Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8399
Peer-review started: September 13, 2023
First decision: November 22, 2023
Revised: November 27, 2023
Accepted: December 6, 2023
Article in press: December 6, 2023
Published online: December 16, 2023
In bow hunter’s syndrome (BHS), also known as rotational vertebral artery (VA) syndrome, there is dynamic/rotational compression of the VA producing verte
The patient, a 45-year-old man, presented to our hospital with occipital headache and vertigo. Computed tomography angiography showed anomalous C4 entry of right VA, with compression upon head rotation to that side. Thyroid cartilage and anterior tubercle of C5 transverse process were visibly at fault. We opted for sur
BHS is an important consideration where aberrant coursing of VA and neurologic symptoms coexist.
Core Tip: Herein, we report a rare case of bow hunter’s syndrome (BHS) induced by dynamic/rotational compression of the vertebral artery (VA) at the mid-cervical level associated with anomalous entry of the VA at C4. The VA was dynamically compressed between the thyroid cartilage and the anterior tubercle of the C5 transverse process upon right rotation. Complete symptom relief followed excision of the offending tubercle. BHS usually involves the atlantoaxial, rather than mid-cervical, VA. BHS linked to anomalous entry of the VA has rarely been reported. This case involves a rare etiology of BHS and a unique approach to its management.
- Citation: Ahn JH, Jun HS, Kim IK, Kim CH, Lee SJ. Atypical case of bow hunter’s syndrome linked to aberrantly coursing vertebral artery: A case report. World J Clin Cases 2023; 11(35): 8399-8403
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8399.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8399
In bow hunter’s syndrome (BHS), also known as rotational vertebral artery (VA) syndrome, there is dynamic com
A 45-year-old man presented to the hospital with a 3-mo history of occipital headache, which began after a marathon race.
During the prior month, he had also complained of a spinning sensation within moments of turning his head to the right.
Other than admitted hypertension, his general health was good.
The patient denied any family medical history.
During the neurologic examination, head-turning to the right induced nystagmus of left-sided gaze.
The patient had no abnormalities in blood and urine tests.
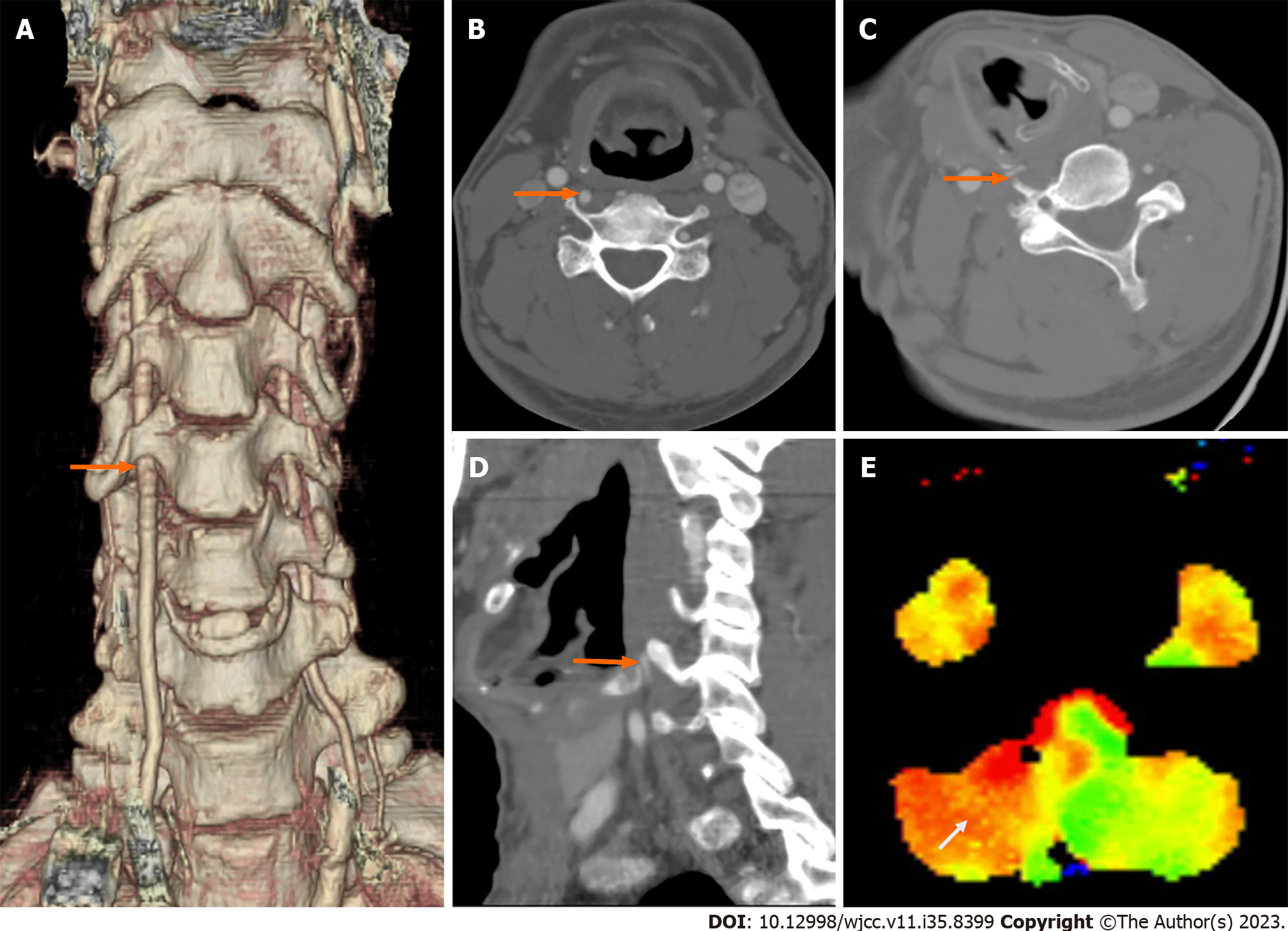
Computed tomography angiography (CTA) and perfusion magnetic resonance imaging (MRI) were performed to assess for VBI. The CTA showed normal left VA entry at C6 vertebra, with right VA entering the C4 transverse foramen (Figure 1A and B). Both thyroid cartilage and anterior tubercle of C5 transverse process brought compression of right VA upon head-turning to the right (Figure 1C and D). Perfusion MRI acquired with right head rotation also indicated a time-to-peak delay in right cerebellar territory (Figure 1E).
Base on the results of the imaging examinations, the final diagnosis was BHS linked to aberrantly coursing VA.
This extrinsic obstruction of VA called for surgical intervention through anterior cervical approach. A skin incision was made above medial sternocleidomastoid muscle to remove the offending C5 tubercle and achieve wide VA decom
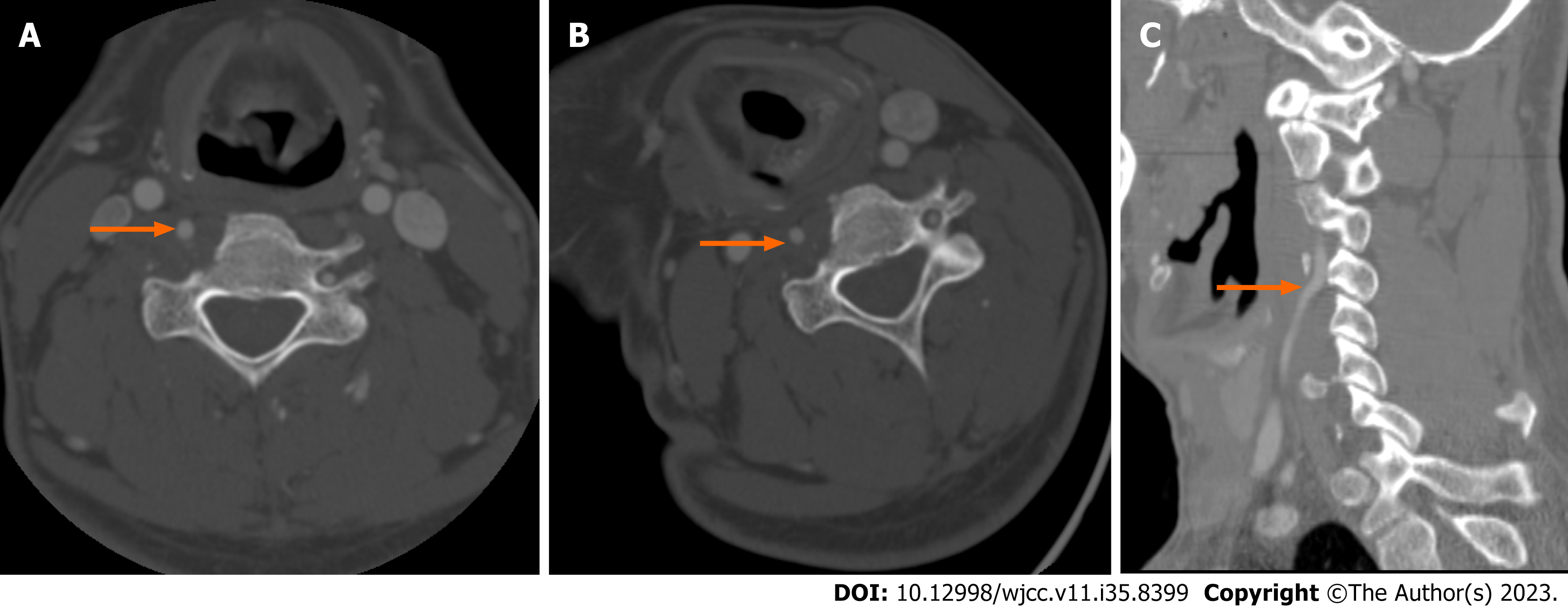
Following surgery, complete elimination of culprit bone (Figure 2A) and absence of right rotational compression were documented by CTA (Figure 2B and C). Patient recovery was uneventful, with full and lasting resolution of preoperative symptoms.
The VA ordinarily runs cephalad within transverse foramina of the cervical spine, entering at C6 level and exiting at C1. Aberrancies in course are rare and are byproducts of anomalous embryologic development[6]. According to the literature, the compressive impact of BHS is usually borne at C2 level or above, with a left-dominant VA more likely involved[7]. Although bony malformations or regional instability are both implicated in BHS, the present case indicates that VA aberrancy may contribute as well, predisposing to dynamic mid-cervical compression. Karle et al[4] and Jongbloed et al[5] have chronicled similar VA entries at C4 and C5, respectively[4,5]. The relatively narrow space afforded and encroaching structures (i.e, thyroid cartilage, anterior tubercle of cervical spine) are apt to intensify compressive insults.
Dynamic VA occlusion is expectedly signaled by VBI symptoms, namely vertigo, dizziness, syncope, paresthesia, ataxia, or headache[8]. Review of the limited available literature suggests there is also increased risk of recurrent embolic stroke[9,10]. Although the precise mechanism of our patient’s occipital headache is not fully understood, it is feasible that pro-inflammatory neurotransmitter release triggered by localized irritation may have elicited pain remote from points of actual injury[11]. In a patient presenting with headache and positional VBI symptoms, such as nystagmus or transient vertigo, BHS is then a valid consideration; and provocative CTA (with head rotation) is the principal means of confirming any clinical suspicions.
Once a diagnosis of BHS is established, the condition may be managed conservatively or surgically treated. Conservative measures include avoidance of head rotation and anticoagulant or antiplatelet therapy. However, these actions fail to address underlying pathologies, proving ineffective for some. Surgical treatments range from direct VA decompression to cervical spine fusion, depending on circumstances and level of VA compromise. There have been two published cases of BHS and aberrant VAs where laryngoplasties served to eliminate problematic superior cornual ossifications of thyroid cartilage[4,5]. Ultimately, direct VA decompression achieved by resecting a prominent tubercle readily sufficed for our patient.
The middle-aged man we describe presented with BHS of unusual nature, marked by aberrant coursing of right VA and mid-cervical compressive symptoms. This predicament was successfully remedied through careful diagnostic workup and surgical decompression. BHS must always be considered in analogous situations where comparable anomalies and neurologic manifestations coexist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koumantakis GA, Greece S-Editor: Qu XL L-Editor: A P-Editor: Qu XL
| 1. | Rastogi V, Rawls A, Moore O, Victorica B, Khan S, Saravanapavan P, Midivelli S, Raviraj P, Khanna A, Bidari S, Hedna VS. Rare Etiology of Bow Hunter's Syndrome and Systematic Review of Literature. J Vasc Interv Neurol. 2015;8:7-16. [PubMed] [Cited in This Article: ] |
| 2. | Duan G, Xu J, Shi J, Cao Y. Advances in the Pathogenesis, Diagnosis and Treatment of Bow Hunter's Syndrome: A Comprehensive Review of the Literature. Interv Neurol. 2016;5:29-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Sorensen BF. Bow hunter's stroke. Neurosurgery. 1978;2:259-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 151] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Karle WE, Buniel MC, Lutsep HL, Hamilton BE, Nesbit GM, Schindler JS. Thyroid cartilage compression causing stroke. Laryngoscope. 2019;129:E445-E448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Jongbloed W, Gertel A, Kashat L, Singh R, Parham K. Vertebral Artery Compression by the Greater Cornu of the Thyroid Cartilage. Ear Nose Throat J. 2023;102:301-303. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 6. | Uchino A, Saito N, Takahashi M, Okada Y, Kozawa E, Nishi N, Mizukoshi W, Nakajima R, Watanabe Y. Variations in the origin of the vertebral artery and its level of entry into the transverse foramen diagnosed by CT angiography. Neuroradiology. 2013;55:585-594. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Zaidi HA, Albuquerque FC, Chowdhry SA, Zabramski JM, Ducruet AF, Spetzler RF. Diagnosis and management of bow hunter's syndrome: 15-year experience at barrow neurological institute. World Neurosurg. 2014;82:733-738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Lima Neto AC, Bittar R, Gattas GS, Bor-Seng-Shu E, Oliveira ML, Monsanto RDC, Bittar LF. Pathophysiology and Diagnosis of Vertebrobasilar Insufficiency: A Review of the Literature. Int Arch Otorhinolaryngol. 2017;21:302-307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Grossmann RI, Davis KR. Positional occlusion of the vertebral artery: a rare cause of embolic stroke. Neuroradiology. 1982;23:227-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Tominaga T, Takahashi T, Shimizu H, Yoshimoto T. Rotational vertebral artery occlusion from occipital bone anomaly: a rare cause of embolic stroke. Case report. J Neurosurg. 2002;97:1456-1459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Sheikh HU. Headache in Intracranial and Cervical Artery Dissections. Curr Pain Headache Rep. 2016;20:8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |