Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6032
Peer-review started: January 10, 2022
First decision: February 14, 2022
Revised: February 21, 2022
Accepted: April 20, 2022
Article in press: April 20, 2022
Published online: June 26, 2022
Hypertrophic scars and keloid treatment is a major problem in plastic surgery. While small keloids can be treated with resection followed by radiotherapy, large keloids require treatment with a tissue expander. Conventional methods increase the need for auxiliary incisions, causing new scar hyperplasia.
To introduce a new method for the treatment of keloids with an expander.
Between 2018 and 2021, we performed surgeries to treat large keloids in nine patients with a two-stage approach. In the first stage, an intrascar incision was made in the keloid, and a customized expander was implanted under the keloid and the surrounding normal skin. A period of 3-6 mo was allowed for skin expansion. In the second stage, after the initial incision healed, a follow-up surgery was performed to remove the expander, resect the keloid, and repair the expanded skin flap. To accomplish this, an incision was made along the scar boundary to avoid making a new surgical incision and creating new scars. Superficial radiotherapy was then performed postoperatively.
Two patients had anterior chest keloids. After treatment, the anterior chest incision was broken repeatedly and then sutured again after debridement. It healed smoothly without scar hyperplasia. Keloids were successfully removed in 7 patients without recurrence.
This method was performed through a keloid incision and with a custom expander embedded. After full expansion, the keloid was directly resected using a linear suture, which avoids new surgical incisions and scars and can successfully remove large-area keloids. The treatment is effective, providing new insights and strategies for the treatment of similar large-area keloid and hypertrophic scar cases in the future.
Core Tip: This paper introduces a new method for the treatment of keloids with an expander. After treatment with a single linear incision, the surgical incision was located on the keloids. Thus, because there was no additional auxiliary incision, the possibility of a new keloid was reduced.
- Citation: Wu M, Gu JY, Duan R, Wei BX, Xie F. Scar-centered dilation in the treatment of large keloids. World J Clin Cases 2022; 10(18): 6032-6038
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6032.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6032
Keloid treatment has always been a major problem for surgeons[1,2]. Keloids are caused by fibroblast proliferation disorders during wound healing[1,3]. Current treatments mainly include topical or oral drugs, surgical treatment, radiotherapy, and laser therapy. Specifically, these include topical (tape/ointment) and injectable adrenocorticotropic hormones, compression therapy and silica gel (application of bandages, stents, plastic clothes, among others), surgical resection, sutures, surgical resection after skin graft or flap reconstruction, and postoperative radiotherapy, among other treatments[5]. Drug injections can be used to treat small keloids, while surgical resection and superficial radiotherapy are often used to treat large keloids[5-7]. However, it is often difficult to resect keloids with large areas directly by surgery[8,9].
In 1979, the American Society of Plastic Surgeons officially recognized expander therapy was initiated in 1976, and officially recognized skin dilation as a form of expander therapy, and it has since been widely used[10,11]. Skin dilation, which entails embedding an expander and continuously pumping water to expand the normal skin and increase the area, can be used to repair skin lesions. The method is advantageous as it avoids donor site injury, has a good repair effect, and ensures the color and texture of the flap match the recipient area. Therefore, expanders have been widely used to treat hypertrophic scars and keloids in recent decades[12,13]. However, previously reported methods involved burying the expander near the scar. During skin dilation, the expanded skin flap must be rotated or pushed to repair skin lesions; thus, an auxiliary incision is needed. For patients with scar constitution, a new incision means there is a possibility for new keloid formation.
In this study, we describe a new method for treating large keloids that minimizes the need for a new surgical incision, thereby reducing the chances of new keloid formation. In this method, a direct incision was made on the keloid to form an expander bag with a capsule cavity that includes the keloid and the surrounding normal skin. After full expansion, the keloid was directly excised and the expanded flaps were pulled together and sutured linearly, minimizing the need for a new surgical incision.
Before surgical treatment, a detailed medical history was obtained, and a physical examination was performed for each patient. The size and shape of the custom expanders were designed based on the lesion site and the shape of the surrounding normal skin. Each custom expander was 2.5 times the diameter of the lesion.
The skin expander was implanted during the first surgery stage. The patient was placed under general anesthesia, and the surgical sites were routinely disinfected. An incision, the length of the long axis of the scar, was made along the midline of the scar. The incision was not extended beyond the boundary of the scar. Based on the customized expander, the boundary of the separated expansion cavity was marked with Meilan. The boundary usually exceeded the shape of the expander by 1 cm. The full-thickness of scar tissue was cut with a blade, and taking care to maintain a uniform vertical section, the subcutaneous fat was cut down to the surface of the myometrium, and the cavity separated from the surface of the muscular membrane. During separation, the perforating vessels were electro-coagulated or ligated. The separated cavity was 1 cm wider than the boundary of the customized expander to ensure that the expander could be fully expanded without folding after implantation. Separation of the injection pot cavity and pot mouth position and the injection pot from the expansion of the capsule cavity 10 cm was done. To achieve hard support, we ensured that the bottom of the pot was at the appropriate depth, it was easy to touch on the body surface, and the expansion was optimal. Prior to placing the expander in the separated cavity, we ensured that it had no leaks. We also checked the chassis position, flattened the expander, and placed the injection bottle that was inserted in the drainage tube in the separated cavity. We were careful not to puncture the expander during suturing.
The wound dressing was changed routinely on the second day after surgery, and the drainage tube was removed when the drainage volume was less than 20 mL (this volume was based on the size of the embedded expander and was estimated based on clinical experience). The suture was removed on the 14th day after the first surgery, and a small amount of water was injected into the cavity twice per week. The volume injected was 10% of the designed capacity of the expander; however, this was not always the case. We paid special attention to the color and tension of the expanded flap and the sensation of pain around the flap area. Therefore, if the patient was obviously uncomfortable, the tension of the flap was too high, or the color of the flap was white, the water infusion was stopped, and the site of injection was monitored over time. When the expander was filled with water to 3-4 times its designed volume, the second stage surgery to remove the keloid was commenced. Prior to initiating the second surgery, the size of the expanded flap was measured to determine whether the normal skin on both sides of the scar was sufficient to cover the chassis.
During the second-stage surgery, the expander was removed, the scar excised, and the expanded flap repaired. To achieve this, an incision was made along the scar boundary to remove the lesion from the normal tissue completely and remove the expander and injection pot. While paying attention to the treatment of both sides of the flap, the flaps were pulled towards the midline of the incision and sutured, and an appropriate drainage tube was inserted. A multi-layer tension-reduction cosmetic suture using one silk suture was required. The bottom of the flap was tethered to the rib periosteum while ensuring that there was no tension in the suture. A full subcutaneous reduction was required in patients with scar constitution.
The wound was dressed, and the drainage tube was removed as described earlier. The suture was removed between days 10 and 14 after surgery and prior to radiotherapy[14]. Radiotherapy, totaling 20 Gy, was administered in four sessions at a dose of 5 Gy per session. Radiotherapy was started on the first day post-surgery (if the first day after surgery was on the weekend, radiotherapy was suspended for two days and continued the following Monday)[15,16]. To prevent recurrence of keloids and hypertrophic scars, adequate anti-scar treatment was provided postoperatively, which included the early and effective application of reducing devices, external use of silicone gel for three months, and avoidance of foods including spicy foods, seafood, and alcohol. In addition, we ensured regular review and close postoperative follow-up of the patients.
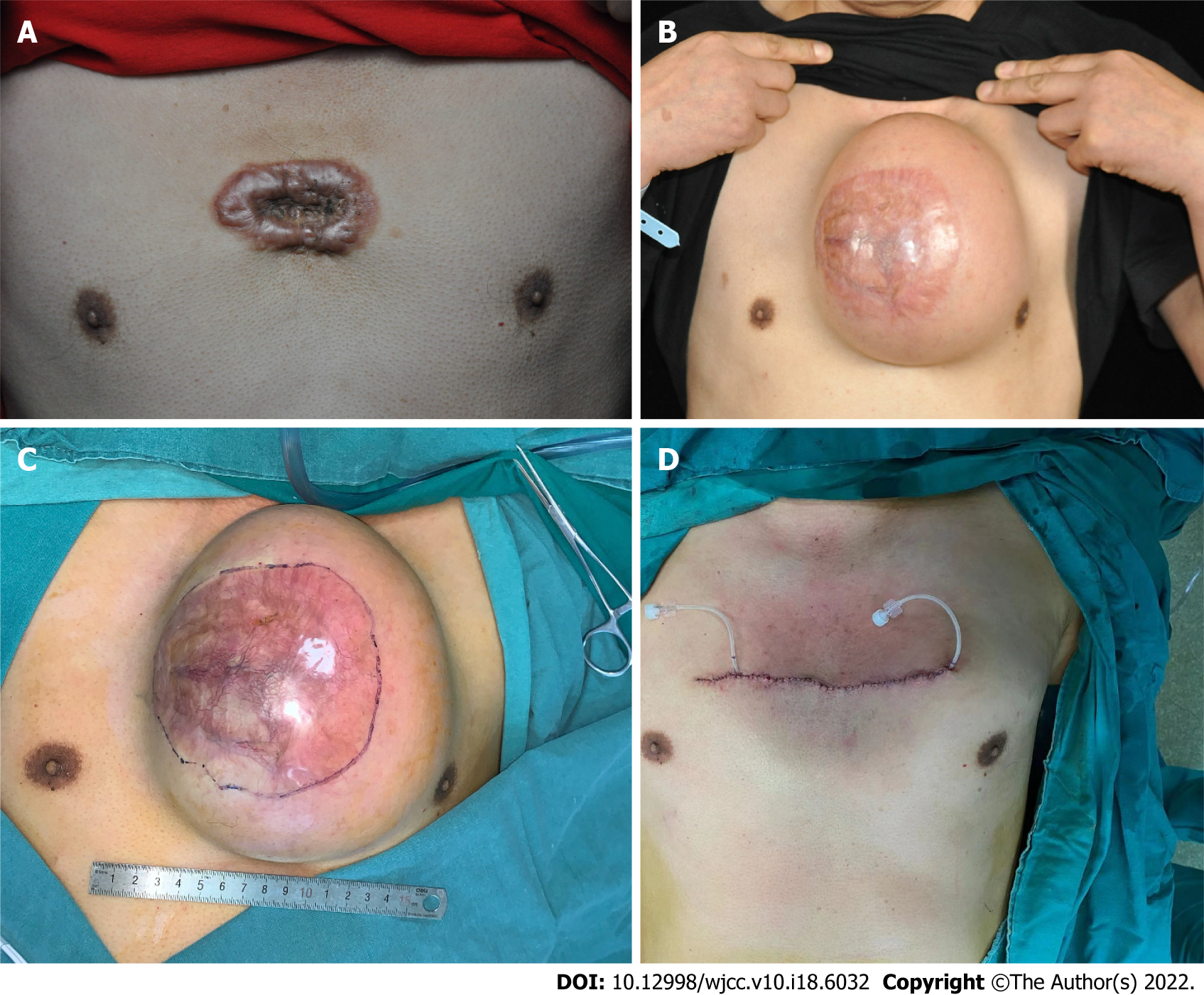
The size of the keloids ranged from 2 cm × 5 cm to 15 cm × 13 cm in surgical patients (Table 1). The expansion time and designated volume of the customized expander were 3–5 mo (mean, 4 mo), and 100–800 mL (mean, 500 mL), respectively. The total volume of water injected ranged from 320–2400 mL (average, 1452 mL). Keloids were completely removed, and the surgery resulted in a linear scar. One patient had a long-term unhealed wound in the anterior chest for half a year after scar resection and radiotherapy. In this patient, the wound was directly reopened and re-sutured without further radiotherapy. This treatment resulted in smooth healing of the wound without keloid recurrence.
| Patients | Age (yr) | Scar area (cm) | Dilator size (mL) | Total water injection (mL) | Location |
| 1 | 23 | 6.5 × 4.5 | 200 | 600 | Chest |
| 2 | 69 | 15 × 10 | 800 | 2400 | Back |
| 5 × 3 | 200 | 600 | Back | ||
| 3 | 28 | 15 × 13 | 700 | 2161 | Chest |
| 4 | 13 | 2 × 5 | 100 | 350 | Upper limb |
| 5 | 35 | 6 × 4 | 400 | 1200 | Chest |
| 6 | 32 | 13 × 4 | 100 | 320 | Neck |
| 7 | 24 | 10 × 6 | 600 | 1300 | Chest |
| 8 | 30 | 15 × 5 | 800 | 2400 | Abdomen |
| 9 | 24 | 11 × 6 | 500 | 1500 | Chest |
Total nine patients underwent keloid repair surgery, which was conducted in two stages between 2018 and 2021. In the first stage, customized expanders were implanted under the scars, and in the second stage, scar resection and expanded skin flap repair were performed. Due to the different shapes of the keloids, the customized expanders used were also different (Table 1).
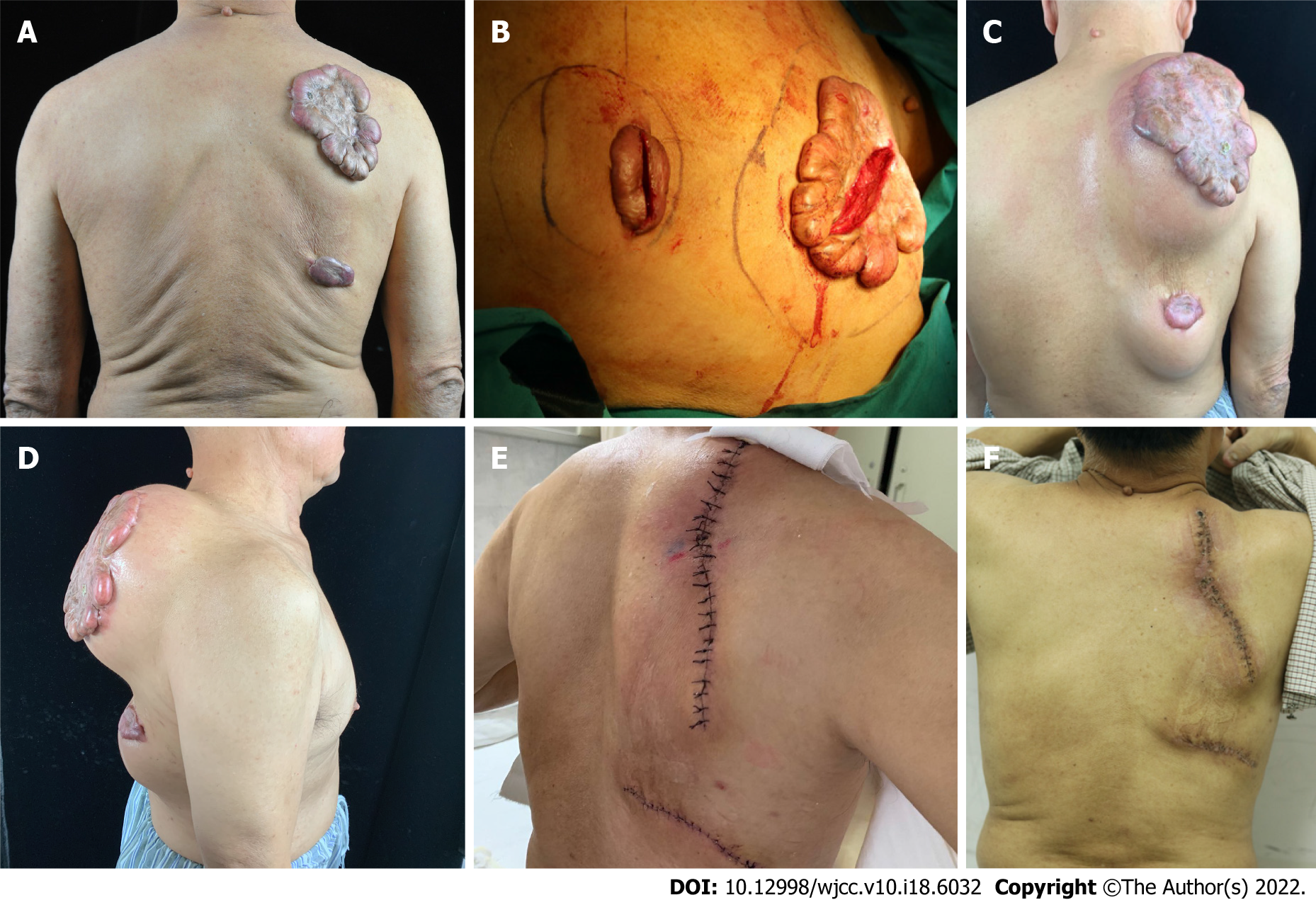
The expander size ranged from 100-800 mL. The final expansion size was between 320 and 2400 mL. The water injection interval was 2 d, and each injection volume was 10% of the design capacity. When the tension of the flap was too high, a smaller volume could be injected. Expansion time in March-May, and an average of April. Representative patient cases are presented in Figure 1 and Figure 2.
Keloid-centered expansion has replaced traditional para-scar expansion. The main advantages are as follows: (1) Incisions are made in hypertrophic scars or keloids, and the wound has a strong tensile strength. This is because the healing surface includes thick scar tissue and the underlying adipose tissue. Therefore, in the process of expansion, incision dehiscence does not occur; (2) Unlike the traditional method in which the expander is embedded via an incision in the normal skin, this method of incision in the scar area will not add any new surgical scars, which is particularly important for people with a scar physique and does not require a new drainage tube incision. Furthermore, a previous report has confirmed that a scar within the vicinity of the incision will not cause keloid hyperplasia[17]; and (3) During the expansion process, keloids stop developing and even partially subside due to pressure compression. This phenomenon has not been previously reported.
In this study, one patient presented with two keloids, and satisfactory results were achieved for both keloids with the keloid-centered expansion approach. In another patient, the case was complicated by poor wound healing for half a year, which manifested as epidermal erosion, exudation, and crusting. After extensive subcutaneous separation and re-suturing, the wound healed successfully. The wound healed poorly in this patient because the surgical tension was concentrated at the incision, which caused the scar at the incision to widen continuously under tension traction, and this wound was associated with the radiotherapy area. To avoid such complications, attention should be paid to the selection of an appropriate multi-gradient tension suture (specifically a flap deep and periosteum tension suture), in addition to the need for subcutaneous tension suture. This prevents the concentration of the flap tension on the wound.
The method of implanting the expander via a scar incision, as described in this report, effectively reduces the risk of additional scarring, which is a significant advantage. In addition, during the expansion process, the pressure achieved with water injection plays a role in compressing the keloids. According to clinical observations, skin expansion under keloids can prevent and reverse the pathological progress of keloids. This is another significant advantage of the keloid-centered expansion approach. After the second-stage operation to remove the lesion, the flaps were directly sutured. The resulting linear incision prevents the need for an auxiliary incision. Compared with the pedicle flap and free flap, the technical requirements and accuracy of the keloid-centered expansion approach are superior.
To repair a particular area of a keloid, custom-designed expanders are required. The diameter of a normal skin expander should be 2–3 times the keloid diameter. After expansion, the scar can be successfully removed, and the wound successfully closed. If the normal skin area to be expanded is too small, even after expansion, there will not be sufficient normal skin, and the tension will be too high to remove the scar completely when closing.
In this study, postoperative radiotherapy consisted of 20 Gy, continuous irradiation for 4-5 d, starting from the first day after surgery. A 4–5 Gy linear accelerator electron beam radiotherapy can penetrate 2-3 mm below the skin[18,19].
In the method described in this report, the surgical incision was simple, and no auxiliary incisions were required. Previous expander transfer methods included propulsion and rotation methods. An auxiliary incision is required to fully expand a hemispherical expanded flap using those methods. In this study, the expander was in the central part of the scar; thus, no auxiliary incision was needed.
The expansion process to achieve keloid compression effectively prevents the progression of keloids. However, there is also a risk of complications. After the expansion, the tension at the incision is large, and since the scar is around the incision, there is a high risk of skin damage. Therefore, after the second-stage surgery, the probability of healing is low. To mitigate this risk, a deep tension-reduction suture should be considered.
From this study of surgical patients, we present a new method, keloid-centered expansion, that we believe can successfully remove large keloids and have good prospects for healing since this method prevents the need for auxiliary incisions and reduces the risk for the formation of new keloids. The sequence of events associated with this method includes scar incision, customized expander implantation, skin expansion to remove the keloid, formation of a single linear suture incision, followed by postoperative radiotherapy.
Current treatment modalities are classified as either conservative or surgical. Conservative treatments include intra-scar injection of anti-scar drugs, laser, external force compression, and radiotherapy, although complete curation is often not achieved. While small keloids can be directly resected followed by radiotherapy, large keloids cannot be directly resected; they require treatment with a tissue expander.
We present a new method, keloid-centered expansion keloid-centered expansion.
After treatment with a single linear incision, the surgical incision was located on the keloids. Thus, because there was no additional auxiliary incision, the possibility of a new keloid was reduced.
In the first stage, an intrascar incision was made in the keloid, and a customized expander was implanted under the keloid and the surrounding normal skin. A period of 3-6 mo was allowed for skin expansion. In the second stage, after the initial incision healed, a follow-up surgery was performed to remove the expander, resect the keloid, and repair the expanded skin flap.
Keloids were successfully removed in seven patients using this approach without recurrence. In two patients who had anterior chest keloids, wound healing was prolonged. However, after debridement and re-suturing, the wound healed smoothly without scar hyperplasia.
This method was performed through a keloid incision and with a custom expander embedded. After full expansion, the keloid was directly resected using a linear suture, which avoids new surgical incisions and scars and can successfully remove large-area keloids.
Keloid treatment, especially large keloids, has always been a major problem for surgeons, and this study provides a solution for this problem, which is likely applicable for treating keloids of all sizes and for treating other hypertrophic scars as well.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Laukkanen K, Finland; Maria Villar L, Spain S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Brown JJ, Bayat A. Genetic susceptibility to raised dermal scarring. Br J Dermatol. 2009;161:8-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Ogawa R. Keloid and Hypertrophic Scars Are the Result of Chronic Inflammation in the Reticular Dermis. Int J Mol Sci. 2017;18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 323] [Cited by in F6Publishing: 443] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 3. | Robles DT, Moore E, Draznin M, Berg D. Keloids: pathophysiology and management. Dermatol Online J. 2007;13:9. [PubMed] [Cited in This Article: ] |
| 4. | Lee HJ, Jang YJ. Recent Understandings of Biology, Prophylaxis and Treatment Strategies for Hypertrophic Scars and Keloids. Int J Mol Sci. 2018;19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 247] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 5. | Norris JE. Superficial x-ray therapy in keloid management: a retrospective study of 24 cases and literature review. Plast Reconstr Surg. 1995;95:1051-1055. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Xu J, Yang E, Yu NZ, Long X. Radiation Therapy in Keloids Treatment: History, Strategy, Effectiveness, and Complication. Chin Med J (Engl). 2017;130:1715-1721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Pozzi M, Zoccali G, Drago MC, Mirri MA, Costantini M, DE Vita R. Radiotherapy following surgery in keloid treatment: our protocol. G Ital Dermatol Venereol. 2016;151:492-498. [PubMed] [Cited in This Article: ] |
| 8. | Bijlard E, Kouwenberg CA, Timman R, Hovius SE, Busschbach JJ, Mureau MA. Burden of Keloid Disease: A Cross-sectional Health-related Quality of Life Assessment. Acta Derm Venereol. 2017;97:225-229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Walliczek U, Engel S, Weiss C, Aderhold C, Lippert C, Wenzel A, Hörmann K, Schultz JD. Clinical Outcome and Quality of Life After a Multimodal Therapy Approach to Ear Keloids. JAMA Facial Plast Surg. 2015;17:333-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Radovan C. Tissue expansion in soft-tissue reconstruction. Plast Reconstr Surg. 1984;74:482-492. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 317] [Cited by in F6Publishing: 260] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Austad ED. Evolution of the concept of tissue expansion. Facial Plast Surg. 1988;5:277-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Jones K, Fuller CD, Luh JY, Childs CC, Miller AR, Tolcher AW, Herman TS, Thomas CR Jr. Case report and summary of literature: giant perineal keloids treated with post-excisional radiotherapy. BMC Dermatol. 2006;6:7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Wolfram D, Tzankov A, Pülzl P, Piza-Katzer H. Hypertrophic scars and keloids--a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009;35:171-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 403] [Cited by in F6Publishing: 383] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 14. | Cheraghi N, Cognetta A Jr, Goldberg D. RADIATION THERAPY for the Adjunctive Treatment of Surgically Excised Keloids: A Review. J Clin Aesthet Dermatol. 2017;10:12-15. [PubMed] [Cited in This Article: ] |
| 15. | Kal HB, Veen RE. Biologically effective doses of postoperative radiotherapy in the prevention of keloids. Dose-effect relationship. Strahlenther Onkol. 2005;181:717-723. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Gold MH, Nestor MS, Berman B, Goldberg D. Assessing keloid recurrence following surgical excision and radiation. Burns Trauma. 2020;8:tkaa031. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Matton GE, Tonnard PL, Monstrey SJ, Van Landuyt KH. A universal incision for tissue expander insertion. Br J Plast Surg. 1995;48:172-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Pampena R, Palmieri T, Kyrgidis A, Ramundo D, Iotti C, Lallas A, Moscarella E, Borsari S, Argenziano G, Longo C. Orthovoltage radiotherapy for nonmelanoma skin cancer (NMSC): Comparison between 2 different schedules. J Am Acad Dermatol. 2016;74:341-347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Chander SS. Postoperative radiotherapy in high-risk postmenopausal breast cancer. Lancet. 1999;354:865-6; author reply 866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |