Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3828
Peer-review started: July 17, 2021
First decision: December 9, 2021
Revised: December 18, 2021
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: April 26, 2022
Severe stenotic myocardial bridges (MBs) have been reported to lead to intracoronary ischaemia, but the physiological evaluation of MBs using intracoronary function evaluation indicators after intraoperative drug treatment has not been fully established.
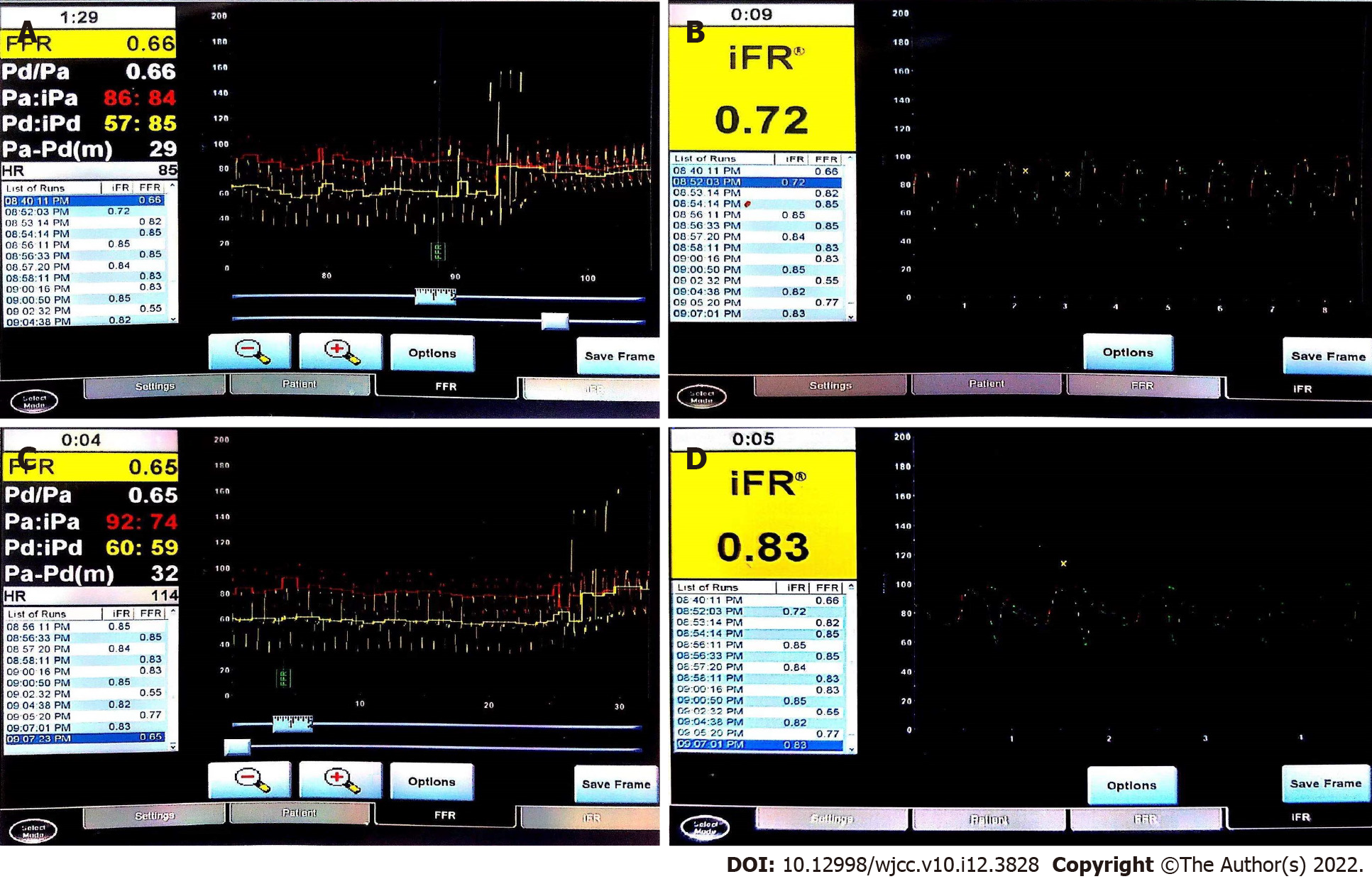
We performed through snuff fossa for coronary angiography in a patient with chest tightness after repeated exercise, and the results showed that the middle part of the anterior descending branch was a MB with 100% systolic compression. The intracoronary function evaluation (defined as the ratio of distal coronary pressure to aortic pressure with zero microcirculation resistance) was instantaneous wave-free ratio (IFR) without drug and fractional flow reserve (FFR) with adenosine. The IFR was 0.73, and the FFR was 0.66. Then esmolol 0.02 µg/kg/min was intravenously injected. The IFR and FFR were measured again when the heart rate dropped to 60 beats/min. The IFR was 0.83, and the FFR 0.65.
This case report is a case of isolated MB with severe stenosis. After intraoperative drug treatment decreased the ventricular rate, an increase in the coronary function evaluation index was immediately observed to confirm the effective improvement of coronary blood flow.
Core Tip: Myocardial bridge is one of the causes of myocardial ischaemia, and some studies have found that the degree of ischaemia is positively correlated with the degree of systolic compression. In this case of severe stenosis, after intraoperative drugs reduced the ventricular rate of the patient, the coronary ischaemia improved. This is a relatively novel change in coronary function that was determined by evaluation indices.
- Citation: Sun LJ, Yan DG, Huang SW. Evaluation of intracoronary function after reduction of ventricular rate by esmolol in severe stenotic myocardial bridge: A case report. World J Clin Cases 2022; 10(12): 3828-3833
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3828.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3828
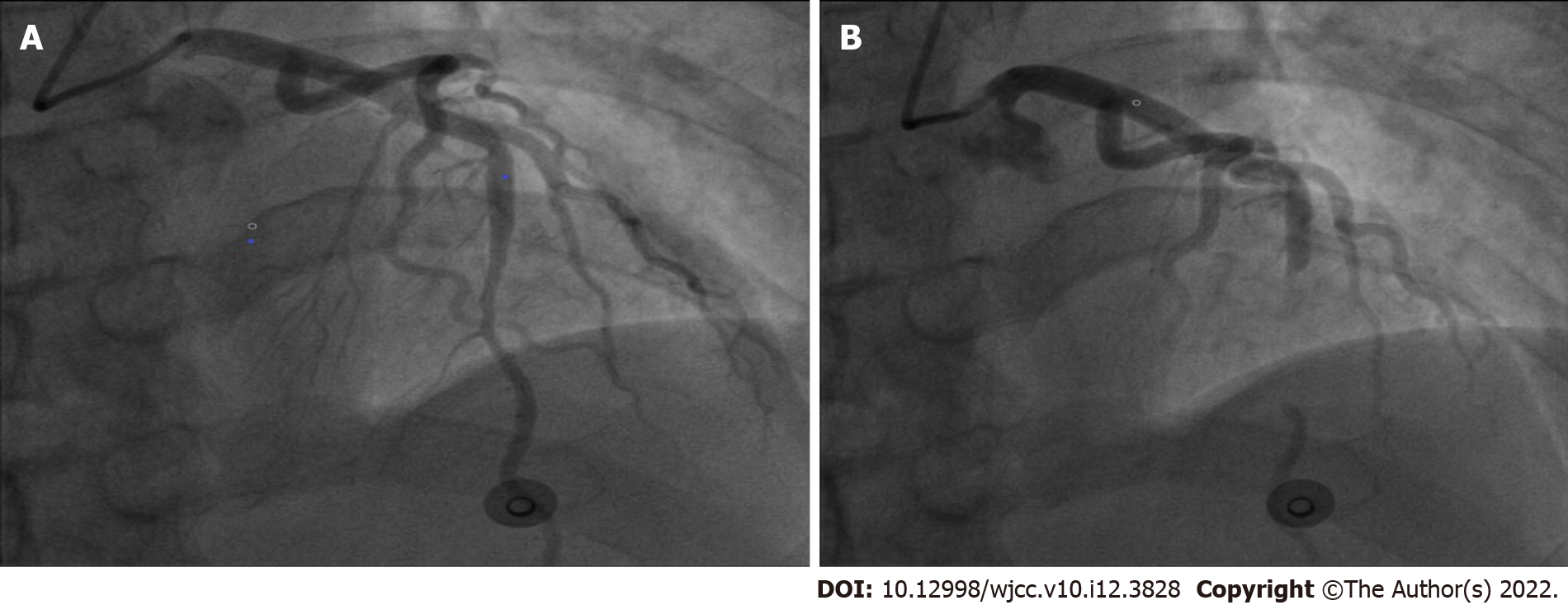
Coronary arteries are usually distributed on the surface of the epicardium, and occasionally segmental blood vessels run through the myocardium[1]. When this blood vessel is compressed by 70% in systole and 35% in late diastole, it is called a myocardial bridge[2]. Referring to relevant studies, Myocardial bridge (MB) can cause ischaemia in some patients, and the degree of systolic compression is inversely proportional to coronary flow reserve[3]. It has been proposed that drugs are the first choice for the treatment of MB. For isolated MB with severe stenosis, it is necessary to evaluate the state of coronary blood flow. The main evaluation methods are fractional flow reserve (FFR) and instantaneous wave-free ratio (IFR). FFR is defined as the ratio of distal coronary artery pressure to aortic pressure under the condition of maximal dilatation of small vessels and microvessels in the coronary artery supply area and no significant increase in central venous pressure under the action of adenosine[4]. IFR refers to the ratio of distal mean pressure to mean arterial pressure in diastolic nonwaveform interphase stenosis. This principle uses the blood pressure with the lowest diastolic coronary artery resistance to approximately replace coronary artery blood pressure under the action of adenosine[5,6]. In this case, we describe a case of coronary angiography via the distal radial artery pathway. The results showed that the anterior descending branch MB was associated with 100% systolic compression (Figure 1). After intraoperative drug control of the ventricular rate, the improvement of the coronary ischaemic state was confirmed by changes in the evaluation index of coronary artery function.
A 37-year-old Chinese male was admitted to the hospital with repeated chest tightness for two years.
After taking aspirin, tigrenol and atorvastatin calcium before the operation, the patient still showed chest tightness. Since the chest tightness was not alleviated, coronary angiography was performed.
The patient had a history of previous hypertension for 4 years, was not taking medications, denied a history of diabetes and other chronic illnesses, had no history of long-term smoking or hyperlipidaemia, and had no family history of heart disease or other related risk factors for coronary heart disease.
No family history of heart disease.
Physical examination revealed an auscultation heart rate of 74 beats/min and no pathological murmur was found in each valve auscultation area. There was no enlargement of the heart boundary of percussion and no tremor in palpation.
No obvious abnormality in laboratory examination.
Twenty-four hours before the operation, the electrocardiogram was normal, and echocardiography showed that the left ventricular systolic function was normal.
The results showed that the MB of the middle part of the left anterior descending branch was accompanied by 100% systolic compression, and the rest of the vessels did not have any other significant stenosis (Figure 2).
Considering that the symptoms of chest tightness and discomfort may be related to severe stenotic myocardial bridges, intracoronary function evaluation was performed. The pressure was adjusted to 1 when the pressure guide wire entered the root of the aorta. The pressure was measured after the guide wire passed through the diseased segment, and an IFR of 0.72 was measured. Using an adenosine intravenous pump, an FFR of 0.66 was measured after the patient's blood pressure dropped by 10% . The critical values of FFR and IFR were 0.80 and 0.89, respectively. A value less than the critical value indicates that a myocardial bridge caused significant haemodynamic changes. After myocardial bridge surgery, β-blockers were routinely used to reduce the heart rate of the patient. During the operation, we waited for the completion of the basic metabolism of adenosine and injected esmolol 0.02 µg/kg/min intravenously. After the heart rate dropped to 60 beats/min (basal heart rate 75 beats/min), changes in coronary blood flow could be observed. The results of the retest were FFR = 0.65 and IFR = 0.83 (Figure 3).
At the end of the operation, the puncture site was pressed with an elastic bandage to stop bleeding. Three hours later, there were no complications, such as blood oozing and haematoma. The patient was discharged 3 h after operation. After discharge, the patient was treated with metoprolol 47.5 mg qd for one month, and the symptoms of chest tightness were significantly relieved after follow-up.
The myocardial bridge is a segment of the coronary artery in the myocardium. Long-term studies have suggested that MB only blocks systolic coronary blood flow[7]. However, some studies have reported that MB is associated with stable angina pectoris, acute coronary syndrome and malignant arrhythmias that may lead to sudden death[8]. Therefore, a full understanding of the haemodynamic significance of MB during surgery is of great significance to guide treatment. There have been a large number of studies evaluating the intracoronary function of myocardial bridges. First, Teragawa et al[8] used FFR and IFR to confirm that myocardial bridges can cause coronary ischaemia and angina pectoris in patients. Second, Ryan and Escaned[9] measured the FFR of patients with myocardial bridges stimulated by baseline and dobutamine. This study ultimately found that the average FFR measurement increased artificially due to excessive systolic blood pressure, and diastolic FFR should be the first choice. Compared with adenosine, dobutamine seems to be more accurate in evaluating myocardial bridge FFR, highlighting the importance of muscle strength in the development of vascular compression. Third, Klues found that a myocardial bridge causes coronary haemodynamic abnormalities by combining intracoronary Doppler blood flow with pressure measurement. This is characterized by a continuous decrease in diastolic diameter, an increase in blood flow velocity and retrograde blood flow, and a decrease in blood flow reserve. However, there are few reports on the evaluation of the intracoronary function of myocardial bridges after intraoperative drug treatment. In this case, the MB was located near the middle part of the anterior descending branch. Here, the muscle bridge is longer, so the degree of systolic compression is more serious. Angiography also indicated that the muscle bridge had a systolic compression of 100%. To understand the blood flow changes of severely stenotic myocardial bridges, intraoperative coronary functional evaluation was used. The decrease in coronary flow reserve has a significant inhibitory effect on diastolic coronary blood flow. There are several possible mechanisms for this effect. One such mechanism is that the blood flow in the proximal end of the myocardial bridge with severe systolic compression can be stopped or even retrograde. This results in a partial decrease in the distal perfusion pressure of the bridging vessel and leads to ischaemia[9]. Vascular contraction and compression of the myocardial bridge segment causes turbulence and high shear stress, which leads to the disturbance of vascular endothelial function, an increase in the expression of vasoactive substances and morphological changes in endothelial cells and smooth muscle cells in this region. This leads to self-repair of the vascular endothelium, thickening of the vessel wall, stenosis of the lumen and a decrease in coronary blood flow reserve. The more serious the systolic vascular compression of the myocardial bridge is, the worse the diastolic diameter recovery, the higher the intracoronary filling pressure, and the lower the blood supply rate., All of these conditions seriously affect the main perfusion period of the coronary artery. Another mechanism by which the coronary flow reserve effects diastolic coronary blood flow occurs when the change in diastolic blood flow is more obvious. An obvious abnormality in flow velocity further leads to a decrease in coronary flow reserve. In this case, the coronary blood flow reserve decreased seriously in the severely narrow myocardial bridge, and the symptoms of myocardial ischaemia, such as chest tightness, became more obvious once the heart rate increased. In the face of isolated MB with such severe stenosis, in addition to percutaneous coronary intervention, coronary artery bypass grafting and surgical unroofing, the main treatment is still drugs. To understand the improvement of coronary artery ischaemia in patients with severe myocardial bridge stenosis, esmolol 0.02 µg/kg/min was injected intravenously during the operation. When the heart rate dropped to 60 beats/min, the FFR and IFR were measured again. FFR was 0.65 and IFR was 0.83. The IFR was significantly higher than it was before treatment, suggesting that the coronary flow reserve was better than before. One possible reason is that esmolol inhibits the automaticity of the sinoatrial node, prolongs atrioventricular conduction and reduces heart rate. Thus the diastolic period is prolonged, the time of myocardial bridge blood supply is prolonged, and the myocardial contractility and myocardial oxygen consumption are reduced. The average peak value, diastolic peak value and maximum instantaneous peak velocity in the myocardial bridge were significantly increased[10]. A second possible reason is that β-blockers can also reduce systemic and intramural pressure to reduce vascular compression in vitro, They can also reduce the indirect effect of sympathetic drive, further improve the state of coronary ischaemia, and relieve ischaemic symptoms, such as chest tightness and chest pain, in patients[11]. Other possible reasons could be a decrease in heart rate, decrease in peak blood flow in early diastole, prolongation of diastolic platform, disappearance of reverse blood flow, recovery of normal diastolic blood flow velocity, and relief of coronary flow reserve.
For isolated MB with severe stenosis, it is novel to observe the improvement of coronary blood flow after intraoperative drug therapy is added to reduce ventricular rate. At present, the main treatment is still drugs. However, the applicable types of evaluation methods and the effectiveness of long-term treatment need to be further evaluated by large-scale studies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dhali A, India; Tumminello G, Italy S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Tiryakioğlu M, Aliyu MN. Myocardial bridge. Folia Morphol (Warsz). 2020;79:411-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Hostiuc S, Negoi I, Rusu MC, Hostiuc M. Myocardial Bridging: A Meta-Analysis of Prevalence. J Forensic Sci. 2018;63:1176-1185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Teragawa H, Oshita C, Ueda T. The Myocardial Bridge: Potential Influences on the Coronary Artery Vasculature. Clin Med Insights Cardiol. 2019;13:1179546819846493. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, Bhindi R, Lehman SJ, Walters D, Sapontis J, Janssens L, Vrints CJ, Khashaba A, Laine M, Van Belle E, Krackhardt F, Bojara W, Going O, Härle T, Indolfi C, Niccoli G, Ribichini F, Tanaka N, Yokoi H, Takashima H, Kikuta Y, Erglis A, Vinhas H, Canas Silva P, Baptista SB, Alghamdi A, Hellig F, Koo BK, Nam CW, Shin ES, Doh JH, Brugaletta S, Alegria-Barrero E, Meuwissen M, Piek JJ, van Royen N, Sezer M, Di Mario C, Gerber RT, Malik IS, Sharp ASP, Talwar S, Tang K, Samady H, Altman J, Seto AH, Singh J, Jeremias A, Matsuo H, Kharbanda RK, Patel MR, Serruys P, Escaned J. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017;376:1824-1834. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 679] [Cited by in F6Publishing: 634] [Article Influence: 90.6] [Reference Citation Analysis (0)] |
| 5. | Teragawa H, Fujii Y, Oshita C, Y Uchimura, T Ueda. What factors contribute to chest symptoms during exercise in patients with vasospastic angina? 2017; 3: 1-7. [Cited in This Article: ] |
| 6. | Lee MS, Chen CH. Myocardial Bridging: An Up-to-Date Review. J Invasive Cardiol. 2015;27:521-528. [PubMed] [Cited in This Article: ] |
| 7. | Escaned J, Echavarría-Pinto M, Garcia-Garcia HM, van de Hoef TP, de Vries T, Kaul P, Raveendran G, Altman JD, Kurz HI, Brechtken J, Tulli M, Von Birgelen C, Schneider JE, Khashaba AA, Jeremias A, Baucum J, Moreno R, Meuwissen M, Mishkel G, van Geuns RJ, Levite H, Lopez-Palop R, Mayhew M, Serruys PW, Samady H, Piek JJ, Lerman A; ADVISE II Study Group. Prospective Assessment of the Diagnostic Accuracy of Instantaneous Wave-Free Ratio to Assess Coronary Stenosis Relevance: Results of ADVISE II International, Multicenter Study (ADenosine Vasodilator Independent Stenosis Evaluation II). JACC Cardiovasc Interv. 2015;8:824-833. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 153] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 8. | Teragawa H, Fujii Y, Ueda T, Murata D, Nomura S. Case of angina pectoris at rest and during effort due to coronary spasm and myocardial bridging. World J Cardiol. 2015;7:367-372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Ryan N, Escaned J. Myocardial bridge as a cause of persistent post percutaneous coronary intervention angina identified with exercise intracoronary physiology. Eur Heart J. 2017;38:1001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Tarantini G, Barioli A, Nai Fovino L, Fraccaro C, Masiero G, Iliceto S, Napodano M. Unmasking Myocardial Bridge-Related Ischemia by Intracoronary Functional Evaluation. Circ Cardiovasc Interv. 2018;11:e006247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Alegria JR, Herrmann J, Holmes DR Jr, Lerman A, Rihal CS. Myocardial bridging. Eur Heart J. 2005;26:1159-1168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 257] [Cited by in F6Publishing: 247] [Article Influence: 13.0] [Reference Citation Analysis (0)] |