Published online Sep 16, 2014. doi: 10.12998/wjcc.v2.i9.478
Revised: June 10, 2014
Accepted: June 27, 2014
Published online: September 16, 2014
Processing time: 159 Days and 14.1 Hours
As per strict criteria of Das Gupta et al, primary splenic lymphoma is very rare. Herein, we are reporting an unusual case of primary large cell splenic lymphoma of B lineage in a middle aged female presenting with massive splenomegaly (3.8 kg) and hypersplenism. After performing therapeutic splenectomy for hypersplenism, a precise diagnosis of diffuse large B cell lymphoma was made on histopathology and confirmed by immunohistochemistry. The patient responded well to standard (Cyclophosphamide, Hydroxydaunorubicin, Oncovin (vincristine), Prednisone or prednisolone) regimen last year and is now in full remission. The splenectomy thereby has prevented the potential grave complications related to hypersplenism and splenic rupture. Our aim behind highlighting the topic is to specify that emergency splenectomy followed by anticoagulation therapy is an effective plan of management to prevent untoward complications related to disease and treatment.
Core tip: Primary splenic lymphoma is a rare entity, can present with grave complications like hypersplenism and splenic rupture. In such circumstances, emergency splenectomy is an effective therapeutic and diagnostic tool. Now a days laparoscopic splenectomy is emerging because of minimal complications. Postoperative anticoagulation is important to prevent portal splenic vein thrombosis.
- Citation: Ingle SB, Ingle CRH. Splenic lymphoma with massive splenomegaly: Case report with review of literature. World J Clin Cases 2014; 2(9): 478-481
- URL: https://www.wjgnet.com/2307-8960/full/v2/i9/478.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i9.478
Primary splenic lymphoma is a very unusual entity if strict diagnostic criteria proposed by Das Gupta et al[1] are applied. According to their views diagnosis of Primary Splenic Lymphoma should be made when the disease is confined to spleen or at the most involves hilar lymph nodes with no recurrence of disease after splenectomy[1,2]. Herein, we present such an unusual case of Primary Splenic Lymphoma of diffuse large B cell type diagnosed on histopathology and confirmed by immunohistochemistry in a patient presenting with massive splenomegaly and hypersplenism. Splenectomy was followed by anticoagulation therapy and chemotherapy [with standard Cyclophosphamide, Hydroxydaunorubicin, Oncovin (vincristine), Prednisone or prednisolone (CHOP) regimen]. The patient responded well and as on today, is in complete remission preventing grave complications of disease and splenectomy thus justifying both diagnostic and therapeutic utility of splenectomy and effective anticoagulation therapy is must to prevent portal vein splenic vein thrombosis(PVST).
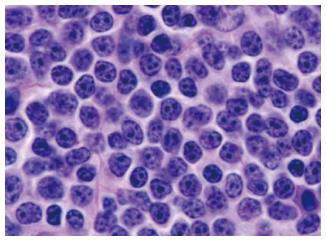
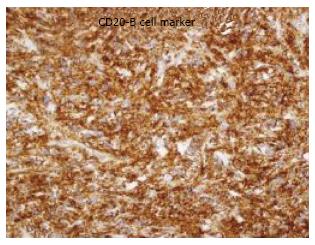
A 41-year-old female, complained of weight loss and abdominal pain. She was afebrile and physical examination revealed no palpable peripheral lymphadenopathy. Head and neck examination revealed moderate anemia, no jaundice and a clear oropharynx. Heart and lung examination were normal. She had a protuberant abdomen with a firm palpable spleen that extended below the navel. There was no ascites or hepatomegaly. Abdominal ultrasonography and plain computed tomography scanning showed massive splenomegaly without a mass lesion (Figure 1). Blood examination revealed pancytopenia: WBC 1.9 × 109/L (neutrophils 48.0%, eosinophils 0%, basophils 0%, monocytes 4.0%, lymphocytes 48.0%), Hb 10.3 g/dL, platelet count 99 × 109/L, LDH 127 U/L (normal range 100-220 U/L). Air-dried peripheral blood smear showed no abnormal lymphocytes including hairy cells or villous lymphocytes. Liver and renal functions were within normal limits. Bone marrow aspiration and biopsy revealed normocellular bone marrow without abnormal cell involvement, fibrosis, dysplasia or hemophagocytosis. Liver cirrhosis and idiopathic portal hypertension were ruled out. Whole body computed tomography (CT) scanning revealed no abnormal lesions in other organs. Therefore, emergency splenectomy was planned and performed. The operation progressed without complications. The resected spleen weighed 3.8 kg. The cut surface was almost totally effaced by a huge greywhite homogenous tumor soft rubbery in consistency (Figures 2 and 3) Microscopy revealed diffuse proliferation of monotonous population of large neoplastic lymphoid cells [Large B cell lymphoma (DLBCL)] (Figure 4) , The tumor cells were immunopositive for CD 20 and immunonegative for T cell markers (Figure 5). Intraoperative findings did not reveal any lymph node swelling or tumor. Therefore, the patient was diagnosed as stage I splenic lymphoma. Four days after the operation, the patient recovered from the pancytopenia: WBC of 7.6 × 109/L, Hb 13.0 g/dL and platelet count 330 × 109/L although CRP increased to 8.21 mg/dL owing to postoperative infection. 24 h after surgery, received subcutaneous injection of LMWH (Low Molecular Weight Heparin) routinely, 0.3 mL per 12 h for 5 d and then maintained by oral therapy with warfarin for one month to keep the target prothrombin time/international normalized ratio (PT/INR) at a level between 1.25 and 1.5 to prevent PSVT.
Three courses of standard CHOP plus rituximab chemotherapy were given. Complete remission has continued for 12 mo post operatively without any grave complications related to disease and splenectomy. Thus, the case was finally confirmed as primary splenic lymphoma of B cell lineage as per the strict criteria of Das Gupta et al[1].
Primary lymphoma of the spleen is very rare if strict criteria for diagnosis suggested by Das Gupta et al[1] are applied[2].
Solitary splenic non Hodgkin Lymphoma (NHL) is rare; the incidence is less than 1%[3]. Some solitary lymphomas cannot be discerned by plain CT scanning alone or US alone. Consequently, enhanced CT scanning and Gallium scintigraphy are absolutely required to identify splenic tumor. Splenectomy is often chosen to diagnose solitary splenic lymphoma.
However, several previous reports discussed the risk of splenectomy for massive (greater than 1500 gm) splenomegaly. Splenectomy for massive splenomegaly showed a high rate of perioperative mortality (about 20%[4,5]. In some cases with poor general status, bleeding tendency, complications due to infection or organ failure, one should be hesitant to use an invasive diagnostic method. On the other hand, splenic needle biopsy may provide an adequate diagnosis without severe complications. Tam et al[6] reported percutaneous image guided splenic needle biopsy in 156 consecutive cases and concluded that splenic needle biopsy in the evaluation of new or recurrent neoplasm is a minimally invasive procedure with low complication rates and a high diagnostic yield. If it is institutionally and technically possible, splenic needle biopsy should be taken into consideration for high risk patients[6]. Recently, laparoscopic splenectomy has often been used for splenic masses because of fewer complications and since it is rather appropriate for moderate splenomegaly[7,8].
This patient underwent splenectomy because she had no complications. Splenectomy was done to: (1) establish a correct pathological diagnosis; (2) reduce the hypersplenism; (3) reduce the radiation field; (4) relieving symptoms; and (5) prevent splenic rupture and prevented PSVT with effective anticoagulant therapy
Generally speaking,the localized indolent lymphoma is expected to have good prognosis despite the absence of further treatment with chemotherapy. In contrast, most cases of aggressive lymphoma such as DLBCLs show disease expansion and progression, requiring immediate chemotherapy. It is speculated that the high rate of perioperative mortality in massive splenomegaly could be due to rapid progression of disease and such patients should be subjected to less invasive diagnostic methods and treated immediately.
Splenic lymphoma and splenomegaly secondary to lymphoma or other hematological malignancies are often reported as a cause of hypersplenism and the cytopenias resolved after splenectomy in most cases[4,9]. Therefore ,splenectomy is useful not only for diagnosis but also for treatment of the underlying hematologic malignancy.
It is an unusual case of primary splenic lymphoma presenting with massive splenomegaly (3.8 kg) and hypersplenism. In such a critical clinical situation, clinician should keep in mind splenectomy supported by anticoagulation therapy as an effective therapeutic and diagnostic method to prevent grave complications related to disease (hypersplenism, splenic rupture) and splenectomy, i.e., PSVT that could prove fatal. Recently splenic needle biopsy can be used to diagnose the condition earlier.
Massive splenomegaly, hypersplenism.
Primary splenic lymphoma presenting with huge splenic mass and hypersplenism.
Causes of hypersplenism, lymphoma, leukemia, Malaria, Kala azar.
Hypersplenism presenting with thrombocytopenia.
Computed tomography scan revealing massive splenomegaly without mass lesion.
Biopsy findings are confirmatory for diffuse large B cell lymphoma.
Emergency splenectomy is an effective therapeutic and diagnostic tool in such critical circumstances.
This manuscript is very interesting.
P- Reviewer: Yoshida H S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Das Gupta T, Goombes B, Brosfeld RD. Primary malignant neoplasms of the spleen. Surg Gynecol Obstet. 1969;120:947-60. |
| 2. | Cavanna L, Artioli F, Vallisa D, Di Donato C, Bertè R, Carapezzi C, Foroni R, Del Vecchio C, Lo Monaco B, Prati R. Primary lymphoma of the spleen. Report of a case with diagnosis by fine-needle guided biopsy. Haematologica. 1995;80:241-243. [PubMed] |
| 3. | Brox A, Shustik C. Non-Hodgkin’s lymphoma of the spleen. Leuk Lymphoma. 1993;11:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Han B, Yang Z, Yang T, Gao W, Sang X, Zhao Y, Shen T. Diagnostic splenectomy in patients with fever of unknown origin and splenomegaly. Acta Haematol. 2008;119:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Danforth DN, Fraker DL. Splenectomy for the massively enlarged spleen. Am Surg. 1991;57:108-113. [PubMed] |
| 6. | Tam A, Krishnamurthy S, Pillsbury EP, Ensor JE, Gupta S, Murthy R, Ahrar K, Wallace MJ, Hicks ME, Madoff DC. Percutaneous image-guided splenic biopsy in the oncology patient: an audit of 156 consecutive cases. J Vasc Interv Radiol. 2008;19:80-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Tessier DJ, Pierce RA, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Czerniejewski S, Matthews BD. Laparoscopic splenectomy for splenic masses. Surg Endosc. 2008;22:2062-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Shimizu I, Ichikawa N, Yotsumoto M, Sumi M, Ueno M, Kobayashi H. Asian variant of intravascular lymphoma: aspects of diagnosis and the role of rituximab. Intern Med. 2007;46:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Pottakkat B, Kashyap R, Kumar A, Sikora SS, Saxena R, Kapoor VK. Redefining the role of splenectomy in patients with idiopathic splenomegaly. ANZ J Surg. 2006;76:679-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |