Published online Aug 6, 2014. doi: 10.5527/wjn.v3.i3.118
Revised: April 28, 2014
Accepted: June 10, 2014
Published online: August 6, 2014
Little is written on the management of an innocuous-looking skin scab over an autogenous arteriovenous fistula (AVF) used for haemodialysis. The seriousness of the underlying pathology can be under-estimated, and this may lead to early loss of the AVF, and major-life-threatening haemorrhage. We describe the management of a 78-year-old patient presenting with an innocuous-looking scab over an AVF and review the pertinent literature on this subject.
Core tip: An innocuous looking scab may develop over an arteriovenous fistula after repeated punctures. There may be serious underlying damage to the arterialised vein. This case report emphasizes the importance of an early diagnostic colour Doppler examination in these circumstances and timely surgical intervention, to prevent potential life-threatening haemorrhage or other complications.
- Citation: Shrestha B, Boyes S, Brown P. Innocuous-looking skin scab over an arteriovenous fistula: Case report and literature review. World J Nephrol 2014; 3(3): 118-121
- URL: https://www.wjgnet.com/2220-6124/full/v3/i3/118.htm
- DOI: https://dx.doi.org/10.5527/wjn.v3.i3.118
An arteriovenous fistula (AVF) is a crucial life line for patients with end-stage renal failure, and its preservation is paramount. Complications related to AVF such as puncture haematoma, pseudoaneurysm formation, venous hypertension, arterial steal, high-output cardiac failure, and ischemic neuropathy, can not only lead to the early loss of an AVF but also can be life-threatening[1,2]. The prevalence of AVF compared to arteriovenous grafts, has risen steadily as a result of the National Kidney Foundation/Kidney Disease Outcome Quality Initiative (NKF/KDOQI) recommendations[3,4]. Little has been written on the pathological anatomy, natural history and management of visible scabs in the skin overlying AVF cannulation sites. We describe the management of a 78-year-old patient presenting with an innocuous-looking scab over the cannulation site of an AVF, emphasise the importance of early recognition and intervention, and review the pertinent literature related to the subject.
A 78-year-old male with renal failure secondary to obstructive uropathy had been on haemodialysis (HD) for two years using a brachiocephalic AVF. The AVF was cannulated using rope-ladder technique three times a week for 3 h in each session leading to excellent dialysis (pA: -71, pV: 73, blood flow: 360 mL/min, Kt/V: 1.4, pre-HD serum creatinine: 600 μmol/L and post-HD serum creatinine: 142 μmol/L). His haemoglobin was 12.2 gm/dL, white cell count of 7.5 × 106 / mL and C-reactive protein of 25 mg/L. His regular medication was erythropoietin, alphacalcidol and simvastatin.
The patient, who normally dialysed at a satellite unit, was referred to our tertiary referral teaching hospital because the dialysis staff were concerned about a visible black scab on the distal needling site which had developed over the previous 2 wk. There was no history of bleeding post-dialysis.
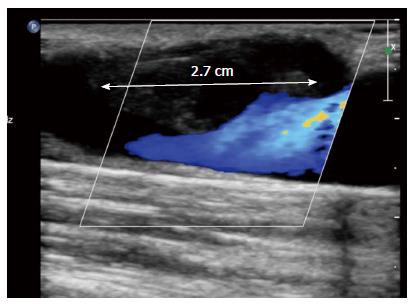
On examination, there was a 3 mm-sized black scab on the skin at the distal cannulation site without surrounding cellulitis or discharge (Figure 1). There was no clinical evidence of pseudo-aneurysm or subcutaneous haematoma. A palpable thrill and a low-pitched bruit were present along the course of the arterialised upper arm cephalic vein. The initial clinical impression was that the scab represented needle tract thrombus, which could be managed conservatively. However, based on previous experience of managing similar cases, a Doppler ultrasound scan was carried out. This showed a thrombus under the scab measuring 2.7 cm in length narrowing the vein significantly (Figure 2). It was suspected that although the size of the scab on the skin surface was about 3 mm in diameter, the defect in the cephalic vein wall could be more than 2 cm. A decision was made to explore the fistula and repair the defect.
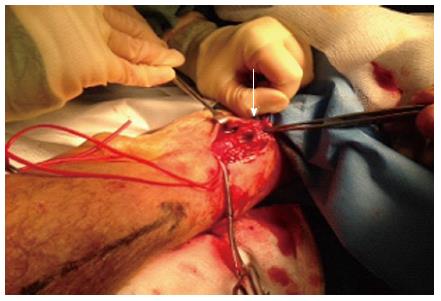
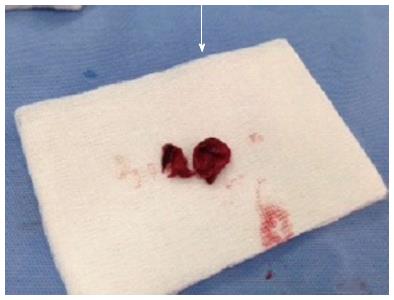
Under general anaesthesia, through an incision parallel to the AVF, the arterialised cephalic vein was skeletonised and controlled proximal and distal to the scab. The skin containing the scab was dissected off the vein, and this revealed dark thrombus bulging out through a 2.5 cm long defect on the anterior wall of the vein. The thrombus was causing partial narrowing of the vein (Figures 3 and 4). The thrombus was removed and the vein filled proximally and distally with heparinised saline. The edge of the defect on the vessel wall was debrided and closed using continuous 4/0 prolene suture. The thrombus was sent for culture and remained sterile after 48 h of incubation. The AV fistula was used for HD after 24 h.
Dialysis access procedures and access complications are the leading causes of morbidity among HD patients, often resulting in an increased number of hospitalizations and missed dialysis sessions. These complications, such as erosion, infection, thrombosis, and pseudoaneurysm formation, burden the health care system and disrupt patient care. As such, limiting these complications can significantly improve the quality of life of dialysis patients whilst decreasing health care costs[5,6]. The trauma of recurrent cannulation of a functioning AVF through the same site can lead to a tear of the wall of the vein. Simultaneous heparinisation during HD allows blood to flow out through the tear leading to the formation of a small pseudoaneurysm. Thrombus can form within the pseudoaneurysm in hypotensive and hypercoagulable states. The size of the pseudoaneurysm may be difficult to estimate on physical examination. The incidence of pseudoaneurysms complicating AVF ranges from 2% to 10%[7]. Generally, investigation of an innocuous-looking scab over an AVF is seldom initiated unless there is bleeding post-HD from the cannulation site, an obvious pseudoaneurysm, recirculation or venous hypertension[8].
Our case illustrates the fact that although the scab was only 3 mm in diameter with no evidence of surrounding inflammation, it was associated with a 2.5 cm long defect in the vein wall. The defect was filled with a thrombus which was also narrowing the lumen of the vein. The appearances were consistent with a thrombosed pseudoaneurysm.
Repeated needling of thrombus within a pseudoananeurysm may cause infective complications which may lead to bacteraemia and systemic sepsis. There is also a risk of necrosis of the overlying skin, ulceration and a life-threatening haemorrhage[9,10]. Dislodgement of the thrombus can lead to fatal pulmonary embolism. Recognition of the potential danger of small skin scabs was important in the timely investigation and intervention in our patient. Not only was the AVF salvaged, but the potential hazard of massive bleeding was prevented.
When assessing patients with skin scabs, a history of bleeding post-dialysis, adequacy of dialysis and systemic sepsis should be obtained. Physical examination should include the inspection of skin overlying the AVF for the extent of skin necrosis, cellulitis, pulsatility and haematoma, as well as assessment of the nature of the bruit along the length of the AVF. Duplex ultrasound is the primary diagnostic modality, with a sensitivity of 94% in the assessment of the size of the defect, and complications such as the presence of thrombus, reduced blood flow, stenoses and pseudo-aneurysms[11]. Ultrasound-guided compression of pseudoaneurysms can be curative[12]. If a defect is detected in the wall of the AVF, the patient should be prepared for exploration of the AVF under brachial block or general anaesthesia. Broad-spectrum antibiotic cover should be provided at the time of surgery. Surgical repair of the defect can be done by direct suture, patch angioplasty using saphenous vein or a Dacron patch, excision followed by end-to-end anastomosis, excision and interposition of a Polytetrafluroethylene graft or insertion of a bypass graft[13]. A large skin defect due to necrosis may require a locally rotated full-thickness Limberg skin flap[14]. Any thrombus extracted from the AVF should be sent for microbiological assessment. In majority of the patients, the AVF can be salvaged and used for HD within 24 h. If a bypass graft is inserted, the reported primary-assisted patency at 12 mo is 50%[15].
Every effort should be made to prevent the development of pseudoaneurysms, venous stenoses, skin erosions, haemorrhage and reduced access patency. The cannulation technique of an AVF has been a subject of debate. The rope-ladder (RL) technique is the most common technique, although button-hole cannulation (BHC) or constant-site technique is recommended by the NKF/KDOQI vascular access guidelines. Previous studies have shown less haematoma formation and less intervention in BHC group compared to the RL group[16-19]. However, a recent study comparing access patency, intervention rate, bacteraemia and mean scores from kidney disease-specific health-related quality of life (KD HRQOL-36) survey between RL and BHC groups failed to show a significant difference in outcome between the two groups[20].
In conclusion, awareness of the possibility of a large defect in the vein wall under an innocuous-looking scab, with the potential for life-threatening haemorrhage and access failure, should be raised among patients and health care workers[21]. If there is clinical concern an urgent Doppler ultrasound should be arranged, with urgent surgical intervention if indicated. It is also essential that trained staff follow established cannulation techniques to reduce the risk of puncture site complications.
A 78-year-old male, who was on haemodialysis using a brachiocephalic arteriovenous fistula (AVF), was referred by the dialysis staff raising concern for a scab over the cannulation site.
On examination, there was a 3 mm-sized black scab on the skin on the distal cannulation site without surrounding cellulitis or discharge.
A pseudoaneurysm and a haematoma underlying the scab were entertained in the differential diagnosis.
The white cell count and C-reactive protein were within normal limits.
The Duplex ultrasound scan showed a 2.7 cm large thrombus and a 2 cm defect in the vessel wall.
A 2.5 cm defect in the wall of the cephalic vein was occupied by a thrombus.
The vessel was explored and the defect was closed with 4/0 prolene suture.
The size of the visible scab over an autogenous AVF is misleading as in our case where there was a 2.5 cm defect in the vessel wall filled with a thrombus although the size of the scab was of 3 mm diameter. A Duplex san should be performed early to assess the AVF for prevention of bleeding.
The authors described the management of a 78-year-old patient who presented with an innocuous-looking scab over the cannulation site of an AVF which turned out to be a thrombus on the outer wall of the vein. This a good case report.
P- Reviewer: Teo TKB, Olowu WA S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | Ellingson KD, Palekar RS, Lucero CA, Kurkjian KM, Chai SJ, Schlossberg DS, Vincenti DM, Fink JC, Davies-Cole JO, Magri JM. Vascular access hemorrhages contribute to deaths among hemodialysis patients. Kidney Int. 2012;82:686-692. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Padberg FT, Calligaro KD, Sidawy AN. Complications of arteriovenous hemodialysis access: recognition and management. J Vasc Surg. 2008;48:55S-80S. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Pisoni RL, Young EW, Dykstra DM, Greenwood RN, Hecking E, Gillespie B, Wolfe RA, Goodkin DA, Held PJ. Vascular access use in Europe and the United States: results from the DOPPS. Kidney Int. 2002;61:305-316. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | NKF KDOQI Guidelines. Clinical practice guidelines and clinical practice recommendations 2006 Updates. Available from: http://www.kidney.org/professionals/kdoqi/guidelines_updates/doqi_uptoc.html#va. [Cited in This Article: ] |
| 5. | Biuckians A, Scott EC, Meier GH, Panneton JM, Glickman MH. The natural history of autologous fistulas as first-time dialysis access in the KDOQI era. J Vasc Surg. 2008;47:415-421; discussion 420-421. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Vascular Access Work Group. Clinical practice guidelines for vascular access. Am J Kidney Dis. 2006;48 Suppl 1:S248-S273. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Chen CY, Teoh MK. Graft rescue for haemodialysis arterio-venous grafts: is it worth doing and which factors predict a good outcome? J R Coll Surg Edinb. 1998;43:248-250. [PubMed] [Cited in This Article: ] |
| 8. | Lee T, Roy-Chaudhury P. Advances and new frontiers in the pathophysiology of venous neointimal hyperplasia and dialysis access stenosis. Adv Chronic Kidney Dis. 2009;16:329-338. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Mazzoleni L, Jadoul M, Labriola L. Arteriovenous fistula infection as a cause of vascular access hemorrhage. Kidney Int. 2013;83:969-970. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Jaffers GJ, Fasola CG. Experience with ulcerated, bleeding autologous dialysis fistulas. J Vasc Access. 2012;13:55-60. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Coughlin BF, Paushter DM. Peripheral pseudoaneurysms: evaluation with duplex US. Radiology. 1988;168:339-342. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Saad NE, Saad WE, Davies MG, Waldman DL, Fultz PJ, Rubens DJ. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25 Suppl 1:S173-S189. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Galbusera M, Remuzzi G, Boccardo P. Treatment of bleeding in dialysis patients. Semin Dial. 2009;22:279-286. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Pirozzi N, Pettorini L, Scrivano J, Menè P, Karam L, Bourquelot P. Limberg skin flap for treatment of necrosis and bleeding at haemodialysis arteriovenous angioaccess puncture sites. Eur J Vasc Endovasc Surg. 2013;46:383-387. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Kinning AJ, Becker RW, Fortin GJ, Molnar RG, Dall’Olmo CA. Endograft salvage of hemodialysis accesses threatened by pseudoaneurysms. J Vasc Surg. 2013;57:137-143. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | MacRae JM, Ahmed SB, Atkar R, Hemmelgarn BR. A randomized trial comparing buttonhole with rope ladder needling in conventional hemodialysis patients. Clin J Am Soc Nephrol. 2012;7:1632-1638. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Hashmi A, Cheema MQ, Moss AH. Hemodialysis patients’ experience with and attitudes toward the buttonhole technique for arteriovenous fistula cannulation. Clin Nephrol. 2010;74:346-350. [PubMed] [Cited in This Article: ] |
| 19. | van Loon MM, Goovaerts T, Kessels AG, van der Sande FM, Tordoir JH. Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant. 2010;25:225-230. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Chan MR, Shobande O, Vats H, Wakeen M, Meyer X, Bellingham J, Astor BC, Yevzlin AS. The effect of buttonhole cannulation vs. rope-ladder technique on hemodialysis access patency. Semin Dial. 2014;27:210-216. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Winsett OE, Wolma FJ. Complications of vascular access for hemodialysis. South Med J. 1985;78:513-517. [PubMed] [Cited in This Article: ] |