Published online Oct 16, 2016. doi: 10.12998/wjcc.v4.i10.333
Peer-review started: February 27, 2016
First decision: March 24, 2016
Revised: August 2, 2016
Accepted: August 17, 2016
Article in press: August 18, 2016
Published online: October 16, 2016
Atypical fibroxanthoma (AFX) is a spindle cell neoplasm with low metastatic potential but high tendency to recur after surgery. Because of the rarity of this lesion and its aspecific clinical features, AFX could be easily misdiagnosed and undertreated by many clinicians who encounter them. Dermoscopy represents a valuable tool for easily assessing skin lesions, even though histological examination is required for final diagnosis. We report a case of a cheek lesion with dermoscopic “blue amber pattern”, easily recognisable and not observed in others skin tumours, which could represent an additional feature useful in differentiating this tumour from other skin neoplasms.
Core tip: Until recent years there has been little published literature about the dermatoscopy of atypical fibroxanthoma (AFX). A case of AFX is presented. Dermatoscopy could be helpful in avoiding a misdiagnosis and undertreatment of this tumour.
- Citation: Pagliarello C, Peccerillo F, Zucchi A, Tortorella RG, Ricci R, Stanganelli I, Feliciani C, Di Nuzzo S. Lesion presenting with a “blue amber” pattern. World J Clin Cases 2016; 4(10): 333-335
- URL: https://www.wjgnet.com/2307-8960/full/v4/i10/333.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i10.333
Atypical fibroxanthoma (AFX) is an uncommon, locally aggressive malignant fibrohistiocytic tumour with a tendency for recurrence and a low metastatic potential[1]. Exposure to ultraviolet light represents a risk factor for its development. AFX is usually described as a solitary red or pink papule or extensively ulcerated nodule on the head or neck; nevertheless, early cases could be easily undiagnosed or misdiagnosed. Complete tumour excision could be critical in avoiding local recurrence[1]. Although the rarity of this neoplasm explains its low clinical suspicion, the absence of characteristic features contributes to the delay in diagnosis that it is usually reached through histopathological examination. Dermoscopy has proven to be a useful diagnostic tool in other cutaneous malignancies[2,3], but the unique published report concerning AFX shows that its dermoscopic features are non-contributory and nonspecific[4]. The correct preoperative diagnosis is therefore rarely made. Undertreatment usually will result in recurrence, since the recurrence rate for AFX is high even for cases treated appropriately and in a timely manner.
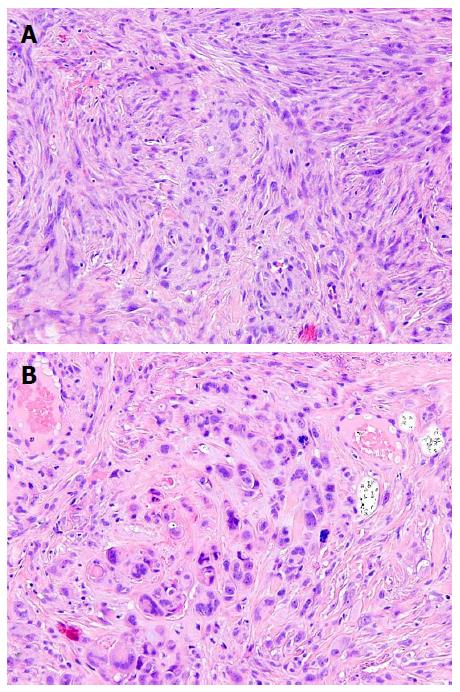
We present the case of a 69-year-old female with a history of hypertension and occupational sun exposure. She was referred to our clinic for evaluation of an asymptomatic, rapidly growing violaceous nodule on her cheek that appeared 8 wk earlier (Figure 1A). The lesion was previously diagnosed twice as a basal cell carcinoma and accordingly treated with imiquimod and cryotherapy, but it recurred. Using dermoscopy, we observed on the right side of the lesion some irregular, linear vessels over a whitish veil. On the left side, however, we noticed a “blue amber” pattern consisting of bluish, homogeneous pigmentation surrounded by a purple halo with scattered yellowish inclusions (Figure 1B and inset). The plaque was excised, and histological examination showed an intradermal tumour with no epidermal involvement, made up of a mixture of spindle-shaped cells, histiocytelike cells, xanthomatous cells, and multinucleated giant cells with marked pleomorphism, hypercromasia, and prominent mitotic activity (Figure 2). A diagnosis of AFX was made.
The correct diagnosis of AFX is difficult because of its rarity, so skin biopsy for obtaining histological examination is usually necessary. A handful of cases has been reported in the literature about dermoscopy of AFX. Bugatti et al[4] described these lesions as “slightly pigmented, reddish, malignant cutaneous tumours displaying prominent and chaotic dermatoscopic neoangiogenetic features in more advanced stages of proliferation”. Lallas et al[5] described AFX as “typified by reddish and whitish areas in combination with polymorphous vascular pattern with various combinations of linear, dotted, hairpin and highly tortuous vessel irregularly distributed over the surface of the lesion”. Pitarch et al[6] recognised in AFX “shiny whitish areas between the rainbow-patterned structures and scales visible on surface”. Until recent years there has been little published literature about the dermatoscopy of AFX, and published reports suggest that dermoscopic features are quite non-specific and depend on the stage of the lesion. Therefore, as stated elsewhere, is highly recommended the excision of any skin lesion with the clinical features of elevation, firmness and growth[7] for avoiding AFX undertreatment. Although the vascular morphology of our lesion was suspicious for a malignant neoplasm, such as an adnexal tumour or amelanotic melanoma, the blue amber pattern, to our knowledge, had not been previously reported. The anatomical counterparts of this pattern are possibly represented by haemorrhagic areas in the periphery of the lesion, while xanthomatised cells could explain the yellow inclusions. The blue amber pattern is easily recognisable and is not observed in other skin tumours; it could represent an additional feature in the differential diagnosis between AFX and other skin neoplasms such as basal cell carcinoma, prompting a histological examination. We provide an easy-to-recognise dermoscopic pattern in a histologically proven case of AFX. Dermatologists should be aware of this pattern to avoid undertreating this neoplasm.
A 69-year-old female with a history of hypertension and occupational sun exposure with a nontender nodule on her cheek of eight weeks’ duration.
Rapidly growing violaceous nodule on cheek.
Basal cell carcinoma, merckel cell carcinoma.
All labs were within normal limits.
Atypical fibroxanthoma (AFX).
Complete surgical excision of lesion.
AFX and solid neoplasm presenting as a solitary red or pink papule or extensively ulcerated nodule on the head or neck.
AFX: A locally aggressive malignant fibrohistiocytic tumour with a tendency for recurrence and a low metastatic potential.
This entity is commonly undiagnosed or misdiagnosed. Dermoscopy have the potential for avoiding undertreatment of this tumour.
This is a nice case report illustrating an easily recognizable dermoscopic pattern (“blue amber pattern”) which could represent an additional feature in differential diagnosis between Atypical fibroxanthoma and other skin neoplasms.
Manuscript source: Invited manuscript
Specialty Type: Medicine, research and experimental
Country of Origin: Italy
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Gonzalez-Lopez MA, Kaliyadan F S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Iorizzo LJ, Brown MD. Atypical fibroxanthoma: a review of the literature. Dermatol Surg. 2011;37:146-157. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part II. Nonmelanocytic skin tumors. J Am Acad Dermatol. 2010;63:377-386; quiz 387-388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 168] [Cited by in F6Publishing: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 3. | Argenziano G, Zalaudek I, Corona R, Sera F, Cicale L, Petrillo G, Ruocco E, Hofmann-Wellenhof R, Soyer HP. Vascular structures in skin tumors: a dermoscopy study. Arch Dermatol. 2004;140:1485-1489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 203] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 4. | Bugatti L, Filosa G. Dermatoscopic features of cutaneous atypical fibroxanthoma: three cases. Clin Exp Dermatol. 2009;34:e898-e900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Lallas A, Moscarella E, Argenziano G, Longo C, Apalla Z, Ferrara G, Piana S, Rosato S, Zalaudek I. Dermoscopy of uncommon skin tumours. Australas J Dermatol. 2014;55:53-62. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Pitarch G. Patrón dermatoscópico en arcoíris en fibroxantoma atípico. Dermoscopic rainbow pattern in atypical fibroxanthoma. Actas Dermosifiliogr. 2014;105:97-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Inskip M, Magee J, Weedon D, Rosendahl C. Atypical fibroxanthoma of the cheek-case report with dermatoscopy and dermatopathology. Dermatol Pract Concept. 2014;4:77-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |