Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5208
Peer-review started: August 8, 2021
First decision: January 10, 2022
Revised: January 19, 2022
Accepted: April 2, 2022
Article in press: April 2, 2022
Published online: June 6, 2022
Intraventricular hemorrhage is a neurosurgical emergency, and a dangerous condition associated with high morbidity and mortality. Previously, hematoma evacuation is generally executed by external intracranial drainage (EVD) or surgical evacuation. Nowadays, endoscopic evacuation is emerging as a good alternative because it brings relatively less invasion and injury. However, successful endoscopic evacuation requires skilled manipulation of endoscopic devices and the evidence supporting its efficacy differs in different reports.
To improve the technique usage and provide more evidence of endoscopic evacuation efficacy, we summarize our surgical experience and compared the outcomes of the endoscopic evacuation with EVD using real-world data.
We retrospectively studied 96 consecutive patients with intraventricular hemor
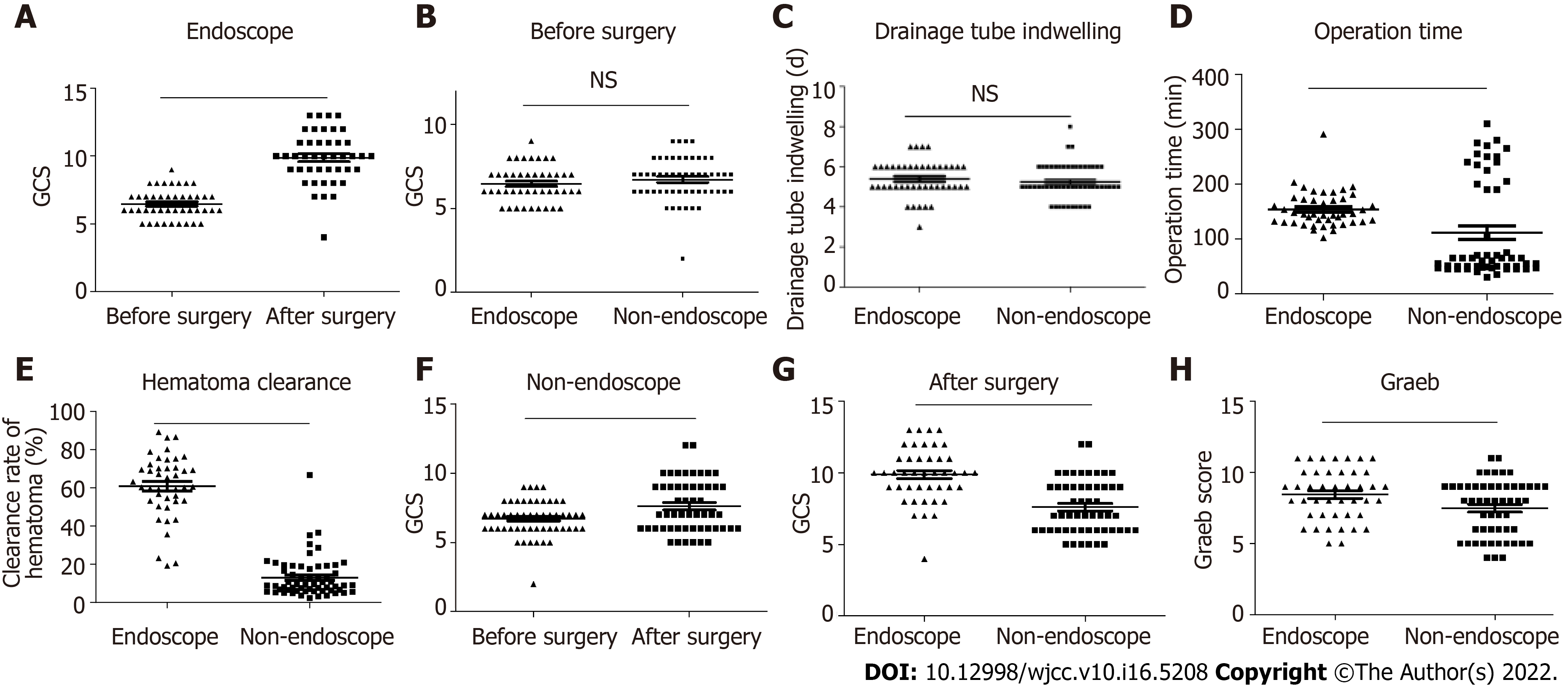
Patients in the endoscopic and non-endoscopic groups presented with a similar state of consciousness, with a comparable Glasgow Coma Scale (GCS) index. The average operation time of the endoscopic group was longer than that of the non-endoscopic group (median 2.42 h vs 1.08 h, P < 0.001). Although the endoscopic group was older and had a baseline Graeb score that indicated more severe hemorrhage than the non-endoscopic group (Graeb median: Endoscopic group = 9 vs non-endoscopic group = 8, P = 0.023), the clearance rate of hematoma was as high as 60.5%. Both the endoscopic and non-endoscopic groups showed an improved GCS index after surgery. However, this improvement was more marked in patients in the endoscopic group (median improvement of GCS index: Endoscope group = 4 vs non-endoscopic group = 1, P < 0.001). Additionally, the endoscopic group had a lower Graeb score than the non-endoscopic group after the operation. The intensive care unit stay of the endoscopic group was significantly shorter than that of the non-endoscopic group (median: endoscopic group = 6 d vs non-endoscope group = 7 d, P = 0.017).
Endoscopic evacuation of intraventricular hemorrhage was generally an effective and efficient way for hemorrhage evacuation, and contributed remarkably to the improvement of consciousness in patients with intraventricular hemorrhage.
Core Tip: Endoscopic evacuation is a minimally invasive technique used to treat intraventricular hemorrhage. However, skilled manipulation is required when applying the technique, the evidence supporting its efficacy differs in different reports. Here, we present our experience in patients with intraventricular hemorrhage who underwent endoscopic intraventricular hematoma evacuation, and compared the efficacy of the technique with traditional external ventricular drainage using real-world data. The results indicate that endoscope evacuation was effective and efficient for treating intraventricular hemorrhage, and led to a higher rate of hemorrhage evacuation and a more remarkable recovery in consciousness than patients who underwent non-endoscopic surgery.
- Citation: Wang FB, Yuan XW, Li JX, Zhang M, Xiang ZH. Endoscopic surgery for intraventricular hemorrhage: A comparative study and single center surgical experience. World J Clin Cases 2022; 10(16): 5208-5216
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5208.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5208
Intraventricular hemorrhage (IVH) is a neurosurgical emergency, and a dangerous condition associated with high morbidity and mortality[1]. IVH in adults generally results from aneurysm rupture, trauma, vascular malformation and tumor (primary causes), or entrance of intracranial hemorrhage into the ventricle system (secondary cause)[2]. In such cases, it is essential to evacuate the hematoma and normalize intracranial pressure. Hematoma evacuation is generally executed by external intracranial drainage or surgical evacuation, but endoscopic evacuation is emerging as a good alternative[3].
Endoscopic evacuation is a minimally invasive technique for IVH treatment, and has been reported to efficiently improve surgery outcomes[4]. However, successful endoscopic evacuation requires skilled manipulation of endoscopic devices. Here, we present in detail our experience in 43 patients with IVH who underwent endoscopic intraventricular hematoma evacuation and catheter drainage of residual hematoma. Surgery outcomes were generally satisfactory, and we believe that our experience of IVH surgery may constructively improve the clinical practice of endoscopic evacuation.
We retrospectively enrolled patients diagnosed with IVH and underwent endoscopic surgery or external ventricular drainage (EVD) surgery between November 2013 and September 2019 in Xinyi People’s hospital (Jiangsu province). The inclusion criteria were as follows: (1) 15–80 years of age; (2) with clinical signs of moderate to severe IVH; (3) Head computed tomography (CT) images showed the existence of hemorrhage breaking into the third and fourth ventricles or primary IVH; and (4) A Glasgow Coma Scale (GCS) score < 10. Patients over 80 years old, with any anticoagulation/anti-aggregation-related bleeding, a serious disease in other major organs or systems, or who rejected the surgery treatment were excluded. Generally, the treatment choice was made based on integrating surgeons’ experience, CT appearance, and the patient’s clinical conditions and financial situation. Finally, a total of 96 patients were studied; of these, 43 received endoscopic surgery and 53 underwent EVD surgery. The conscious states of all patients were assessed using the GCS[5] upon admission. The Graeb score was used to assess the severity of hemorrhage[6]. The Graeb score components are as follows: Each lateral ventricle, 1 = trace of blood, 2 = less than 50% filled, 3 = more than 50% filled, 4 = completely filled and expanded (each lateral ventricle was assessed individually); third and fourth ventricles, 0 = no blood, 1 = blood present and size normal, 2 = filled with blood and expanded. The total score was 12.
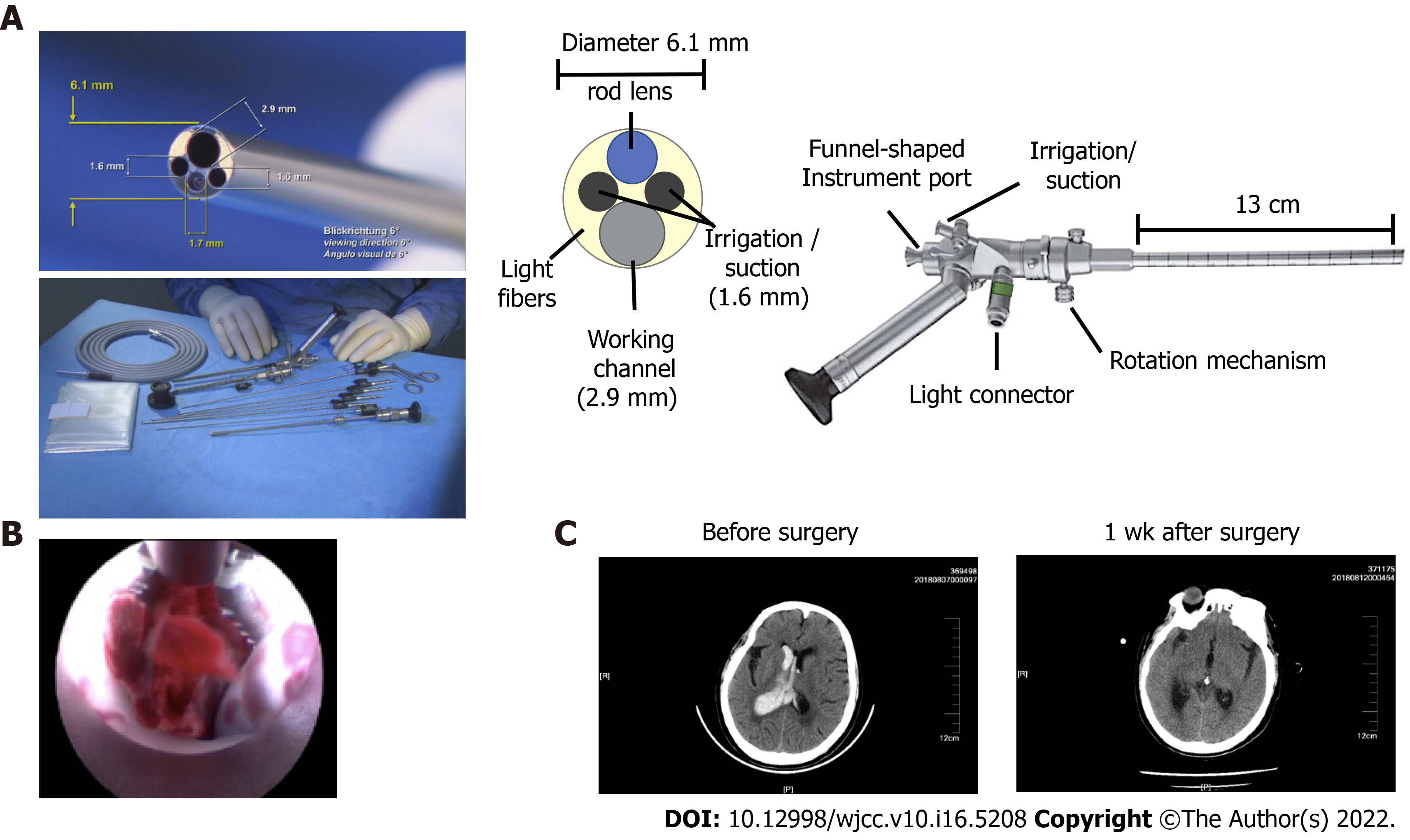
A KARL STORZ high-resolution ventriculoscopic system was used. The 6° 28164 LA LOTTA ventriculoscope was 6.1 mm in outside diameter and 18 cm in length, with a 2.9 mm working channel and two 1.6 mm irrigation/suction channels (Figure 1A). The working sheath was 6.8 mm for the outside diameter and 13.3 cm long A holding arm was used to hold and stabilize the ventriculoscope.
All procedures were performed while patients were under general anesthesia in the supine position. The procedures began from the side with the least hemorrhage. At 3 cm posterior to the hairline and 2.5 cm lateral to the midline, a 3 cm scalp incision parallel to the midline was made. A 1.2 cm burr hole was made at the midpoint of the incision. After hemostasis, a cross-shape incision of the dura mater was made. Then, a drainage catheter (O.D. 4 mm) was inserted perpendicularly to the surface of the brain into the lateral ventricle. Generally, bloody cerebrospinal fluid flowed out when the catheter reached a depth of 5 cm-6 cm inside the brain. Then, the catheter was removed, and the working sheath (with an obturator) was placed carefully through the trajectory of the catheter. After reaching the lateral ventricle, the sheath was advanced 0.5 cm deeper. Then, the obturator was removed and the ventriculoscope was placed into the lateral ventricle frontal horn through the working sheath.
Normal saline (23 ℃-25 ℃) was continuously infused through one of the irrigation/suction channels and drained from the other one to irrigate the lateral ventricle. Visible hematomas were aspirated through the irrigation/suction channel or the working channel, and removal of hematomas in the third ventricle was conducted if necessary. When blood clots could not be removed by aspiration, or an important ventricular structure was suspected to be beneath the clots, forceps were advanced through the working channel to pull out the clot (Figure 1B). A bipolar coagulation electrode was used to stop active hemorrhages. Finally, the ventriculoscope and the working sheath were slowly removed while avoiding injuring brain tissue along the trajectory. A ventricular drainage catheter was inserted before closing the scalp incision. The same procedure was repeated on the other side. A head CT scan was conducted immediately after the surgery (Figure 1C). If there was residual hematoma in the fourth ventricle, ventricular irrigation was performed by pumping 40000 IU urokinase and 100 mL normal saline through the drainage catheter at 4.3 mL/h. Patients were followed up to monitor the occurrence of complications, including hydrocephalus.
Continuous variables with normally distributed data are presented as the mean ± SD, and were compared using t-tests. Non-normally distributed data are presented as the median and interquartile range (IQR), and were compared using the nonparametric Kruskal–Wallis test. Categorical variables are expressed as absolute numbers with percentages, and were compared using Chi-square tests. A two-tailed P < 0.05 was considered as statistically significant. All statistical analyses were performed using SPSS 22.0 (IBM SPSS Statistics, IBM, Chicago, IL, United States) and GraphPad Prism (version 7.0; GraphPad Software, Inc, San Diego, CA, United States).
Twenty (46.51%) and twenty-two (41.51%) men were included in the endoscopic and EVD groups, respectively, and the two groups did not show a significant difference in sex distribution. Patients in the endoscopic group were significantly older than those in the EVD group [endoscopic group: (median, IQR) 60.40 ± 9.55 years; EVD group: 55.34 ± 12.17 years]. The preoperative GCS score was comparable between the two groups (Table 1). The total ventricular hemorrhage and hematoma into the third and fourth ventricles (blood volume ≥ 30 mL) were regularly recorded by head CT scans (Figure 1C). Among all patients, 12 had a pre-operative history of hypertension and 2 had a history of moyamoya disease. Compared with the non-endoscopic group, the baseline Graeb score was higher in the endoscopic group, which indicated more severe hemorrhage.
| Metrics | Endoscopic group | Non-endoscopic group | P value |
| Baseline | |||
| Age, yr | 60.40 ± 9.55 | 55.34 ± 12.71 | 0.033 |
| Sex (male), n % | 20 (46.51%) | 22 (41.51%) | 0.623 |
| Pre-operative GCS score | 6.00 (6.00-7.00) | 7.00 (6.00-8.00) | 0.216 |
| Graeb score | 9.00 (7.00-10.00) | 8.00 (6.00-9.00) | 0.023 |
| Perioperative | |||
| Operation time, hours | 2.42 (2.17-2.88) | 1.08 (0.82-3.33) | < 0.001 |
| Hematoma clearance rate, % | 60.50% (53.20%-70.40%) | 10.20% (6.60%-18.90%) | < 0.001 |
| GCS score improvement | 4.00 (2.00-4.50) | 1.00 (-1.00-2.00) | < 0.001 |
| Drainage, d | 5.00 (5.00-6.00) | 5.00 (5.00-6.00) | 0.288 |
| ICU stay, d | 6.00 (3.00-9.00) | 7.00 (5.00-10.00) | 0.017 |
| Hospitalization time, d | 26.00 (18.50-33.00) | 26.00 (19.00-40.00) | 0.292 |
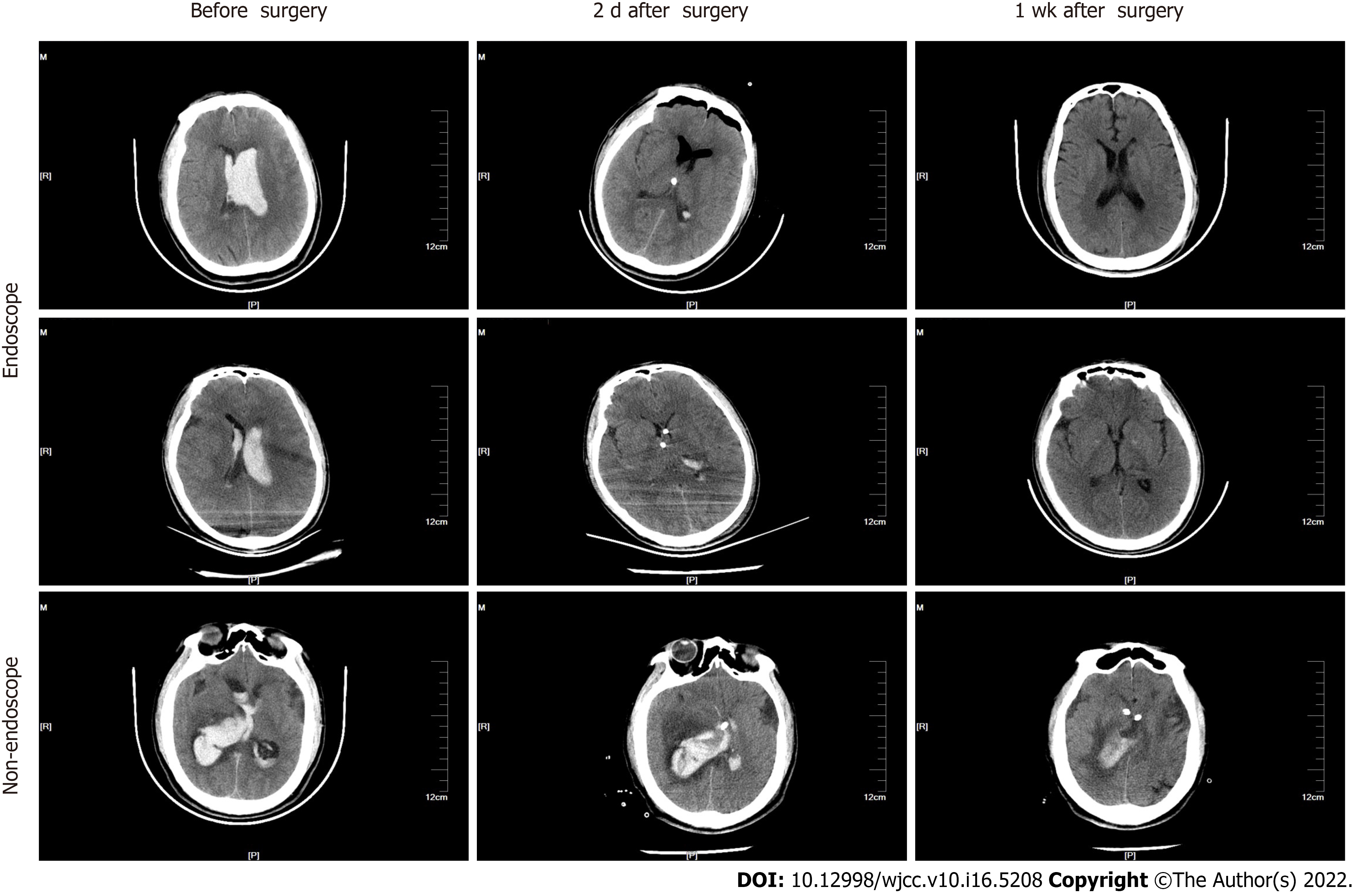
The median operation time was 2.42 h and 1.08 h for the endoscopic and EVD groups, respectively (Table 1). During the endoscopic operation, conversion to craniotomy was necessary in 10 cases (23.3%) (including 5 patients with moyamoya disease, 2 with aneurysm ruptures at the basilar artery junction, and 3 with hypertensive intracerebral hemorrhage in the basal ganglia) as a result of intraoperative massive hemorrhage. Eight (18.6%) patients with hypertensive intracerebral hemorrhage had a history hematoma evacuation by craniotomy before endoscopic evacuation, and their hematoma volumes were over 30 mL. The ventricular hemorrhage and hematoma in the endoscopic group were evaluated by head CT scans before and after surgery (Figure 2). The average clearance rate of the hematoma was 60.5% in the endoscopic group, and only 10.2% in the EVD group (Table 1).
In the short term, 28 (65%) patients in the endoscopic group showed marked improvement in conscious states, with a mean GCS score increase of more than 3. Five patients (11.7%) had postoperative communicating hydrocephalus and were cured by ventriculoperitoneal shunt. No other complications, such as intracranial infection, were observed in any patients. In the long term, consciousness was restored in most patients, as revealed by increased GCS scores after surgery (Figure 3A and Table 1).
The total ventricular hemorrhage and hematoma in the non-endoscopic group were visualized using head CT scans before and after surgery (Figure 2, lower panel). Drainage tube indwelling time (Figure 3C and Table 1) was comparable between the endoscopic and non-endoscopic groups. Despite a longer operation time, older age, and more serious hemorrhage, the endoscopic surgery dramatically improved the clearance rate of hematoma (Figure 3D). The endoscopic group had a longer operation time than the non-endoscopic group (Figure 3E). Although both groups exhibited an increased GCS after surgery (Figure 3A and 3F), the endoscopic group had a higher GCS index than the non-endoscopic group after surgery (Figure 3G and Table 1), which indicates that endoscopic surgery for IVH contributed to the recovery of consciousness. In addition, the endoscopic group showed a lower Graeb score than the non-endoscope group after surgery (Figure 3H), which suggests that endoscopic surgery leads to more successful hemorrhage evacuation. Finally, although there was no significant difference in hospitalization time between the two groups, the intensive care unit stay of the endoscopic group was shorter than that of the EVD group (Table 1).
In this paper, we present our experience of treating patients with IVH using endoscopic surgery, and compared their perioperative metrics with patients who received traditional EVD surgeries. We found that endoscopic evacuation was effective and efficient for treating IVH. Furthermore, endoscopic surgery led to a higher rate of hemorrhage evacuation and more marked consciousness recovery compared with the non-endoscopic surgery group. Herein, we will combine clinical evidence, our clinical experience, and previous publications to discuss the key factors for hemorrhage evacuation using the endoscopic approach.
IVH can induce a cascade of lethal symptoms. Cerebrospinal fluid circulation obstruction by hemorrhage clots in the third and fourth ventricles leads to drastic elevation of intracranial pressure and loss of consciousness. Blood clots and breakdown products compress and squeeze the hypothalamus and brain stem, resulting in multiple organ dysfunction. Immediate clearance of intraventricular blood is the key to an improved prognosis[7]. Currently, many methods are available for the evacuation of IVH, such as catheter drainage with or without fibrinolytic therapy, neurosurgical evacuation, and minimally invasive endoscopic surgery. A recent meta-analysis[8] has reported that endoscopic evacuation is more favorable than catheter drainage. However, other researchers claim that the latter is more favorable[4,9]. Moreover, with the help of more accurate instruments and neuronavigation methods, endoscopic hematoma evacuation can be conducted under the guidance of visualization of ventricles. Previous reports have shown that patients with IVH treated by endoscopic management tend to have more favorable outcomes, a shorter recovery time[3,7,10], and a lower incidence of infection[11]. Generally, subdural effusion, intraventricular hemorrhage and infection are the main complications in endoscopic procedure, which is similar with conventional indwelling ventricular drainage tube operation. However, as with the application of endoscopic methods in other fields, the techniques and experiences of surgeons have great impacts on the efficacy and outcome of ventricular endoscopic surgery. Subdural effusion always occurs during the operation of intraventricular lesions, which cases needed drilling and drainage. When the thick intraventricular endoscope entering ventricle from the cortex, it is equivalent to ventriculostomy. Cerebrospinal fluid flow from the ventricle to the subdural canal caused by the endoscope, resulting in subdural effusion, and few patients could heal themselves. It is worth noting that the rate of communicating hydrocephalus was relatively low (11.7%) in our study. Blood residue in the ventricles after intracranial hemorrhage evacuation is a risk factor for communicating hydrocephalus[12], which suggested that the evacuation was effective.Intraventricular endoscopic surgery is an operation with high aseptic requirements, which need the instruments be strictly disinfected, and the aseptic operation should be strictly carried out during the operation. It is best to use antibiotics before the operation. In our series, no patients showed signs of intracranial infection. Effective prevention of infection may have been done because the drainage was completed within 3 d in our series. Therefore, our operation method greatly prevents the occurrence of complications, and has operability and safety.
We have summarized several features of our experience in surgical techniques. First, the frontal horn of the lateral ventricle is a safer trajectory towards lesions in the lateral ventricle in intracranial procedures[13], which was effective and less traumatic in our patients. Meanwhile, careful positional adjustments of the ventriculoscope could help to improve the efficacy and safety of hematoma evacuation. Second, clearing the visual field increased the accuracy of hematoma removal. The vision of the endoscope was often blurred by bloody cerebrospinal fluid as the endoscope entered the lateral ventricle. The incidence of injury may significantly increase without clear vision, and blind manipulation under blurred or “red-out” endoscopic vision is not recommended[14]. Thus, we used normal saline to displace the bloody cerebrospinal fluid before aspiration. Intraoperative hemorrhage can also obscure the endoscope vision, so continuous rinsing and avoiding blind operation are particularly important issues to highlight. In addition, the endoscope can be interfered with by hemorrhages from small vessels on the puncture trajectory and damaged choroid plexus and ventricular walls, which can usually be attenuated or prevented by rinsing, which is consistent with previous reports[15,16]. After regaining a clear vision, the hemorrhagic spots can be identified and cauterized with a bipolar coagulation electrode to stop bleeding.
We considered navigation to be necessary at the beginning of the surgery since the loss of cerebrospinal fluid during an evacuation may cause a position shift of the brain. Moreover, given that rinsing ensures a better visibility in the ventricle, the endoscopy can be more precisely navigated to avoid damaging the brain. Therefore, performing endoscopy in the center of the hematoma is not necessary.
The irrigation fluid used was normal saline (23 ºC -25 ºC) at 5 cm -10 cm H2O, which is not consistent with other authors who have claimed that artificial cerebrospinal fluid is the better choice for irrigation[17-19]. The use of low-temperature saline should indeed be avoided in infants[20]. However, there is no evidence to suggest that normal saline is more harmful than irrigation fluid in adults, and, considering accessibility, we used normal saline in our series. No irrigation-related intraoperative or postoperative side effects were observed.
Three patients had an intraoperative massive hemorrhage, which is a challenge in neurological procedures[21]. A conversion to craniotomy was conducted to manage intraoperative hemorrhage in these cases. All three patients exhibited large volumes of red bloody fluid and intracranial hypertension (elevated blood pressure and pulse pressure), compared with the previously mentioned minor hemorrhage. Massive hemorrhage cannot be stopped by irrigation. Based on our experience, we suggest that a large hematoma volume and significant brain position shift after hematoma evacuation are likely to be signs of an intraoperative massive hemorrhage, in which case craniotomy should be considered.
This study has some limitations, such as the small sample size and the retrospective nature of the study. Future prospective studies with a larger series are required to further confirm the efficacy and safety of endoscopic evacuation.
Our study showed that endoscopic evacuation of IVH was generally effective and efficient. The included patients showed significant improvement in consciousness, long-term recovery, and the Graeb index. In addition, this research demonstrates our preliminary experience in practicing endoscopic evacuation.
Intraventricular hemorrhage (IVH) is a neurosurgical emergency, and a dangerous condition associated with high morbidity and mortality. In traditional treatment, hematoma evacuation is generally executed by external intracranial drainage (EVD) or surgical evacuation,but endoscopic evacuation is emerging as a good alternative approach, which brings relatively less invasion and injury. Accordingly, we need more successful endoscopic evacuation skilled experience to support endoscopic evacuation deve
With the development of endoscopic evacuation approach in Intraventricular hemorrhage therapy,we need more successful endoscopic evacuation skilled manipulation of endoscopic devices and the evidence supporting its efficacy differs. Thus, in this research, we retrospectively studied 96 consecutive patients with intraventricular hemorrhage who underwent either endoscopic surgery or non-endoscopic surgery for hemorrhage evacuation in different reports, which could provide guidance for endoscopic evacuation treatment in IVH.
In this research, we try to improve the technique usage and provide more evidence of endoscopic evacuation efficacy. Besides, we summarize our surgical experience and compared the outcomes of the endoscopic evacuation with EVD using real-world data.
We retrospectively studied 96 consecutive patients with intraventricular hemorrhage who underwent either endoscopic surgery (n = 43) or non-endoscopic surgery (n = 53) for hemorrhage evacuation between November 2013 and September 2019 in our center. Patients’ conditions prior to and after the operation were evaluated and analyzed to assess the efficacy of the operation. The consciousness status improvement and perioperative in-hospital parameters in the two types of operation groups were assessed and compared.
Patients in the endoscopic and non-endoscopic groups presented with a similar state of consciousness, with a comparable Glasgow Coma Scale (GCS) index. It was found that the average operation time was longer in the endoscopic group; the endoscopic group had a baseline Graeb score that indicated more severe hemorrhage than the non-endoscopic group, and the clearance rate of hematoma was as high as 60.5%. In the endoscopic group, the improved GCS index was more marked. Besides, the intensive care unit stay of the endoscopic group was significantly shorter than that of the non-endoscopic group.
Endoscopic evacuation of intraventricular hemorrhage was generally an effective and efficient way for hemorrhage evacuation, and contributed remarkably to the improvement of consciousness in patients with intraventricular hemorrhage, which could be a potential surgical methods to be developed.
In our retrospective analysis, our study showed that endoscopic evacuation of IVH was generally effective and efficient. The included patients showed significant improvement in consciousness, long-term recovery, and the Graeb index. This research provides us more preliminary experience in practicing endoscopic evacuation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anandan H, India; Chiu KW, Taiwan S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Garton T, Hua Y, Xiang J, Xi G, Keep RF. Challenges for intraventricular hemorrhage research and emerging therapeutic targets. Expert Opin Ther Targets. 2017;21:1111-1122. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Zhang S, Jia B, Li H, You C, Hanley DF, Jiang Y. Primary intraventricular hemorrhage in adults: etiological causes and prognostic factors in Chinese population. J Neurol. 2017;264:382-390. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Ma L, Hou Y, Zhu R, Chen X. Endoscopic Evacuation of Basal Ganglia Hematoma: Surgical Technique, Outcome, and Learning Curve. World Neurosurg. 2017;101:57-68. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Song P, Duan FL, Cai Q, Wu JL, Chen XB, Wang Y, Huang CG, Li JQ, He ZQ, Huang QC, Liu M, Zhang YG, Luo M. Endoscopic Surgery vs External Ventricular Drainage Surgery for Severe Intraventricular Hemorrhage. Curr Med Sci. 2018;38:880-887. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Green SM, Haukoos JS, Schriger DL. How to Measure the Glasgow Coma Scale. Ann Emerg Med. 2017;70:158-160. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Romero JM, Rosand J. Hemorrhagic cerebrovascular disease. Handb Clin Neurol. 2016;135:351-364. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Ceja Espinosa A, Franco Jimenez JA, Reyes Vazquez P, Gutierrez Aceves GA, Ponce Ayala A. Endoscopic Third Ventriculostomy for Obstructive Hydrocephalus Secondary to Delayed Intracerebellar Hematoma. Cureus. 2021;13:e17302. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Kellner CP, Song R, Ali M, Nistal DA, Samarage M, Dangayach NS, Liang J, McNeill I, Zhang X, Bederson JB, Mocco J. Time to Evacuation and Functional Outcome After Minimally Invasive Endoscopic Intracerebral Hemorrhage Evacuation. Stroke. 2021;52:e536-e539. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Xiao T, Wan J, Qu H, Jiang W, Zhou X. Endoscopic Surgery vs Minimal Puncture Drainage Surgery for Treatment of Supratentorial Intracerebral Hemorrhage. Turk Neurosurg. 2020;30:565-572. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Oertel J, Linsler S, Csokonay A, Schroeder HWS, Senger S. Management of severe intraoperative hemorrhage during intraventricular neuroendoscopic procedures: the dry field technique. J Neurosurg. 2018;131:931-935. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Wellons JC 3rd, Shannon CN, Holubkov R, Riva-Cambrin J, Kulkarni AV, Limbrick DD Jr, Whitehead W, Browd S, Rozzelle C, Simon TD, Tamber MS, Oakes WJ, Drake J, Luerssen TG, Kestle J; Hydrocephalus Clinical Research Network. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr. 2017;20:19-29. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Yang WS, Shen YQ, Zhang XD, Zhao LB, Wei X, Xiong X, Xie XF, Li R, Deng L, Li XH, Lv XN, Lv FJ, Li Q, Xie P. Hydrocephalus Growth: Definition, Prevalence, Association with Poor Outcome in Acute Intracerebral Hemorrhage. Neurocrit Care. 2021;35:62-71. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Avinash KS, Thakar S, Ghosal N, Hegde AS. Anaplastic hemangiopericytoma in the frontal horn of the lateral ventricle. J Clin Neurosci. 2016;26:147-149. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Motegi H, Kobayashi H, Terasaka S, Yamaguchi S, Ishi Y, Ito Y, Houkin K. Application of endoscopic ultrasonography to intraventricular lesions. Acta Neurochir (Wien). 2016;158:87-92. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Oesterling AE, Hansen BE. Severe Intraoperative Hemorrhage during Craniectomy in a Patient with Polyostotic Fibrous Dysplasia. Anesthesiology. 2020;133:1261-1262. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Tan LA, Lopes DK, Munoz LF, Shah Y, Bhabad S, Jhaveri M, Moftakhar R. Minimally invasive evacuation of intraventricular hemorrhage with the Apollo vibration/suction device. J Clin Neurosci. 2016;27:53-58. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Yamamoto T, Takeuchi K, Nagata Y, Mizuno A, Wakabayashi T. Novel Endoscopic Technique for Inserting a Sheath into a Slit Ventricle: The Water-Slide Technique. World Neurosurg. 2021;145:1-4. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Kuwabara M, Sadatomo T, Yuki K, Migita K, Imada Y, Shimizu K, Hara T, Oba H, Kurisu K. The Effect of Irrigation Solutions on Recurrence of Chronic Subdural Hematoma: A Consecutive Cohort Study of 234 Patients. Neurol Med Chir (Tokyo). 2017;57:210-216. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Guan F, Peng WC, Huang H, Ren ZY, Wang ZY, Fu JD, Li YB, Cui FQ, Dai B, Zhu GT, Xiao ZY, Mao BB, Hu ZQ. Application of neuroendoscopic surgical techniques in the assessment and treatment of cerebral ventricular infection. Neural Regen Res. 2019;14:2095-2103. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Demerdash A, Rocque BG, Johnston J, Rozzelle CJ, Yalcin B, Oskouian R, Delashaw J, Tubbs RS. Endoscopic third ventriculostomy: A historical review. Br J Neurosurg. 2017;31:28-32. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Li C, Zong X, Wang X, Gui S, Zhang Y. Intraoperative Hemorrhage in Ventriculoscopic Surgery: Experience of a Single Chinese Neurosurgery Center. World Neurosurg. 2016;88:548-551. [PubMed] [DOI] [Cited in This Article: ] |