Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1086
Peer-review started: June 30, 2021
First decision: October 18, 2021
Revised: October 27, 2021
Accepted: December 22, 2021
Article in press: December 22, 2021
Published online: January 21, 2022
The corona virus disease 2019 (COVID-19) has been a pandemic for more than one year and estimated to affect the whole world in the near future.
Here we reported that one COVID-19 patient with vesicles was treated by bullectomy. The patient’s perioperative laboratory tests were analyzed. The pathological findings of bullectomy were described and compared with those of common bulla cases.
This patient with vesicles underwent bullectomy and had a poor prognosis. He showed diffuse alveolar damage and extensive necrosis in bullectomy specimen. We hope our report will be of interest for clinicians who will treat COVID-19 patients in the future.
Core Tip: We reported that one corona virus disease 2019 (COVID-19) patient with vesicles was treated by bullectomy. The patient’s perioperative laboratory tests were analyzed. The pathological findings of bullectomy were described and compared with those of common bulla cases. This patient with vesicles underwent bullectomy and had a poor prognosis. He showed diffuse alveolar damage and extensive necrosis in bullectomy specimen. We hope our report will be of interest for clinicians who will treat COVID-19 patients in the future.
- Citation: Tang HX, Zhang L, Wei YH, Li CS, Hu B, Zhao JP, Mokadam NA, Zhu H, Lin J, Tian SF, Zhou XF. Bullectomy used to treat a patient with pulmonary vesicles related to COVID-19: A case report. World J Clin Cases 2022; 10(3): 1086-1092
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1086.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1086
Pulmonary bullae are cavities more than one centimeter in diameter in the lung that form from structurally damaged lung tissue due to a variety of etiologies[1]. When nonoperative approaches for pulmonary bullae are ineffective, in some cases, surgical resection can be considered[2,3].
Corona virus disease 2019 (COVID-19) presents with a severe phenotype in as many as 26% of patients. Medical therapy is lacking, and many of these patients require intubation and even extracorporeal life support[4]. COVID-19 mainly attacks the lungs and other organs that express angiotensin-converting enzyme 2 receptors[5]. Patients with pneumonia who are infected with COVID-19 have been reported to develop pulmonary vesicles and tension pneumothorax with the use of ventilators. Pulmonary vesicles are defined as peripheral predominant consolidation patterns with internal round cystic changes[6]. Because of the high risk of health care worker transmission and the difficulty in performing an operation with full personal protective equipment, operations for patients infected with COVID-19 are quite difficult; thus, these operations are extremely rare. Recently, we performed a bullectomy under special circumstances as the last option to treat a patient.
Intermittent fever for 1 wk.
The patient suffered from chest tightness and chest pain due to infection with COVID-19 5 d ago. He urgently went to the local hospital to see a doctor. The perfect chest X-ray showed a right pneumothorax, and the patient’s dyspnea was progressively worsening. The local hospital gave an emergency tracheal intubation, connected to a ventilator to assist breathing, and transferred him to our intensive care unit for treatment.
Denies the history of diabetes, heart disease, etc. Denies the history of infectious diseases such as tuberculosis and hepatitis. Denies the history of food and drug allergy. Denies the history of trauma surgery.
Denies the family history of genetic disease.
T 38.3 ℃, P 85 bmp, HR 20 bmp, diastolic blood pressure: 69 mmHg, systolic blood pressure: 116 mmHg, mentally clear, good spirits, no yellowing of skin and mucous membranes throughout the body, and superficial lymph nodes less than swollen. Pharyngeal is not congested, breath sounds in both lungs are clear, heart rhythm is uniform, no pathological murmurs are heard in each valve area. HR 85 bpm, the heart rhythm is uniform, no pathological murmur is heard in each valve area. Abdomen is soft, no tenderness and rebound pain, liver, spleen and ribs are not in reach, Murphy sign is negative, there is no percussion pain in the kidneys, no redness and swelling of the limbs and joints, and no edema of the lower limbs.
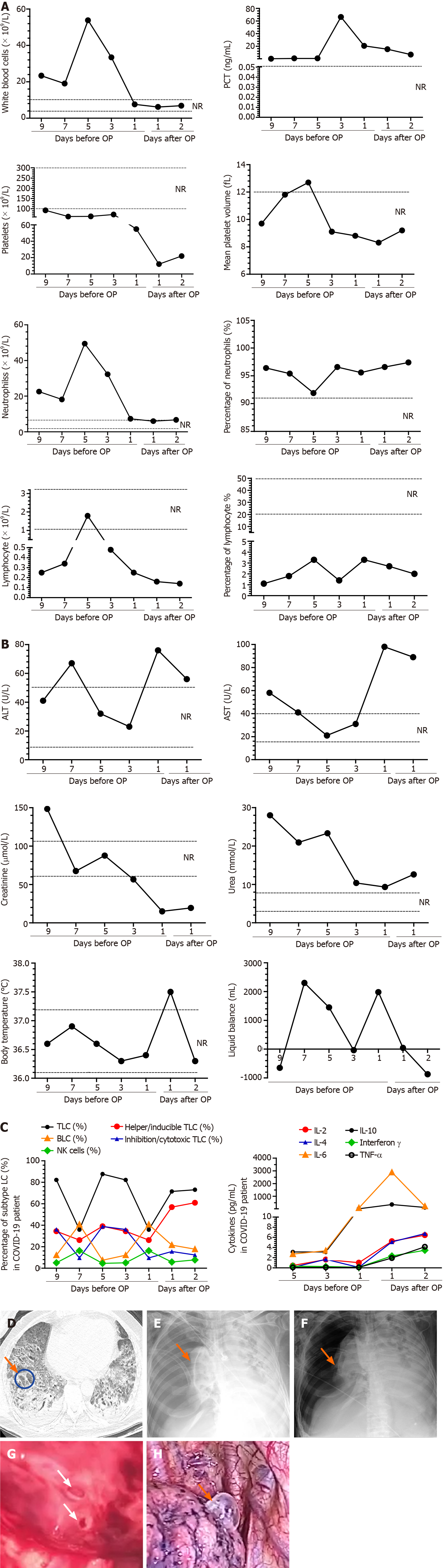
T lymphocyte (%) [February 24, 2020] 87.67, [March 12, 2020] 73.15; Helper/inducible T lymphocytes (%) [February 24, 2020] 39.09, [March 12, 2020] 60.97; NK cells (%) [February 24, 2020] 4.55, [March 12, 2020] 7.73; Interleukin-6 (pg/mL) [February 24, 2020] 2.46, [March 12, 2020] 211.33; Interleukin-10 (pg/mL) [February 24, 2020] 29.22, [March 12, 2020] 122.35; White blood cells (×109/L) [February 22, 2020] 21.99, [March 11, 2020] 6.88; Red blood cells (×1012/L) [February 22, 2020] 3, [March 11, 2020] 3.61; hemoglobin (g/L) [February 22, 2020] 92.0, [March 11, 2020] 116.0; platelet (×109/L) [February 21, 2020] 154, [March 11, 2020] 22; Alanine aminotransferase (U/L) [February 21, 2020] 41, [March 10, 2020] 56; Aspartate aminotransferase (U/L) [February 21, 2020] 58, [March 10, 2020] 89.
The X-ray before bullectomy: Infection of both lungs, massive pneumothorax on the right side; The chest CT scan before bullectomy; Severe infection of both lungs, extensive bullae; The X-ray after bullectomy; The X-ray before bullectomy: Both lung infections, the right pneumothorax improved significantly.
Spontaneous pneumothorax, Respiratory failure, lung infection with COVID-19, Septic shock, ARDS.
Received ECMO support, underwent a bullectomy.
This patient with vesicles underwent bullectomy and had a poor prognosis. He showed diffuse alveolar damage and extensive necrosis in bullectomy specimen.
The etiology of pulmonary bulla is complex and includes chronic obstructive pulmonary disease, emphysema, ventilator-related lung injury, and COVID-19[1]. Patients who have pulmonary vesicles shown on chest CT scans, and peripheral predominant consolidation patterns with internal round cystic changes[6], are more prone to pulmonary bullous formation. However, the influence of COVID-19 on pulmonary vesicles has not yet been reported.
Our study found that as alveolar structure destruction occurred quickly, the wall of the air cavity was significantly thicker than that of common pulmonary bulla (Figure 1G and H). In this process, the inflammatory storm is also an important factor[4]. Thus, we believe that the destruction of alveolar structure due to COVID-19 easily induces emphysema and then causes the formation of pulmonary vesicles.
Although pulmonary vesicles are not exactly bulla, they can easily develop into them. The most effective approach to treat symptomatic pulmonary bulla is surgical resection[7], which is widely accepted by thoracic surgeons worldwide. Nevertheless, it was a difficult choice for treating COVID-19 patients with pulmonary vesicles. It is clear that when patients have tension pneumothorax, chest drainage tubes must be placed as soon as possible. In this study, one patient underwent bullectomy, with pulmonary vesicles induced by COVID-19 and tension pneumothorax. To our knowledge, this operation was the first bullectomy performed on a COVID-19 patient with both gross and histologic findings. Regrettably, the outcome of this patient was poor after undergoing bullectomy (Figure 1F).
This is also the first report on pathological findings of COVID-19 complicated by emphysematous bulla formation in the lung. Interactions of multiple factors, including diffuse alveolar damage overlapping with extensive necrosis, abundant neutrophils in lung tissue that can produce matrix metalloproteinase, and elevated levels of cytokines such as interleukins in the peripheral blood, may have led to bulla formation in this case.
In conclusion, COVID-19 may induce the formation of pulmonary vesicles, which have a thicker air cavity wall than common bulla. Considering ventilator-related lung injury, it is recommended to choose the ventilator mode and PEEP carefully. Based on the extensive destruction of lung tissue by COVID-19, the use of bullectomy is limited, only as a last resort and trial treatment if the patient accepts. More research is needed to explore the specific mechanisms of pulmonary vesicle formation to improve the efficacy of COVID-19 pneumonia treatment, especially in patients with severe COVID-19 with vesicles.
We thank all our colleagues who helped us during the current study. We greatly appreciate the kind assistance of Professor Bicheng Wang and Doctor Lijun Cai (Both are in the Department of Pathology, Zhongnan Hospital of Wuhan University, Wuhan, China) in staining the sections, as well as Doctor Xianguo Wang and Doctor Zetian Yang (Both are in the Department of Thoracic Surgery, Zhongnan Hospital of Wuhan University, Wuhan, China) for his assistance in discussing the key issues of this study. We are also grateful to the many front line medical staff for their dedication in the face of the COVID-19 outbreak, despite the potential threat to their own lives and the lives of their families.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yalçinkaya İ S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Erne BV, Graff M, Klemm W, Danzl JG, Leschber G. Bulla in the lung. Lancet. 2012;380:1280. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Ozawa Y, Sakai M, Ichimura H. Covering the staple line with polyglycolic acid sheet vs oxidized regenerated cellulose mesh after thoracoscopic bullectomy for primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg. 2018;66:419-424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Sim SKR, Nah SA, Loh AHP, Ong LY, Chen Y. Mechanical vs Chemical Pleurodesis after Bullectomy for Primary Spontaneous Pneumothorax: A Systemic Review and Meta-Analysis. Eur J Pediatr Surg. 2020;30:490-496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14113] [Cited by in F6Publishing: 14170] [Article Influence: 3542.5] [Reference Citation Analysis (0)] |
| 5. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17476] [Cited by in F6Publishing: 17282] [Article Influence: 4320.5] [Reference Citation Analysis (0)] |
| 6. | Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425-434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2493] [Cited by in F6Publishing: 2226] [Article Influence: 556.5] [Reference Citation Analysis (0)] |
| 7. | Neidhart P, Suter PM. Pulmonary bulla and sudden death in a young aeroplane passenger. Intensive Care Med. 1985;11:45-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |