Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5479
Peer-review started: October 21, 2021
First decision: March 3, 2022
Revised: March 15, 2022
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: June 6, 2022
Implant fracture is one of the most serious mechanical complications of dental implants. Conventional treatment necessitates visibility of the apical portion of the fractured implant, whereas for deep and invisible implant fractures, the traditional trephine method has been ineffective. Surgical removal of the marginal bone to expose the fracture surface would be a time-consuming and extensively damaging procedure. Here, we propose a novel technique to address invisible implant fractures.
A 50-year-old woman was referred to our department with the chief complaint that her right mandibular implant tooth had fallen out 3 mo earlier. Cone-beam computed tomography examination showed an implant fracture with a fracture surface 5.1 mm below the crestal ridge. The patient was treated with osteotomy combined with the trephine technique to expose the surgical field and remove the implant. The invisible fractured implant was successfully removed, with minimal trauma. A modified Wafer technique-supported guided bone regeneration treatment was then administered to restore the buccal bone wall and preserve the bone mass. Six months later, fine regenerative bone and a wide alveolar crest in the edentulous area were observed, and a new implant was placed. Four months later, restoration was completed using a cemented ceramic prosthesis. Clinical and radiographic examinations 12 mo after loading fulfilled the success criteria. The patient reported no complaints and was satisfied.
Osteotomy combined with the trephine technique can be effectively used to address deep and invisible implant fractures.
Core Tip: This article provides up-to-date knowledge regarding the clinical presentation, incidence, risk factors, diagnosis, and management of implant fractures. Conventional treatment requires that the apical portion of the fractured implant be visible. For deep and invisible implant fractures, the traditional trephine method has been ineffective. We developed a novel method of osteotomy combined with the trephine technique that can effectively address deep and invisible implant fractures. Meanwhile, modified Wafer technique-supported guided bone regeneration treatment was conducted simultaneously to preserve the bone mass in the surgical area.
- Citation: Chen LW, Wang M, Xia HB, Chen D. Osteotomy combined with the trephine technique for invisible implant fracture: A case report. World J Clin Cases 2022; 10(16): 5479-5486
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5479.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5479
Implant fracture is a kind of destructive mechanical complication, which is generally accompanied by the following clinical characteristics: Loss of retention, marginal bone resorption[1], soft tissue inflammation[2], and occlusal disorder[3]. Consequently, implant fracture can cause significant loss to patients’ economies, time, and emotions. According to research involving large amounts of data and long-term follow-up, the incidence of implant fracture was between 0.4%[4] and 0.92%[5] after over 5 years of loading.
The diagnosis of implant fractures requires the detection of implant mobility by clinical examination and of the fracture line by X-ray images[1]. Once diagnosed as an implant fracture, conventional treatment options are: (1) Complete removal of the remaining fractured implant using trephines[6]; (2) Removal and replacement of the coronal portion of the fractured implant with a new prosthetic restoration[7]; (3) Leaving the remaining apical part integrated into the bone and placing a fixed bridge instead[8,9]; and (4) Using a computer-aided design/computer-aided manufacturing surgical guide to remove the buried implant[10].
However, conventional treatments necessitate visibility of the fractured implant. In case of deep and invisible implant fractures, the position and orientation of the implants are not perceptible. No effective solution has been reported for invisible implant fractures. Surgical removal of the marginal bone to expose the fracture surface could be time-consuming and extensively damaging. Herein, we report a novel method to address invisible implant fractures, as an attempt to form new treatment modalities for such cases. This manuscript was prepared according to the CARE checklist[11].
A 50-year-old non-smoking woman was referred to our clinic in August 2017 with the chief complaint that her mandibular right implant tooth (tooth 46) had fallen out 3 mo earlier.
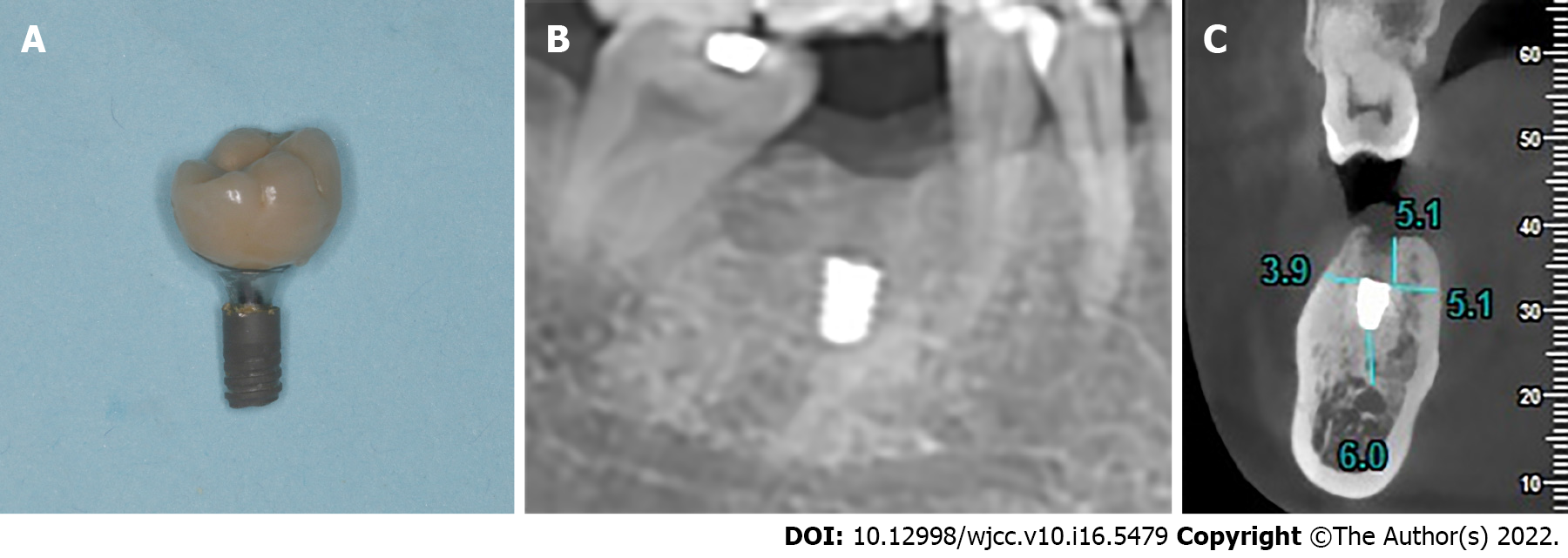
According to the medical record, the implant (Ankylos®, 4.5 mm × 9.5 mm, Germany) was placed in the tooth 46 position in October 2013 and loaded after 6 mo. The patient complained of implant restoration mobility after 2 years of function, with the symptoms worsening while chewing. In May 2017, the patient experienced a foreign body in her mouth, which was the fractured portion of the implant connected to the prosthesis (Figure 1A).
The patient reported no history of systemic diseases, long-term medication, or family genetic history.
No smoking and drinking history, and no hereditary family history were reported.
The patient’s blood pressure was 110/70 mmHg, with a pulse rate of 80 beats per minute (bpm).
The routine blood indicators and coagulation profile were within normal range.
Cone-beam computed tomography (CBCT) examination showed that the residual portion of the implant was osseointegrated with no signs of peri-implantitis. Moreover, there appeared to be a high-density image above the fracture surface of the implant. The remaining apical portion of the implant was 6.0 mm away from the inferior alveolar nerve canal, 3.9 mm away from the buccal cortical bone wall, 5.1 mm away from the lingual bone wall, and 5.1 mm away from the crestal ridge (Figure 1B and C).
The patient was diagnosed with implant fracture.
The risks and benefits of each treatment option were discussed in detail with the patient. The first plan was the fabrication of a three-dimensional (3D) surgical guide for the trephine to achieve precise removal of the remaining implant. However, the 3D surgical guide required at least 20 mm of the trephine with the graduated part, whereas the existing trephines measured only 16 mm. The second plan involved fixed partial restoration, leaving the apical portion of the fractured implant integrated into the bone. However, the patient rejected this plan as she was unwilling to risk damage to her healthy teeth. Consequently, a third treatment plan to perform osteotomy combined with the trephine technique to remove the invisible fractured implant was devised, which was approved by the patient. Informed consent was obtained before treatment.
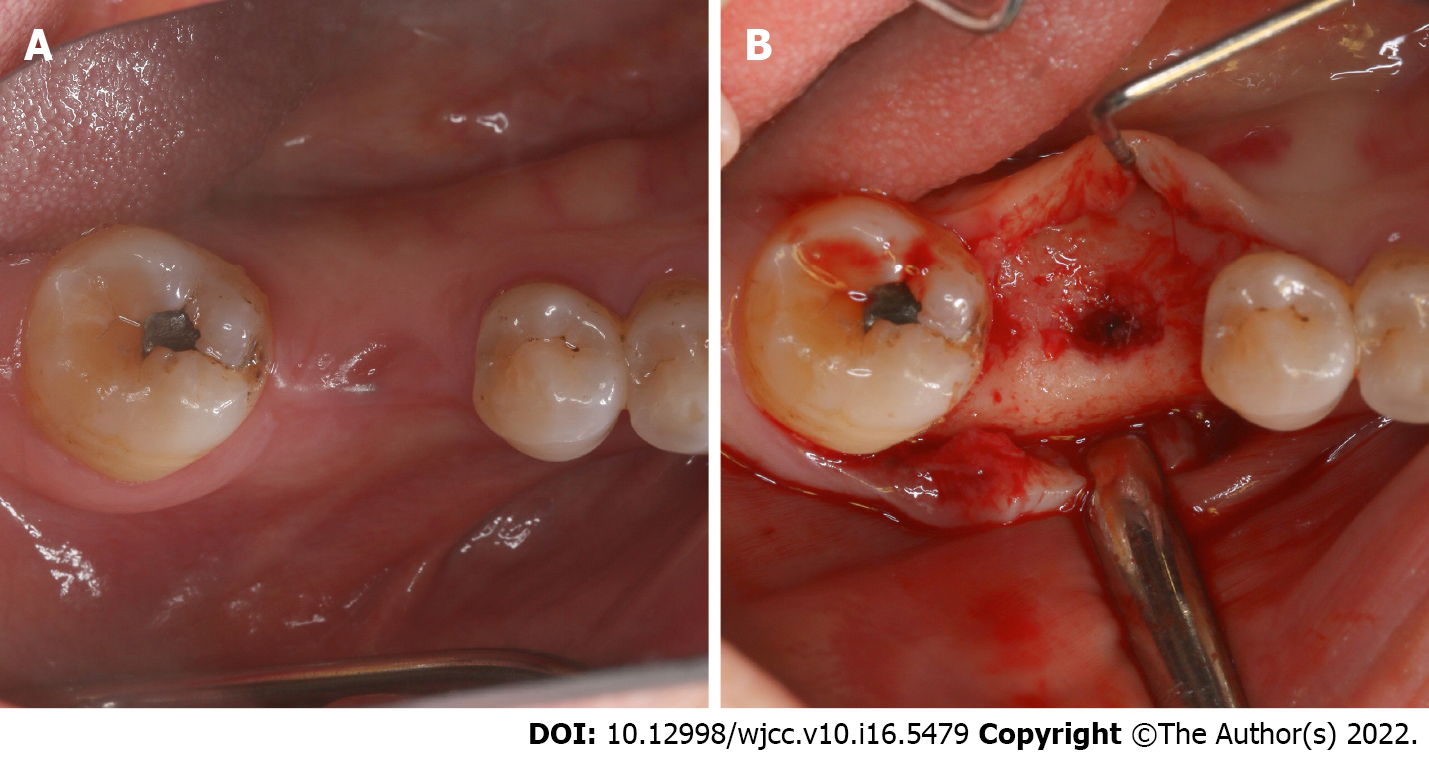
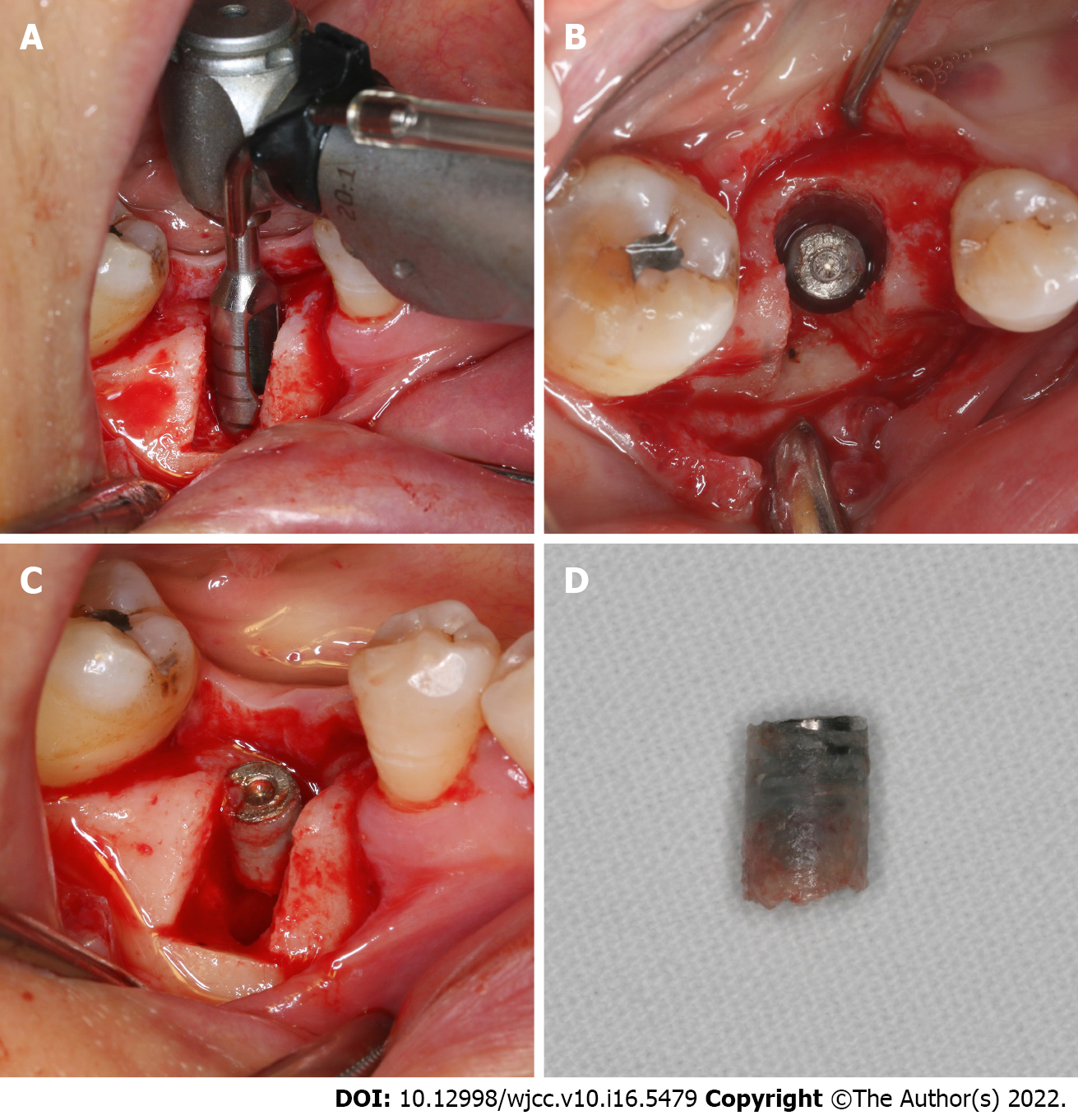
The rapidly growing gingiva had closed the gingival outlet of the implant (Figure 2A). After local anesthesia was administered, a crestal full-thickness flap was raised and an implant hole filled with granulation tissue was observed (Figure 2B). Granulation tissue was removed using a dental excavator and a turbine drill. Thereafter, two vertical incisions and one horizontal incision were made using an ultrasonic osteotome on the buccal side of the alveolar bone where the remaining implant was located (Figure 3A). The buccal bone plate was removed using a bone chisel and hammer (Figure 3B) and soaked in saline temporarily. After the buccal bone plate was removed, the broken end of the fractured implant was clearly exposed (Figure 3C).
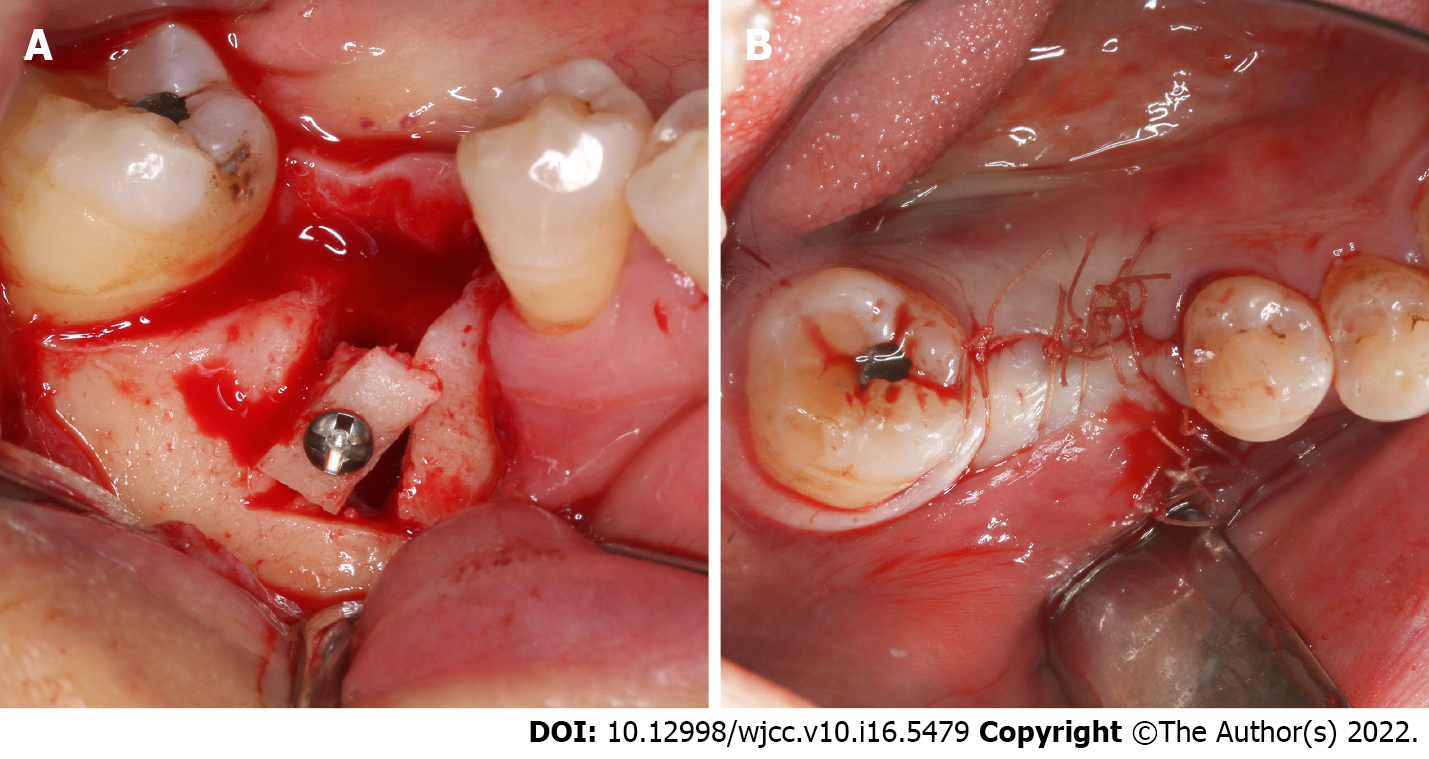
Next, the remaining implant was completely removed with a graduated trephine (Nobel Biocare®, Figure 4A), with the inner diameter of the trephine slightly larger than the outer diameter of the implant. From the occlusal view, a ring of uniform thickness was created around the remaining implant, which did not cause any unnecessary bone defects of the lateral wall and was achieved with minimal bone removal (Figure 4B). The remaining implant was then removed (Figure 4C). The surface of the implant was covered with a thin layer of osseointegrated alveolar bone (Figure 4D). After the surgery, a modified Wafer technique was performed; the buccal bone plate was repositioned in situ using a titanium screw with slight rotation (Figure 5A) to build the external wall of the osteogenic space. Guided bone regeneration (GBR) was performed. The alveolar bone defect was filled with demineralized bovine bone matrix (DBBM; Geistlich Bio-Oss), and the filled defect was covered with a biological membrane (Geistlich Bio-Gide). Finally, the wound was closed up tightly (Figure 5B).
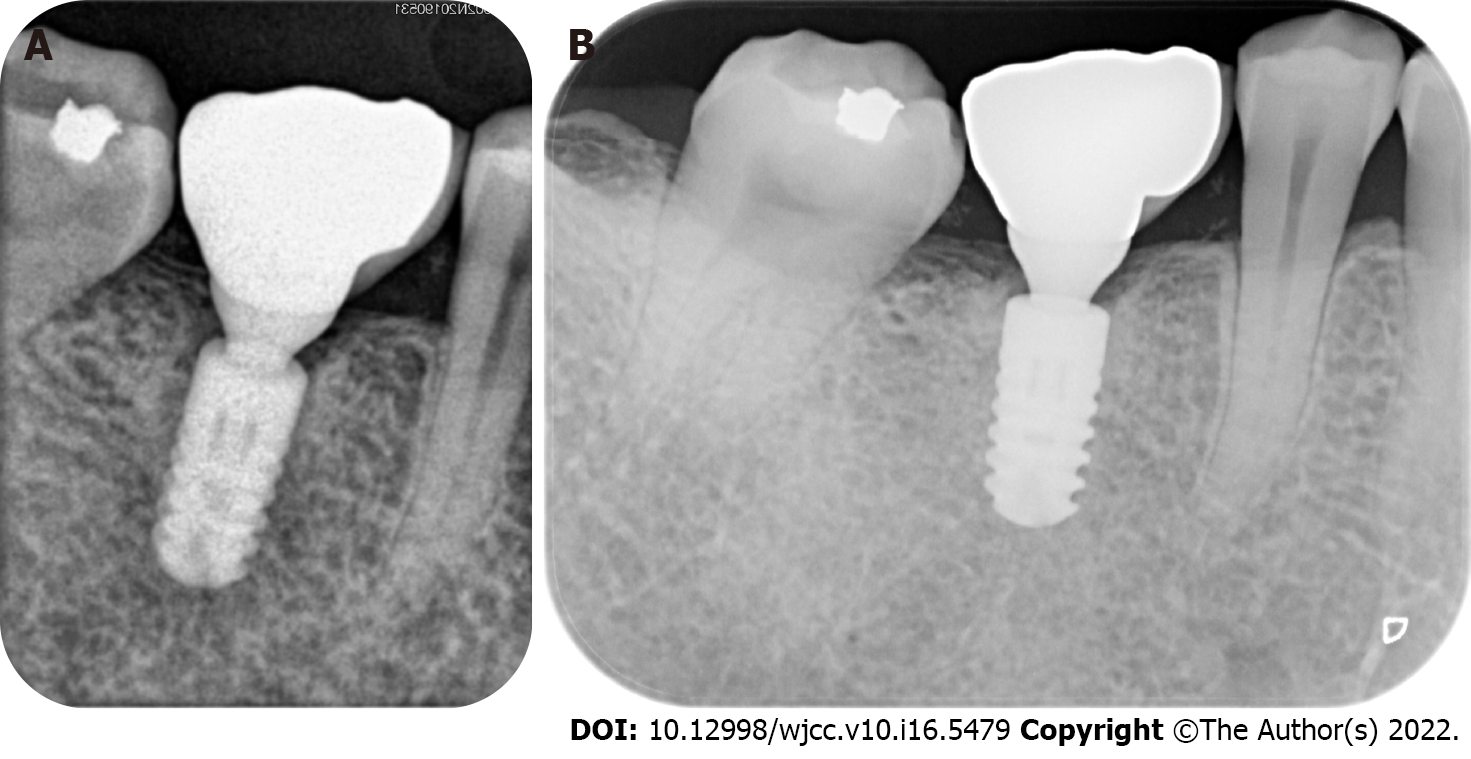
Six months after GBR, fine regenerative bone and wide alveolar crest in the edentulous area were observed. A new implant (Ankylos®, 4.5 mm × 9.5 mm, Germany) was placed in the #30 position. Four months later, restoration was completed using a cemented ceramic prosthesis. Periapical radiographic examination immediately after crown restoration showed a well-osseointegrated implant (Figure 6A). Furthermore, the clinical and radiographic examinations performed 12 mo after loading fulfilled the success criteria outlined by Papaspyridakos et al[13] (Figure 6B)[12,13]. The patient reported no complaints and was very satisfied.
The risk factors for implant fractures remain unclear. The possible risk factors include: (1) Implant diameter and length[5,14]—it is considered that the smaller the diameter, the lower the resistance of the implant to fracture; (2) Implant location (i.e., type of bone)[5,15,16], as implants placed in the anterior or premolar region bear less mechanical overloading than those in the posterior region; (3) Direct adjacency to cantilever[17]; (4) Parafunctional habits (teeth clenching and bruxism)[9,18]; and (5) Patient-related factors (smoking and alcohol intake)[19,20].
This case presents a novel method for managing invisible implant fractures. In brief, buccal bone plate osteotomy was conducted at the fractured implant site, followed by complete removal of the implant with a trephine to achieve minimal trauma. Subsequently, the modified Wafer technique was used to preserve the horizontal alveolar dimension. It is worth mentioning that the incision of the buccal bone plate was based on the CBCT results. Accurate osteotomy depth control was achieved by marking the ultrasonic osteotome in advance. In the present case, the surface of the removed implant was covered with a thin layer of osseointegrated alveolar bone. It was assumed that the trephine did not cut into the implant, and no titanium particles remained in the operation area.
The use of cortical bone plate supported GBR for bone mass preservation was inspired by the 3D bone reconstruction technique named the Bilaminar cortical tenting grafting technique proposed by Yu et al[21] and the Wafer technique proposed by Merli et al[22] According to the bilaminar cortical tenting grafting technique, an autogenic bone block is bisected into two cortical laminae to construct the buccal and palatal walls of an alveolar ridge defect, and the inter-laminar space is filled with bone graft. In the Wafer technique, an autogenous plate is horizontally harvested and vertically fixed, partially supported by the residual bone wall, and the biomaterial is filled in. Both the techniques provide sufficient bone mass. We used the modified Wafer technique at the implant removal defect site to reconstruct the horizontal alveolar dimension, with the buccal bone plate obtained from the bone defect, thus avoiding a second surgical area[23].
Osteotomy combined with the trephine technique has many advantages in addressing deep and invisible implant fractures. This procedure avoids excessive bone removal or titanium particles, which can affect wound healing. The limitation of this technique is that immediate implantation cannot be achieved owing to insufficient primary stability. Therefore, this technique must be used in conjunction with delayed implantation, which is more time-consuming.
This article proposes a novel osteotomy combined with the trephine technique, which effectively addressed an invisible implant fracture 5.1 mm beneath the alveolar crest. In addition, this article provides up-to-date knowledge regarding the clinical presentation, incidence, risk factors, diagnosis, and management of dental implant fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papotto G, Italy S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Liaw K, Delfini RH, Abrahams JJ. Dental Implant Complications. Semin Ultrasound CT MR. 2015;36:427-433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:2-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 554] [Cited by in F6Publishing: 557] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 3. | Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19:119-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 666] [Cited by in F6Publishing: 599] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 4. | Lee JH, Kim YT, Jeong SN, Kim NH, Lee DW. Incidence and pattern of implant fractures: A long-term follow-up multicenter study. Clin Implant Dent Relat Res. 2018;20:463-469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Lee DW, Kim NH, Lee Y, Oh YA, Lee JH, You HK. Implant fracture failure rate and potential associated risk indicators: An up to 12-year retrospective study of implants in 5,124 patients. Clin Oral Implants Res. 2019;30:206-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 6. | Balshi TJ. An analysis and management of fractured implants: a clinical report. Int J Oral Maxillofac Implants. 1996;11:660-666. [PubMed] [Cited in This Article: ] |
| 7. | Jin SY, Kim SG, Oh JS, You JS, Jeong MA. Incidence and Management of Fractured Dental Implants: Case Reports. Implant Dent. 2017;26:802-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Sánchez-Pérez A, Moya-Villaescusa MJ, Jornet-Garcia A, Gomez S. Etiology, risk factors and management of implant fractures. Med Oral Patol Oral Cir Bucal. 2010;15:e504-e508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Gealh WC, Mazzo V, Barbi F, Camarini ET. Osseointegrated implant fracture: causes and treatment. J Oral Implantol. 2011;37:499-503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Deeb G, Koerich L, Whitley D 3rd, Bencharit S. Computer-guided implant removal: A clinical report. J Prosthet Dent. 2018;120:796-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67:46-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 339] [Cited by in F6Publishing: 363] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 12. | Vozza I, Barone A, Quaranta M, De Paolis G, Covani U, Quaranta A. A comparison between endodontics and implantology: an 8-year retrospective study. Clin Implant Dent Relat Res. 2013;15:29-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012;91:242-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 338] [Cited by in F6Publishing: 349] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 14. | Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Factors influencing the fracture of dental implants. Clin Implant Dent Relat Res. 2018;20:58-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Miyamoto I, Takahashi T, Tanaka T, Hirayama B, Tanaka K, Yamazaki T, Morimoto Y, Yoshioka I. Dense cancellous bone as evidenced by a high HU value is predictive of late implant failure: a preliminary study. Oral Radiol. 2018;34:199-207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 16. | Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants. 1995;10:326-334. [PubMed] [Cited in This Article: ] |
| 17. | Zurdo J, Romão C, Wennström JL. Survival and complication rates of implant-supported fixed partial dentures with cantilevers: a systematic review. Clin Oral Implants Res. 2009;20 Suppl 4:59-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Anitua E, Saracho J, Almeida GZ, Duran-Cantolla J, Alkhraisat MH. Frequency of Prosthetic Complications Related to Implant-Borne Prosthesis in a Sleep Disorder Unit. J Oral Implantol. 2017;43:19-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Rani S, Devi J, Verma M. Implant success lies in complications management: A report of two cases. Contemp Clin Dent. 2016;7:226-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Sridhar S, Abidi Z, Wilson TG, Jr. , Valderrama P, Wadhwani C, Palmer K and Rodrigues DC. In Vitro Evaluation of the Effects of Multiple Oral Factors on Dental Implants Surfaces. J Oral Implantol. 2016;42:248-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 21. | Yu H, Chen L, Zhu Y, Qiu L. Bilamina cortical tenting grafting technique for three-dimensional reconstruction of severely atrophic alveolar ridges in anterior maxillae: A 6-year prospective study. J Craniomaxillofac Surg. 2016;44:868-875. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Merli M, Moscatelli M, Mariotti G, Motroni A, Mazzoni A, Mazzoni S, Breschi L, Nieri M. A Novel Approach to Bone Reconstruction: The Wafer Technique. Int J Periodontics Restorative Dent. 2017;37:317-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Xia HB, Zhang YF, Shi B, Wang M. Two bone blocks sandwich technique for horizontal reconstruction of severely atrophic alveolar ridge in anterior maxilla: A case report. World J Clin Cases. 2020;8:971-979. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |