Copyright
©The Author(s) 2022.
World J Clin Cases. Jul 6, 2022; 10(19): 6406-6416
Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6406
Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6406
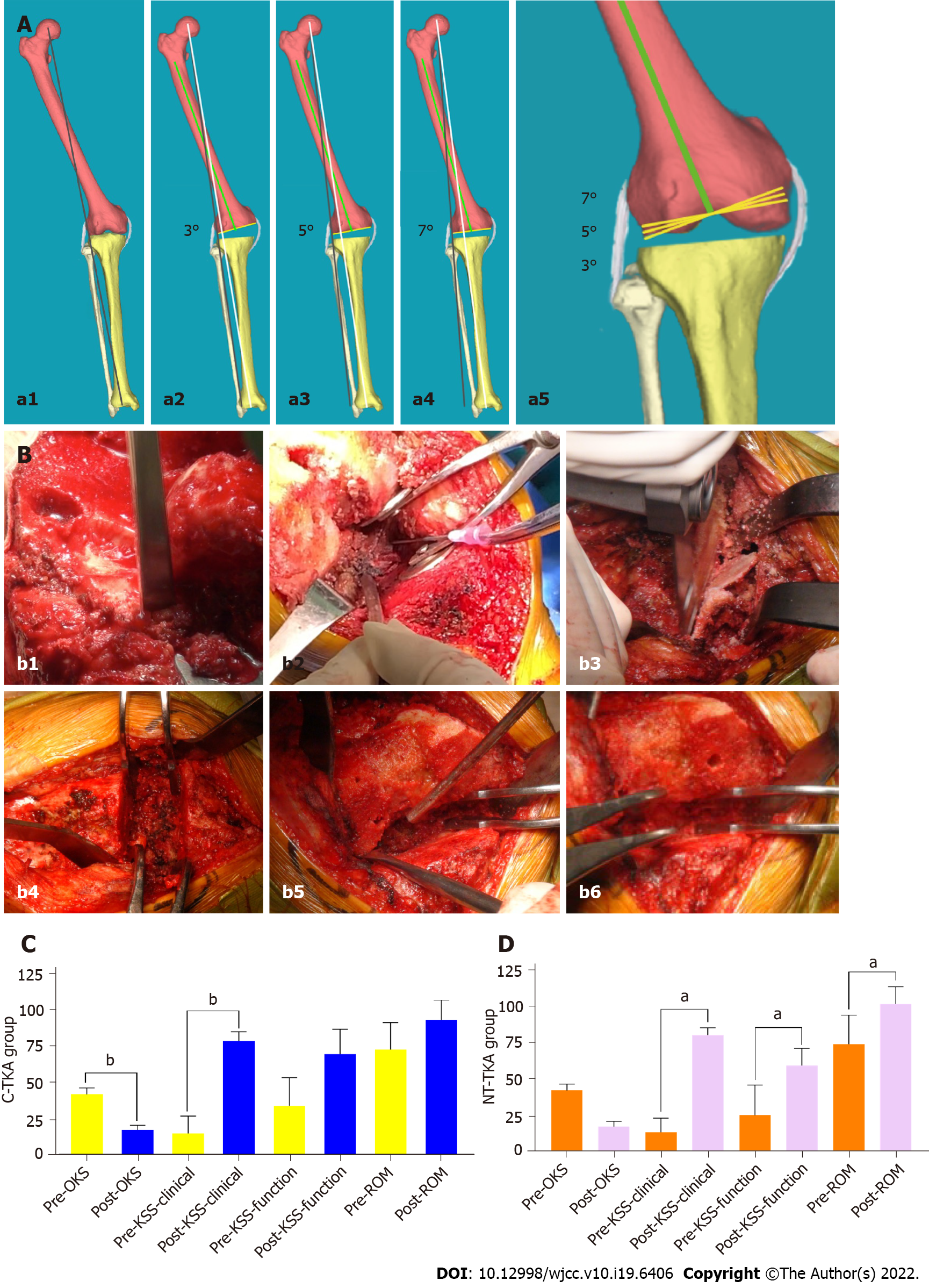
Figure 2 The new osteotomy technique, soft tissue balancing technique, and follow-up results of joint function.
A: Schematic diagram of the distal femoral valgus osteotomy. Preoperative lower limb mechanical axis (MA) (a1, blackline), 3° (a2), 5° (a3), and 7° (a4) valgus osteotomy in distal femur osteotomy (white line: new MA; green line: anatomical axis of femur; yellow line: bone cutting plane) are shown, and 5° and 7° valgus cut angle can correct more osseous MA and increase the relative length of the lateral collateral ligament compared with 3° (a5); B: A 65-year-old man with 18° of valgus knee deformity in the new theory total knee arthroplasty (NT-TKA) group. The surgical procedure included osteophytes removal (b1), soft tissue release with a 20 mL syringe needle (b2), osteotomy (b3), straightening gap balance (b4), soft tissue cuff-like release (b5), and buckling gap balance (b6); C and D: Comparison of Oxford knee score (OKS), knee society score (KSS), and range of motion (ROM) between pre- and post-operation in conventional total knee arthroplasty (C-TKA) group (C) and NT-TKA group (D), respectively. bP < 0.01, compared with pre-OKS, KSS, and ROM in NT-TKA and pre-KSS clinical stability in C-TKA. aP < 0.05, compared with pre-OKS in C-TKA. C-TKA: Conventional total knee arthroplasty; NT-TKA: New theory total knee arthroplasty; OKS: Oxford knee score; KSS: Knee society score; ROM: Range of motion.
- Citation: Lv SJ, Wang XJ, Huang JF, Mao Q, He BJ, Tong PJ. Total knee arthroplasty in Ranawat II valgus deformity with enlarged femoral valgus cut angle: A new technique to achieve balanced gap. World J Clin Cases 2022; 10(19): 6406-6416
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6406.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6406