the combined antibiotic and mucolytic therapy is always advisable before surgery.
This case report describes an extraordinary case of the spontaneous transmaxillary-transnasal discharge of a dental implant. The implant was spontaneously discharged 2 d after during a sneeze. It is interesting and meaningfull.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gürel P, Liang ZQ S- Editor: Ji FF L- Editor: A E- Editor: Zhang FF
| 1. | Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132. [PubMed] |
| 2. | Grandini SA, Barros VM, Salata LA, Rosa AL, Soares UN. Complications in exodontia--accidental dislodgment to adjacent anatomical areas. Braz Dent J. 1993;3:103-112. [PubMed] |
| 3. | Nocini PF, De Santis D, Morandini B, Procacci P. A dental implant in the infratemporal fossa: case report. Int J Oral Maxillofac Implants. 2013;28:e195-e197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | González-García A, González-García J, Diniz-Freitas M, García-García A, Bullón P. Accidental displacement and migration of endosseous implants into adjacent craniofacial structures: a review and update. Med Oral Patol Oral Cir Bucal. 2012;17:e769-e774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Connolly AA, White P. How I do it: transantral endoscopic removal of maxillary sinus foreign body. J Otolaryngol. 1995;24:73-74. [PubMed] |
| 6. | Galindo P, Sánchez-Fernández E, Avila G, Cutando A, Fernandez JE. Migration of implants into the maxillary sinus: two clinical cases. Int J Oral Maxillofac Implants. 2005;20:291-295. [PubMed] |
| 7. | Kitamura A. Removal of a migrated dental implant from a maxillary sinus by transnasal endoscopy. Br J Oral Maxillofac Surg. 2007;45:410-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Haben CM, Balys R, Frenkiel S. Dental implant migration into the ethmoid sinus. J Otolaryngol. 2003;32:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Felisati G, Lozza P, Chiapasco M, Borloni R. Endoscopic removal of an unusual foreign body in the sphenoid sinus: an oral implant. Clin Oral Implants Res. 2007;18:776-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Chiapasco M, Felisati G, Maccari A, Borloni R, Gatti F, Di Leo F. The management of complications following displacement of oral implants in the paranasal sinuses: a multicenter clinical report and proposed treatment protocols. Int J Oral Maxillofac Surg. 2009;38:1273-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | van de Loo S, Kessler P, Lethaus B. Spontaneous transmaxillary-transnasal implant loss: a case report. Implant Dent. 2013;22:117-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Sgaramella N, Tartaro G, D’Amato S, Santagata M, Colella G. Displacement of Dental Implants Into the Maxillary Sinus: A Retrospective Study of Twenty-One Patients. Clin Implant Dent Relat Res. 2016;18:62-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Kharel Sitaula R, Gautam V, Kc K, Shah DN. Impacted iron nail in the orbit and maxillary sinus through a corneo-scleral perforation: a case report. Nepal J Ophthalmol. 2013;5:268-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Sahin YF, Muderris T, Bercin S, Sevil E, Kırıs M. Chronic maxillary sinusitis associated with an unusual foreign body: a case report. Case Rep Otolaryngol. 2012;2012:903714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Feng L, Li H, E LL, Li CJ, Ding Y. Pathological changes in the maxillary sinus mucosae of patients with recurrent odontogenic maxillary sinusitis. Pak J Med Sci. 2014;30:972-975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |