Published online May 16, 2014. doi: 10.12998/wjcc.v2.i5.137
Revised: February 16, 2014
Accepted: March 11, 2014
Published online: May 16, 2014
AIM: To systematically review the literature on the efficacy of noninvasive methods of arresting the progression of non-cavitated occlusal carious lesions in dentin.
METHODS: The Medline/PubMed, LILACS, SciELO and Scopus databases were searched to identify relevant publications through to November 2013. Only clinical trials evaluating the ability of noninvasive methods to arrest the progression of occlusal non-cavitated carious lesions in dentin were included. Screening, data extraction and quality assessment were conducted independently and in duplicate.
RESULTS: Of 167 citations identified, nine full text articles were screened and five were included in the analysis. All papers reported on occlusal fissure sealing using a self-curing glass ionomer (n = 1) or resin-based (n = 4) sealant. Only the use of resin-based sealant to obliterate occlusal fissures arrested the progression of non-cavitated occlusal carious lesions in dentin.
CONCLUSION: Occlusal fissure sealing with a resin-based sealant may arrest the progression of non-cavitated occlusal dentinal caries. Further clinical trials with longer follow-up times should be performed to increase scientific evidence.
Core tip: Occlusal fissure sealing with a resin-based sealant may arrest the progression of non-cavitated occlusal dentinal caries.
- Citation: Assunção IV, Costa GFAD, Borges BCD. Systematic review of noninvasive treatments to arrest dentin non-cavitated caries lesions. World J Clin Cases 2014; 2(5): 137-141
- URL: https://www.wjgnet.com/2307-8960/full/v2/i5/137.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i5.137
Pit and fissure sealing is a noninvasive approach that has been used since the 1960s to prevent occlusal caries by providing a physical barrier that inhibits the accumulation of microorganisms and food particles. The efficacy and clinical safety of this preventive approach have been well established[1,2].
In restorative dentistry, the treatment of carious lesions has been reviewed many times. Minimally invasive dentistry, the goal of which is to preserve the greatest amount possible of tooth structure, is intended to replace conventional procedures[1]. When an open cavity is diagnosed, the option of restoration tends to be unquestionable. However, it should be noted that caries involving dentine may be present in non-cavitated lesions and that there may be a layer of intact enamel[2].
The use of pit and fissure sealant to seal fissures has been investigated as a secondary preventive approach to the management of non-cavitated occlusal carious lesions in dentin since it arrested their progression[3-7]. This noninvasive method may replace the traditional restorative approach as it can be performed with a shorter chair time in the absence of anesthesia. Moreover, it can conserve tooth structure by delaying intervention or minimizing the operative procedure[8]. Although several clinical trials have examined this use of pit and fissure sealants, a systematic analysis of their results is needed to provide scientific evidence for its effectiveness as a secondary preventive approach. Thus, we systematically reviewed the literature on the efficacy of noninvasive methods in arresting the progression of non-cavitated occlusal carious lesions in dentin.
The focused question addressed in this review was: “Can noninvasive treatments arrest the progression of non-cavitated occlusal carious lesions in dentin?”.
The Medline/PubMed, LILACS, SciELO and Scopus databases were searched to identify relevant studies published through to November 2013. The search strategy employed the following keywords related to the intervention method, type of carious lesion and outcome.
Intervention:“Sealing” or “fissure sealing” or “sealant” or “glass ionomer cement” or “nonoperative” or “non-operative” or “noninvasive” or “non-invasive” or “nonsurgical” or “non-surgical”.
Type of caries lesion: [(“dentin” or “dentinal”) and “caries”] and (“occlusal” or “pit and fissure” or “pits and fissures”) and (“non-cavitated” or “noncavitated”).
Outcome:“Progression” or “regression” or “arrest” or “arrested” or “arrestment” or “arresting”.
The selection was limited to clinical trials published in English that evaluated the efficacy of any noninvasive approach in treating non-cavitated occlusal carious lesions in dentin. Review articles, in vitro studies and those reporting only on proximal carious lesions or those in enamel were excluded. Studies that evaluated cavitated lesions were also excluded.
Two independent reviewers (Assunção IV and Costa GF) selected studies using a two stage screening process. In the first stage, titles and abstracts were screened to eliminate irrelevant articles and those that did not meet the inclusion criteria. In the second stage, the reviewers independently verified study eligibility after reading full texts and data extraction and quality assessment were performed for included studies. Disagreements about the inclusion or exclusion of a study were resolved by consensus and, when necessary, consultation with a third reviewer (Borges BCD). In the analysis of these included studies, the following questions were addressed: (1) Does pit and fissure sealing effectively arrest the progression of non-cavitated occlusal carious lesions in dentin?; (2) Is the noninvasive treatment of non-cavitated occlusal carious lesions in dentin effective in permanent and deciduous teeth?; and (3) Which materials should clinicians use to seal pits and fissures in the management of non-cavitated occlusal carious lesions in dentin? What are the perspectives on the use of alternative sealing materials and techniques?
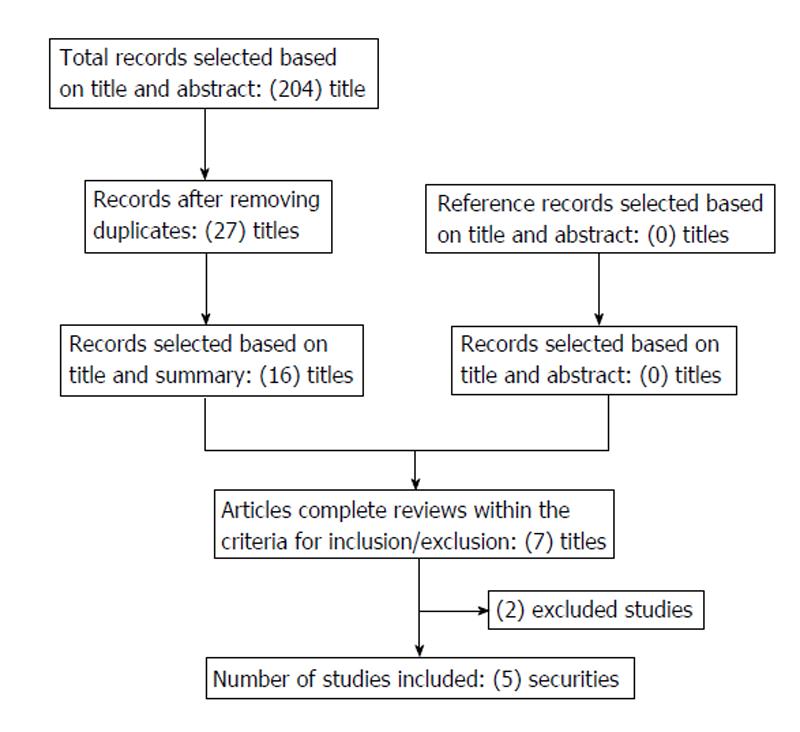
The initial search identified 204 articles (156 articles in Medline/PubMed, 22 articles in LILACS, 8 articles in SciELO and 18 articles in Scopus). Thirty-seven duplicate publications were excluded, leaving 167 potentially eligible articles. First stage screening of titles and abstracts identified nine articles that were qualified for full text screening. The second stage of screening identified five articles that met the inclusion criteria (two studies evaluating cavitated lesions, one article reporting on an invasive treatment and one review article were excluded) (Figure 1).
The content of selected studies is summarized in Table 1.
| Author/yr | Study design | Sample characteristics | Analyzed variables and evaluation methods | Tested treatments | Follow up | Results/conclusions |
| Borges et al[3] (2010) | Randomized controlled clinical trial | Sixty permanent molars in 35 individuals (12–19.5 years old) with non-cavitated carious lesions radiographically located between the dentin-enamel junction and middle third of dentin | Caries progression and sealant loss; clinical and radiographic examinations | Experimental (n = 30): oral hygiene instruction and fissure sealing (Fluorshield, Dentsply); control (n = 30): oral hygiene instruction | 4-mo intervals for 1 year; control group was followed for only 8 mo due to signals of caries progression | Eight teeth (four per group) were lost at 1-year follow up. Clinical and radiographic caries progression was significantly more frequent in control than in experimental teeth. Sealant loss occurred in three cases and resulted in caries progression. Pit and fissure sealant effectively arrested caries progression, suggesting that this intervention may replace traditional invasive treatment of non-cavitated dentinal caries |
| Borges et al[4] (2012) | Randomized controlled clinical trial | Sixty permanent molars in 35 individuals (12-19.5 years old) with non-cavitated carious lesions radiographically located between the dentin-enamel junction and middle third of dentin | Caries progression and sealant loss; clinical and radiographic examinations | Experimental (n = 30): oral hygiene instruction and fissure sealing (Fluorshield, Dentsply); control (n = 30): oral hygiene instruction | 4-mo intervals for 1 year, then 12-mo intervals to 36 mo; control group was followed for only 8 mo due to signals of caries progression | Eight teeth (four per group) were lost at 1-year follow up; no tooth was lost subsequently. Clinical and radiographic caries progression was significantly more frequent in the control than in the experimental group. Three teeth lost sealant and showed caries progression at the 12-mo follow up. No sealant loss or caries progression was observed at 24 or 36 mo. Pit and fissure sealant effectively arrested carious lesions for a 36-mo period |
| Borges et al[5] (2012) | Randomized controlled split-mouth clinical trial | Sixty deciduous molars in 30 schoolchildren (5-9 years old) with non-cavitated carious lesions radiographically located between the dentin-enamel junction and middle third of dentin | Experimental group: caries progression and sealant loss; control group: secondary caries emergence and clinical failure of composite restorations | Experimental (n = 30): fissure sealing (Fluorshield, Dentsply); control (n = 30): composite restoration (Ice, SDI) | 4-mo intervals for 1 year | No tooth was lost to follow up. The treatment modalities were similarly effective in managing non-cavitated occlusal carious lesions in dentin of primary molars. Three teeth showed partial sealant retention and caries progression after 1 year. The invasive approach can be replaced with non-drilling fissure sealing techniques for the management of these lesions |
| da Silveira et al[6] (2012) | Randomized controlled clinical trial | Fifty-one permanent molars in 38 individuals (± 12.78 years old) with non-cavitated carious lesions radiographically located between the dentin-enamel junction and middle third of dentin | Caries progression and sealant loss; clinical and radiographic examinations | Experimental (n = 27): oral hygiene instruction and sealing with self-curing glass ionomer cement (Vidrion-R, SS White) | 4-mo intervals for 1 year; control group was followed for only 8 mo due to signals of caries progression | No tooth was lost to follow up. Clinical examination showed no significant difference between groups, but radiographic examination showed less caries progression in sealed teeth |
| Bakhshandeh et al[7] (2012) | Clinical trial | Five premolars and 67 molars in 52 individuals (± 28 years old) lesions in need of restoration. The maximum depth of the lesions, radiographically assessed, was limited to the middle third of the dentin | Experimental group: caries progression and sealant loss; control group: secondary caries emergence and clinical failure of composite restorations | Control (n = 24): oral hygiene instruction; experimental (n = 60): resin-based fissure sealing (Delton, Dentsply) Control (n = 12): composite restoration (Filtek Supreme XT, 3M ESPE) | 6-12-mo intervals for 25-38 (mean, 33) mo | Eleven sealed teeth were lost to follow up; no restored tooth was lost. All restorations and sealants functioned well; seven sealants were repaired/replaced due to failure and three sealed lesions were restored due to caries progression. Sealants arrested most (44/49) lesions; expansion of criteria for therapeutic sealing of occlusal carious lesions in adults will improve dental health |
All five studies analyzed in this review were performed on similar samples of teeth with visually non-cavitated occlusal lesions between the dentin-enamel junction and middle third of dentin. The extent of carious lesions was confirmed by bite-wing radiographic analysis. The similar samples allow precise comparison of study outcomes.
Four[3-5,7] of five studies analyzed reported that sealing arrested the progression of carious lesions when the sealant was intact and tight. These authors used only resin-based fissure sealants and analyzed caries progression by clinical and radiographic examinations. The blockade of the nutritional supply by the mechanical barrier created by the sealant seems to be the most plausible explanation for the lack of caries progression observed in those studies. Because total retention is an integral requirement for sealant success, attempts should be made to increase the mechanical strength of sealing materials and their adhesion potential to enamel.
In contrast, de Silveira et al[6] reported that a self-curing glass ionomer fissure sealant did not arrest caries progression in molars with non-cavitated occlusal dentinal lesions. Although sealed teeth showed no sign of caries progression on radiographic examination, they exhibited visible cavitation after 12 mo of follow up. The rapid macroscopic loss of self-curing glass ionomer sealant may render fissures susceptible to biofilm adhesion and further acid attack, leading to the emergence of cavitations on occlusal enamel[6].
Some points reported by Borges et al[3,4] should be emphasized. The authors commented that possible limitations of their studies included the absence of power calculation, the sample size of 60 teeth and the loss of some of the sample at 12 mo, which may have reduced the internal and external validity of these investigations. However, they argued that the remarkable difference in caries progression observed between the sealed and unsealed groups at the 12 mo recall appointments indicated that the sample size was satisfactory for the analysis and that the observation period was appropriate to detect distinct differences in outcomes. The authors further emphasized that the lack of caries progression at 12, 24 and 36 mo recall appointments in teeth with intact sealant clearly confirmed that the sample size was satisfactory.
One should consider that only papers published in the English language were included in this systematic review. In fact, the most relevant papers are published in English language since it can be read worldwide. For this reason, we believe that data loss due to the exclusion of papers wrote in other languages could not generate a negative impact to the present results.
The minimally invasive approach to carious lesions in dentistry is based on the principle that nonsurgical treatments are preferable to invasive treatments as the former increase tooth longevity. Invasive interventions initiate a cycle of treatment and re-treatment, often leading to the need for crowns and implants, regardless of the quality of the initial filling preparation[11]. Data from studies included in this review demonstrate the great positive impact of a noninvasive approach to the management of non-cavitated occlusal carious lesions in dentin. Further studies with longer follow-up times should be performed to improve the evidence provided by the present systematic review.
Borges et al[5] compared the efficacy of pit and fissure sealing using a resin-based material with that of traditional tooth restoration in the treatment of non-cavitated occlusal carious lesions in the dentin of primary molars. They concluded that the invasive restorative approach can be replaced with the fissure sealing technique that does not require drilling. Borges et al[3,4] and Bakhshandeh et al[7] reported that the same noninvasive fissure sealing treatment arrested caries in permanent molars. Thus, this approach appears to be effective in deciduous and permanent molars.
The clinical effectiveness of fissure sealing for the management of non-cavitated occlusal carious lesions in dentin depends on complete maintenance of the sealant in fissures[3-7]. The self-curing glass ionomer cement tested by de Silveira et al[6] showed high loss rates that prevented it from arresting caries progression, as determined by clinical examination. The authors observed the emergence of cavitations in enamel when the cement was lost. Resin-based fissure sealants showed higher complete retention rates, as reported by Borges et al[3-5] and Bakhshandeh et al[7]. These superior survival rates suggest that resin-based fissure sealant is preferable to self-curing glass ionomer cement.
Resin-based fissure sealants are adequate for the therapeutic sealing of non-cavitated occlusal carious lesions in dentin. However, the partial and total sealant losses observed by Borges et al[3-5] and Bakhshandeh et al[7] limit the effectiveness of this noninvasive therapeutic approach. Researchers have sought to improve sealant adhesion to enamel and/or the physical properties of polymeric networks as sealant adaptation and polymeric network strength may be related to the survival of sealants in tooth fissures[12]. Enamel conditioning with a casein phosphopeptide-amorphous calcium phosphate paste in association with adhesive system application improved the bond durability of a fissure sealant in vitro[13], suggesting that this protocol could increase sealant retention.
In vitro studies have demonstrated the superiority of flowable composites to traditional fissure sealants in terms of physical properties related to polymeric network strength, such as the degree of conversion, hardness and crosslink density[12,14-16]. Moreover, preheating of flowable composites before photoactivation has been found to increase softening resistance to acid challenge in vitro[17]. In this context, further clinical trials should be performed to evaluate the efficacy of the above described protocols in vivo.
In conclusion, noninvasive therapeutic fissure sealing is effective for the management of non-cavitated occlusal carious lesions in dentin if a resin-based fissure sealant is used. Since only relatively short-time follow-up clinical trials were found, further randomized controlled clinical trials with longer follow-up times should be performed to provide more scientific evidence for the efficacy of therapeutic sealing in the management of these lesions.
The use of pit and fissure sealant to seal fissures has been investigated as a secondary preventive approach to the management of non-cavitated occlusal carious lesions in dentin. Although several clinical trials have examined this use of pit and fissure sealants, a systematic analysis of their results is needed to provide scientific evidence for its effectiveness as a secondary preventive approach.
Cariology, restorative dentistry, preventive dentistry.
Four of five studies analyzed in this systematic review reported that sealing occlusal fissures with a resin-based sealant arrested the progression of carious lesions when the sealant was intact and tight. Occlusal fissure sealing with a resin-based sealant may arrest the progression of non-cavitated occlusal dentinal caries.
The actual restorative approach to treat non-cavitated caries lesion in dentin may be replaced with a noninvasive method. In turn, this will contribute to save sound dental tissues which are lost during cavity preparation, increasing tooth longevity.
Tooth demineralization refers to a process where an acidic environment leaches some of the mineral content (such as calcium) out of a tooth’s calcified tissues (enamel and dentin). Non invasive treatment is when there is no cavity preparation involved and healthy tooth structure is preserved.
The present manuscript is a focused and well performed systematic review.
P- Reviewers: Alves J, Beegun I S- Editor: Song XX L- Editor: Roemmele A E- Editor: Liu SQ
| 1. | Bader JD, Shugars DA. The evidence supporting alternative management strategies for early occlusal caries and suspected occlusal dentinal caries. J Evid Based Dent Pract. 2006;6:91-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Weerheijm KL, van Amerongen WE, Eggink CO. The clinical diagnosis of occlusal caries: a problem. ASDC J Dent Child. 1989;56:196-200. [PubMed] [Cited in This Article: ] |
| 3. | Borges BC, Campos GB, da Silveira AD, de Lima KC, Pinheiro IV. Efficacy of a pit and fissure sealant in arresting dentin non-cavitated caries: a 1-year follow-up, randomized, single-blind, controlled clinical trial. Am J Dent. 2010;23:311-316. [PubMed] [Cited in This Article: ] |
| 4. | Borges BC, de Souza Borges J, Braz R, Montes MA, de Assunção Pinheiro IV. Arrest of non-cavitated dentinal occlusal caries by sealing pits and fissures: a 36-month, randomised controlled clinical trial. Int Dent J. 2012;62:251-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 5. | Borges BC, De Souza Bezerra Araújo RF, Dantas RF, De Araújo Lucena A, De Assunção Pinheiro IV. Efficacy of a non-drilling approach to manage non-cavitated dentin occlusal caries in primary molars: a 12-month randomized controlled clinical trial. Int J Paediatr Dent. 2012;22:44-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | da Silveira AD, Borges BC, de Almeida Varela H, de Lima KC, Pinheiro IV. Progression of non-cavitated lesions in dentin through a nonsurgical approach: a preliminary 12-month clinical observation. Eur J Dent. 2012;6:34-42. [PubMed] [Cited in This Article: ] |
| 7. | Bakhshandeh A, Qvist V, Ekstrand KR. Sealing occlusal caries lesions in adults referred for restorative treatment: 2-3 years of follow-up. Clin Oral Investig. 2012;16:521-529. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Borges BC, de Souza Borges J, de Araujo LS, Machado CT, Dos Santos AJ, de Assunçao Pinheiro IV. Update on nonsurgical, ultraconservative approaches to treat effectively non-cavitated caries lesions in permanent teeth. Eur J Dent. 2011;5:229-236. [Cited in This Article: ] |
| 9. | Ahovuo-Saloranta A, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. 2008;CD001830. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Ahovuo-Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev. 2013;3:CD001830. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 11. | ten Cate JM. Remineralization of deep enamel dentine caries lesions. Aust Dent J. 2008;53:281-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Borges BC, Bezerra GV, Mesquita Jde A, Pereira MR, Aguiar FH, Santos AJ, Pinheiro IV. Effect of irradiation times on the polymerization depth of contemporary fissure sealants with different opacities. Braz Oral Res. 2011;25:135-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Borges BC, Catelan A, Sasaki RT, Ambrosano GM, Reis AF, Aguiar FH. Effect of the application of a casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) paste and adhesive systems on bond durability of a fissure sealant. Odontology. 2013;101:52-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Borges BC, Souza-Junior EJ, Catelan A, Lovadino JR, Santos PH, Paulillo LA, Aguiar FH. Influence of extended light exposure time on degree of conversion and plasticization of materials used as pit and fissure sealants. J Investig Clin Dent. 2010;1:151-155. [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Borges BC, Souza-Junior EJ, Catelan A, Ambrosano GM, Paulillo LA, Aguiar FH. Impact of extended radiant exposure time on polymerization depth of fluoride-containing fissure sealer materials. Acta Odontol Latinoam. 2011;24:47-51. [PubMed] [Cited in This Article: ] |
| 16. | Borges BC, Bezerra GV, Mesquita Jde A, Silva TR, Alves-Júnior C, Pinheiro IV, Braz R, Montes MA. Filler morphology of resin-based low-viscosity materials and surface properties after several photoactivation times. Acta Odontol Scand. 2013;71:215-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Borges BC, Barreto AS, Gomes CL, Silva TR, Alves-Jr C, Pinheiro IV, Braz R, Montes MA. Preheating of resin-based flowable materials in a microwave device: a promising approach to increasing hardness and softening resistance under cariogenic challenge. Eur J Esthet Dent. 2013;8:558-568. [PubMed] [Cited in This Article: ] |