Published online May 29, 2020. doi: 10.5500/wjt.v10.i5.129
Peer-review started: January 5, 2020
First decision: February 20, 2020
Revised: March 18, 2020
Accepted: May 12, 2020
Article in press: May 12, 2020
Published online: May 29, 2020
In context of suboptimal liver utilisation, grafts with various risk factors are under consideration today. For example, impaired vascularity with severe arterial calcifications and modified liver shapes are no longer contraindications and their use depends on the centre policy and experience of the surgical team. Riedel liver lobes represent a tongue-like liver shape with inferior projection in the right liver lobe. Such development modifications were initially described when patients developed a lesion and subsequently presented with symptoms. We here present the first case report in the literature, where such livers with anatomical variations were used for transplantation.
We describe here two cases of adult human liver transplantation, where we have accepted two donor livers with modified shape. The technical considerations for transplantation of such livers, found with enlarged right lobes, or Riedel shape, and hypo-trophic left lateral segment are highlighted. Both recipients experienced immediate liver function and overall good outcomes with a minimum follow up of 1 year. We also provide detailed pictures and outcome analysis in combination with a literature review.
The utilisation of donor livers with modified shape, such as Riedel’s Lobe appears safe and will increase the donor pool.
Core tip: To the best of our knowledge, this will be the first report on utilisation of large right Riedel’s liver lobes with further anatomical modifications for liver transplantation. We highlight donor and recipient risk factors and focus parameters with impact on recipient selection and on technical aspects for implantation. Additionally, we combine our case series with current available literature in this field.
- Citation: Sakuraoka Y, Seth R, Boteon AP, Perrin M, Isaac J, Subash G, Muiesan P, Schlegel A. Large Riedel’s lobe and atrophic left liver in a donor - Accept for transplant or call off? World J Transplant 2020; 10(5): 129-137
- URL: https://www.wjgnet.com/2220-3230/full/v10/i5/129.htm
- DOI: https://dx.doi.org/10.5500/wjt.v10.i5.129
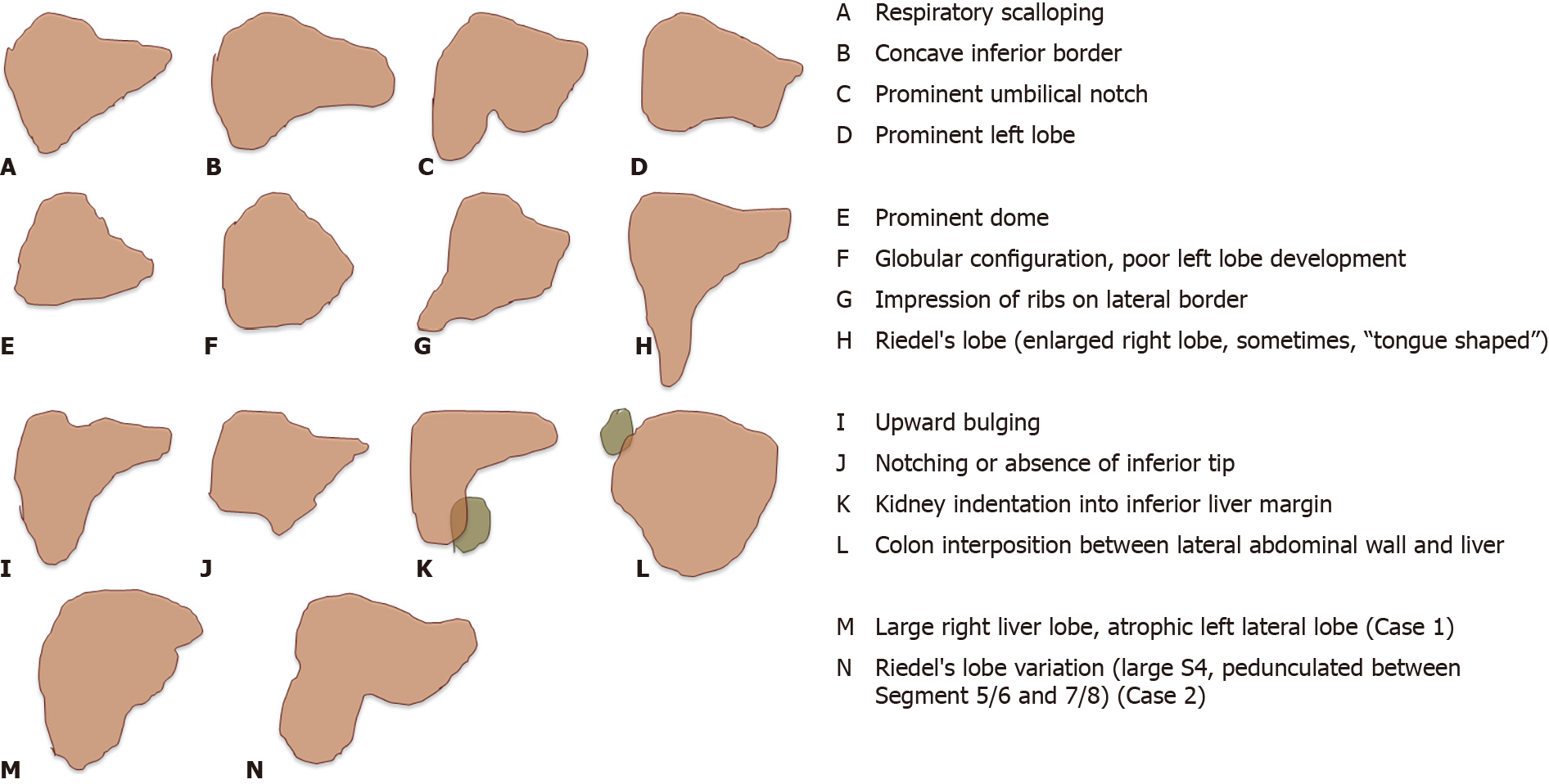
In context of the increasing organ demand, transplant surgeons are forced to push the boundaries and to accept not only marginal livers, but also grafts with calcified hepatic arteries or other anomalies to improve donor liver utilization[1]. Livers donated after traumatic injury are increasingly utilised for transplantation depending on the grade of hepatic damage and the structures involved. The policy of a transplant centre, the individual surgeons experience and the general availability of donor livers with subsequent recipient waiting time impact on such decisions whether to accept livers with specific anatomical features or not. We present here two cases, where donor livers with anatomical variations were utilised for transplantation at our centre. Several modified liver shapes were described initially by hepatobiliary surgeons and enlarged right lobes with a tongue-like shape were defined as one example, summarised as “Riedel’s lobe” (Figure 1)[2-5]. We demonstrate here the safe use of such grafts for transplantation and show recipient outcomes in combination with a literature review.
Chief complaints: The recipient presented with an advanced liver cirrhosis and suffered from the typical symptoms, including ascites, renal impairment and feeling chronically tired and cold.
History of present illness: The donor liver was offered from a 71-year-old male donor with brain death due to intracranial haemorrhage. The candidates underlying liver disease presented with the typical features of a slowly progressive liver disease over many years, despite alcohol abstinence.
History of past illness: The past medical history of the donor included arterial hypertension and cholecystectomy due to cholecystitis with peritonitis more than 20 year prior to donation. The recipient’s history other than the liver disease was uneventful.
Personal and family history: The recipient’s history was uneventful.
Physical examination upon admission: The recipient presented with the typical symptoms of advances liver cirrhosis with several litres of ascites, requiring regular paracentesis, sarcopenia and encephalopathy.
Laboratory examinations: The donor liver parameters were entirely normal. The recipient presented with a lab end stage liver disease (MELD) score of 22 points and the sodium was in the low normal range.
Physical examination upon admission: According to the national allocation system, our team was allowed to choose the recipient from the waiting list. We selected a 62-year-old patient with alcoholic liver cirrhosis and large amount of ascites, regular paracentesis and previous spontaneous bacterial peritonitis. Recipient selection (large volume ascites) was based on the expected large right lobe of 2.2 kg.
Laboratory examinations: Despite such advanced liver disease, the candidate achieved only limited number of 22 and 54 points for the model of MELD and United Kingdom model for end stage liver disease score with, respectively (Table 1). The standard recipients imaging, performed during transplant assessment revealed patent vessels and a replaced right hepatic artery (HA) from the supra-mesenteric artery.
| Parameter | Case 1 | Case 2 |
| Donor and graft Parameter-type, COD | DBD, ICH | DBD, ICH |
| Age (yr) | 71 | 73 |
| BMI (kg/m2) | 23 | 25 |
| Past medical history | Hypertension, Previous cholecystectomy for cholecystitis and peritonitis | Hypertension |
| Liver weight (kg) | 2.2 | 1.8 |
| Recipient parameter | ||
| Age (yr) | 62 | 63 |
| Underlying disease | Alcoholic cirrhosis, ascites, SBP, regular paracentesis | Alcoholic cirrhosis |
| Lab MELD | 22 points | 17 points |
| Transplantation surgery | 7L Ascites, thrombectomy for portal vein thrombosis Grade 2 | Minimal ascites |
| Modified Piggy back, side-to-side | Modified Piggy back, side-to-side | |
| Donor CHA-GDA patch to Recipient RHA from SMA (GDA patch) | Donor CHA-GDA patch to Recipient CHA-GDA patch | |
| Duct – to – Duct over plastie | Duct – to – Duct | |
| 5 RBC, 8 FFP, no platelets or cryo | 2 RBC, no FFP, no platelets or cryo | |
| Outcome | Immediate liver function and extubation | Immediate liver function and extubation |
| Acute kidney injury without renal replacement therapy | One episode of acute cellular rejection | |
| Hospital stay: 12 d | Hospital stay: 26 d | |
| One local readmission for diarrhea within first 3 mo | Biliary reconstruction for Anastomotic stricture after 14 mo | |
| One episode of acute cellular rejection after 19 mo | ||
| Follow up | 12 mo, alive, normal liver function | 22 mo, alive, normal liver function |
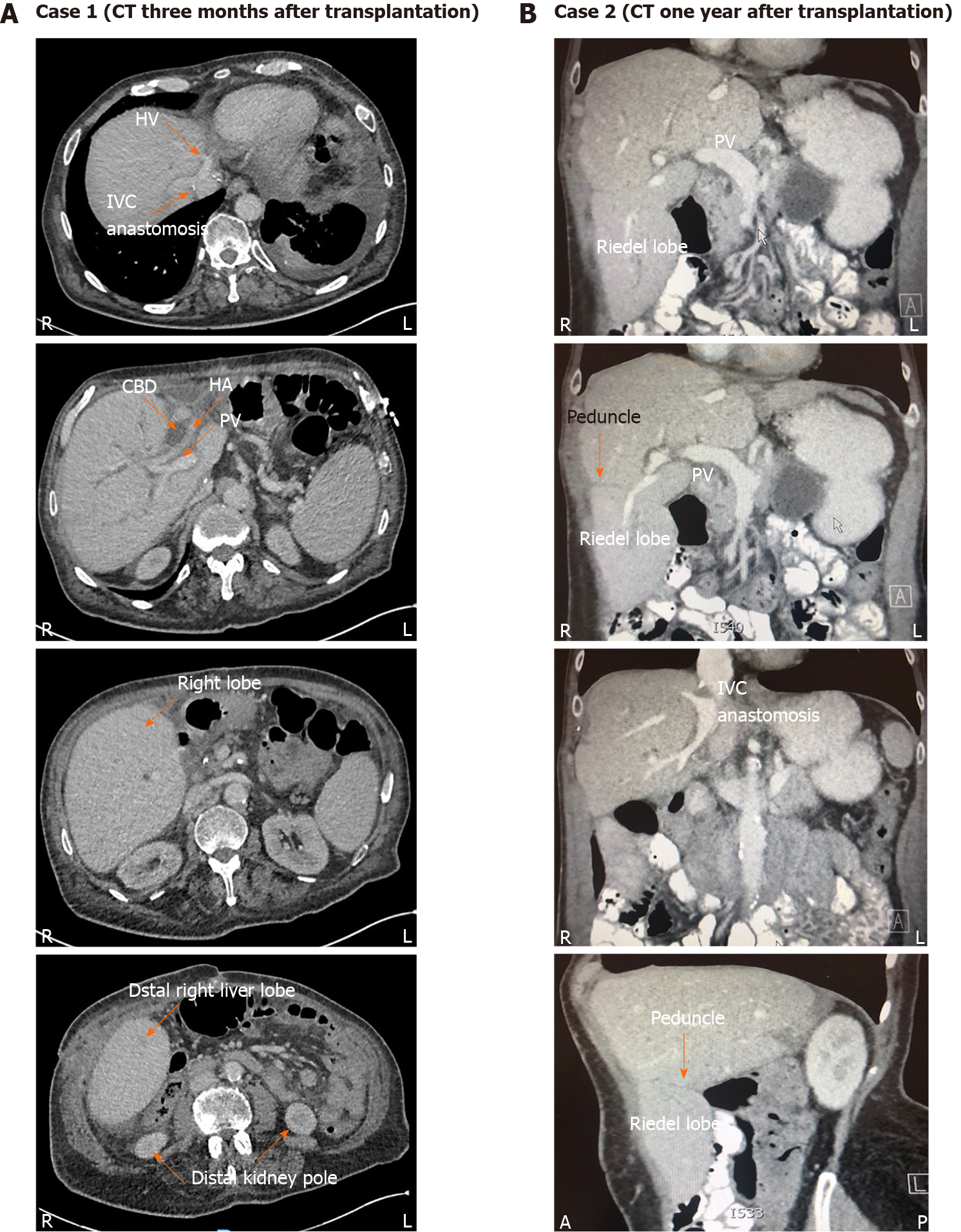
Imaging examinations: Due to an aspiration pneumonia, a computer tomography (CT) of the donor’s chest was done and the upper abdomen was captured, where a very small left lateral liver segment with possible biliary dilatation was identified. The recipient’s ultrasound scan, done as per routine prior to admission on the waiting list showed ascites and the expected cirrhotic and shrunken liver with patent vessels. Interestingly, the intraoperatively identified portal vein thrombosis was not seen on the abdominal CT scan.
Final diagnosis: The donor liver with anatomical variation was accepted for liver transplantation for a recipient with advanced alcohol related liver disease within the fast track liver offering system.
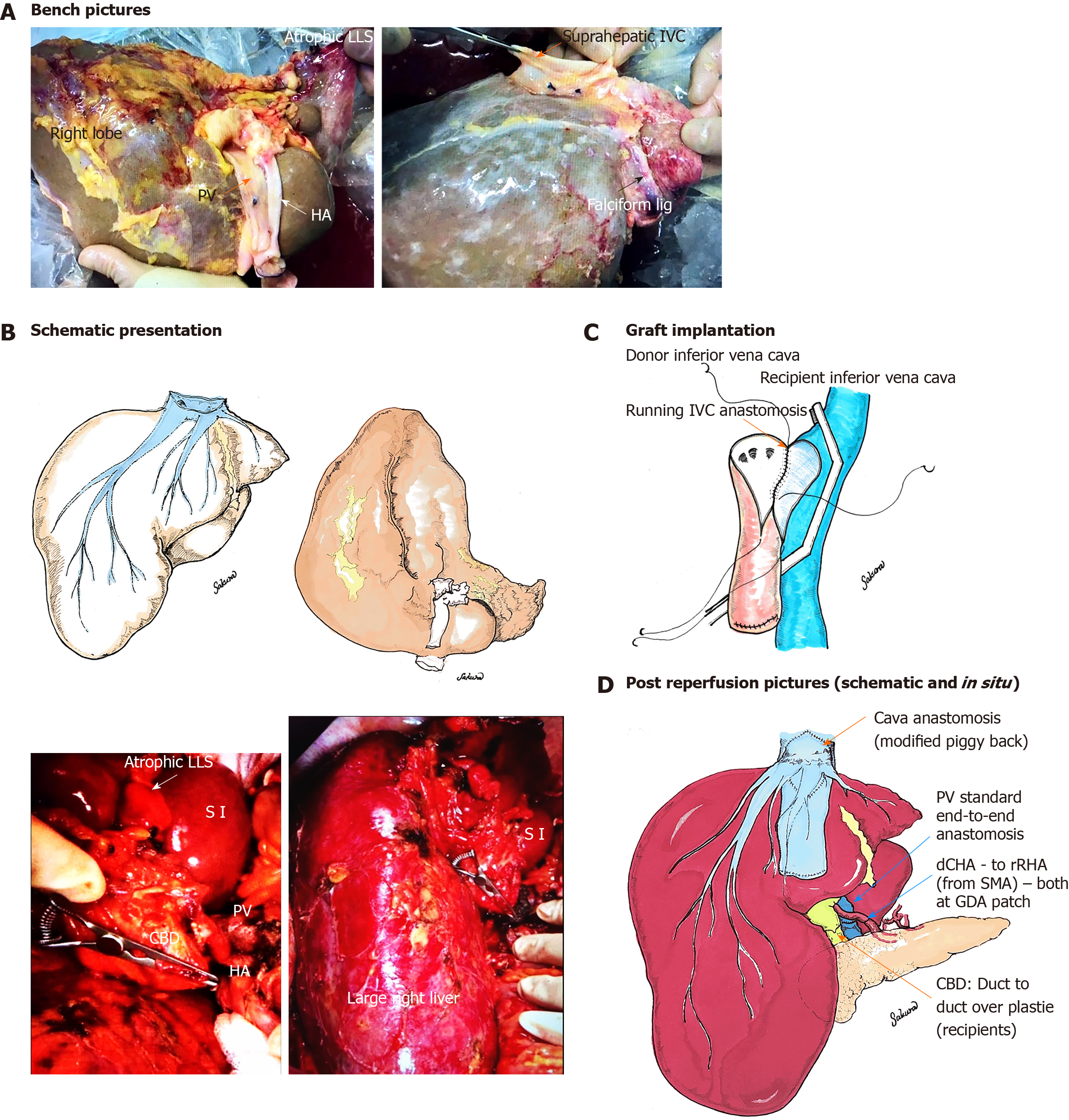
Treatment: Based on the long waiting time in blood group 0, we have decided to go ahead with the donation procedure and assess the donor and the liver. The procurement was done by a team from an experienced centre in the United Kingdom. A large right liver lobe (Riedel’s lobe) combined with an atrophic left lateral segment was identified. Only minimal liver tissue was evident on the left side of the falciform ligament (Figure 2). The weight of this graft was 2.2 kg, with mild steatosis and normal vascular anatomy. Some adhesions from the previous cholecystectomy were found, however no other lesions or findings were evident. Importantly, the anatomical development was normal for all vascular and biliary structures on both liver sides with a however small left hepatic vein corresponding to the atrophic left lateral segment (LLS). This graft was declined by all other centres and became fast tracked.
During transplantation surgery, 7 L of ascites were evacuated, severe portal hypertension, and advanced SBP were found. Additionally, a grade 2 portal vein thrombosis (PVT), requiring thrombectomy was identified. Due to the graft-recipient size relation with the thick right Riedel lobe and dominant right and middle hepatic vein, the decision was made to implant the graft with a modified piggyback technique, in contrast to the standard classic piggy-back technique (graft cava–to recipient orifice of left and middle hepatic vein), which is routinely performed in half of whole grafts at our centre (Figure 2C-2D). To achieve optimal draining of the compact right liver lobe through the dominant right hepatic vein, a large teardrop shape incision was performed at both, donor and recipient vena cava. The satinksy clamp was rotated slightly to the right side of the recipient towards the graft. The recipient hepatic veins were not included in the anastomoses, due to their fragile texture. The portal vein anastomosis was done in a standard fashion (end-to-end) and the recipients replaced right HA demonstrated a good calibre and strong pulse, enabling us to use this vessel for the reconstruction with the common donor HA at the gastro-duodenal artery patch (Figure 2).
Outcome and follow-up: The reperfusion was uneventful, no reclamping was required and immediate graft function was evident through bile flow, decreasing lactate and minimal inotrope support at the end of surgery. The reconstruction of the common bile duct (CBD) was done over a recipient duct plastie, based on the size discrepancy with a large donor CBD. Vessel patency was confirmed through intraoperative ultrasound. The liver demonstrated good function and the recipient was extubated within the first day after transplantation with an overall short intensive care stay of 2 d. Acute kidney injury occurred without requirement of hemofiltration. The recipient was discharged within 12 d and required one short, local readmission for diarrhoea (Table 1). Further follow up was uneventful with an asymptomatic patient more than 12 mo after liver transplantation.
Chief complaints: The second liver was offered through the national allocation system and primarily accepted for a 63-year-old lady with alcoholic liver cirrhosis and limited ascites.
History of present illness: The selected candidate had an alcohol induced liver cirrhosis since many years.
History of past illness: Donor and recipient had no further relevant illnesses in the past.
Physical examination upon admission: On admission the typical features of liver cirrhosis were present in the recipient, including ascites, sarcopenia and dominant venous collaterals.
Laboratory examinations: Expectedly the transplant candidate presented with impaired liver function tests and a laboratory MELD and United Kingdom model for end stage liver disease score of 17 and 59 points, respectively.
Imaging examinations: The previously performed abdominal ultrasound revealed a shrunken liver with features of cirrhosis, abdominal ascites and patent liver vessels.
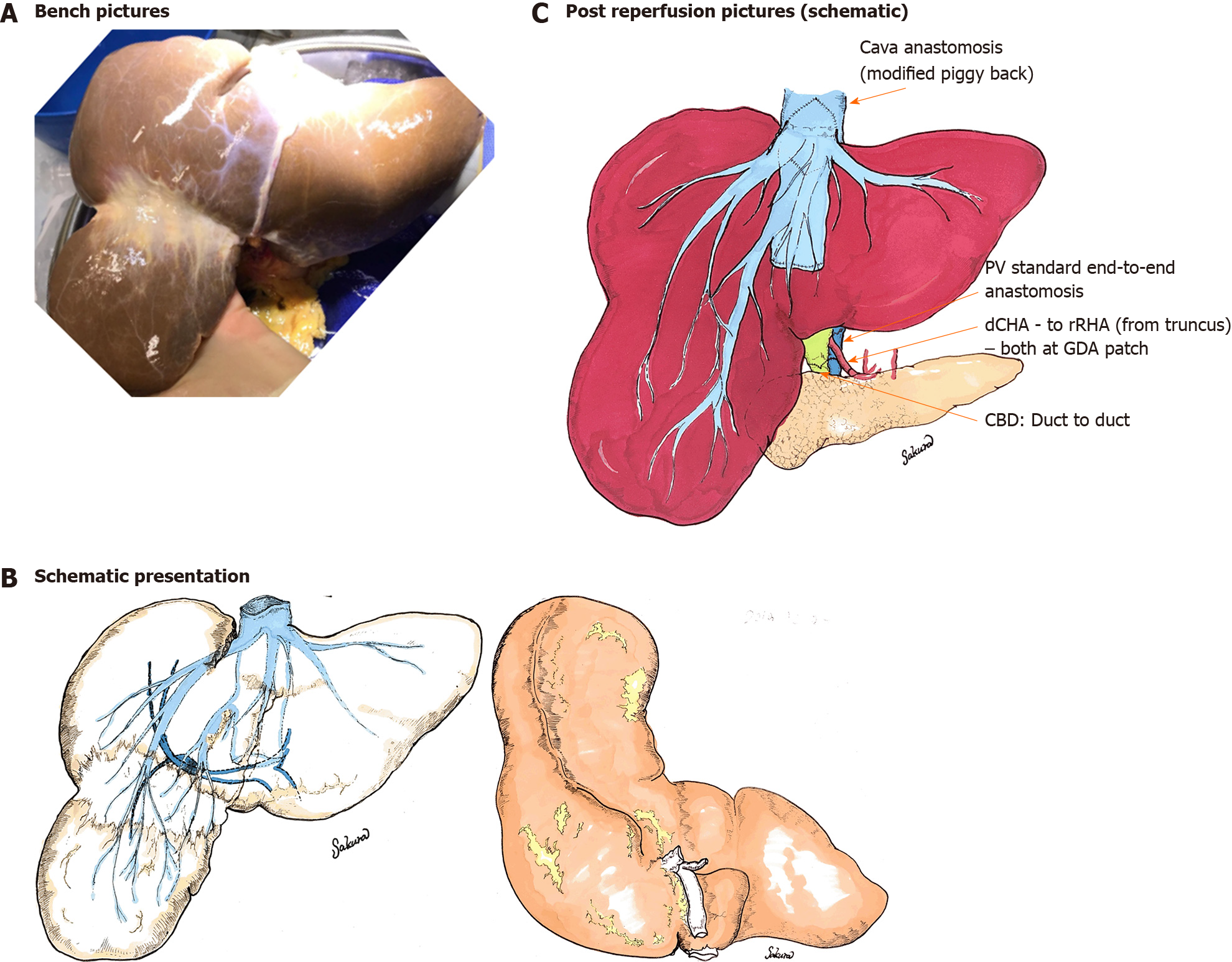
Final diagnosis: The donor liver was 73-year-old and found with a large right Riedel’s lobe, with normal sized left lobe (Figure 3), regularly utilized for liver transplantation for the recipient with alcoholic liver cirrhosis, who was listed within the national offering system.
Treatment: There was no relevant steatosis and no retrieval injuries with normal vascular anatomy. Following an overall cold ischemia time (CIT) of 9 h 36 min the liver was implanted using a modified (side-to-side) piggyback technique. The recipient’s vessel anatomy was normal and standard end-to-end donor - recipient portal vein anastomosis was performed with subsequent arterial reconstruction at both common HA–gastro-duodenal artery patch.
Outcome and follow-up: Day one ultrasound confirmed patent vascularity and the patient were discharged to the normal ward within 3 d. However, moderate acute cellular rejection (ACR) occurred and required steroid treatment with a prolonged hospital stay of 26 d. During further follow-up a late anastomotic stricture was identified and conservative treatment failed with subsequent requirement of a biliary reconstruction, performed 14 mo after liver transplantation. This event was followed by a second episode of ACR, three months later, where the patient recovered with normal liver function tests almost 2 years after transplantation (Table 1). Both donor livers were normally perfused with no areas of hypoperfusion during follow up with ultrasound and CT (Figure 4).
The analysis and report of the cases was approved by the local ethic committee (CARMS-15376).
To the best of our knowledge this is the first report, where donor livers with modified shape, including Riedel’s lobe were safely utilised for liver transplantation. Anatomical liver variations were first described by hepatobiliary surgeons, initially identified through explorative laparotomies, indicated when the large lobe was palpable through the abdominal wall, imitating a large liver lesion[4,6]. The features of the Riedel’s lobe were described first by Corbin in 1830, while Riedel defined this enlarged right liver in 1888 as a “round shaped tumour found on the right distal side of the liver“, which extends beyond the gallbladder[7]. Riedel’s lobes are more common in females and some described the shape as a “tongue“[7]. The overall liver size depends on age, body size, gender and body shape[8]. The ethiology was discussed by many as either congential, being a result of an anomaly of the hepatic bud during development, or acquired, secondary to changes in hepatic morphology in context of skeletal anomalies, including kyphoscoliosis with a wide thorax[2,3]. Further potential causes were described as chronic traction due to adhesions through appendicitis or gallstone disease with subsequent cholecystitis and peritonitis[3]. Such features were found in the first donor, reported here. The development of the liver vessels and biliary tree appeared normal and all structures were evident even on the atrophic left side. In context of acute on chronic cholecystitis with peritonitis the LLS atrophied throughout years with a compensatory increase of the right liver to a Riedel’s lobe shape. The reperfusion of the LLS appeared normal at implantation. Meticulous assessment of potential risk factors in the donors past medical history is of importance to avoid an underlying disease of the biliary tree. In the United Kingdom, the donor past medical history is very thoroughly examined by specialist nurses of organ donation. Donor families, general practitioner and specialists involved are routinely contacted to obtain further details prior to organ donation[1].
Ideally, selection of either larger recipients or the presence of ascites is suggested to achieve enough space for the graft and avoid congestion of the large Riedel’s lobe. Potential candidates with progredient ascites and repeat paracentesis have a prolonged window of fairly stable liver function with low MELD scores, despite very advanced intraabdominal disease with portal hypertension, cocoon-like peritoneum due to repeat peritonitis, which may appear relatively silent. Additionally, such candidates are at higher risk to develop sudden portal vein thrombosis, as seen in our case. Based on this we have selected our recipient here for the first case presented.
In order to achieve an optimal outflow of the dominant right and middle hepatic vein either cava replacement or modified piggyback implantation technique could be used, similarly to right lobe split grafts. In the second case, segment 5/6 were pedunculated from segment 7/8 on a however wide bridging area with low risk of torsion. Similar considerations in terms of space are suggested, though the right lover lobe was not comparably thick as in case 1, which lead to a more standardised side to side piggyback implantation technique with more simple longitudinal incision of donor and recipient cava.
This case report has several limitations. First the retrospective design and selective presentation of two cases, while there is an expected much higher number of Riedel lobe graft implantations, potentially done at our centre where simply the imaging material was not properly collected in earlier days. Such Although variations in liver shape, including Riedel lobes have been seen by many experienced transplant and hepatobiliary surgeons who either removed tumour lesions from such tongue-like liver lobes or used the liver for transplantation, this is the first case report identified to the best of our knowledge. To increase the donor pool further we would therefore suggest to use liver grafts with specific anatomical variations for implantation given there is no other contraindication to accept the graft.
In conclusion, modifications of the donor liver shape should not preclude utilization, particularly in experienced centres, where different implantation techniques, including several piggyback variations, are available and routinely adapted to the clinical and anatomical situation of graft and recipient.
Modifications of the donor liver shape should not preclude utilization, particularly in experienced centres, where different implantation techniques, including several piggyback variations, are available and routinely adapted to the clinical and anatomical situation of graft and recipient.
We would like to express our great appreciation to the donors and their families and the specialist nurses of organ donation involved in our two transplant cases. We also thank the donor procurement teams, our theatre team and colleagues from Anaesthesia, intensive care unit and hepatology for their support and daily care of our patients.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Europen Society of Organ Transplantation; International Liver Transplant Society.
Specialty type: Transplantation
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Abdelaziz O, Akbulut S, Chedid M, Cimen SG, Mrzljak A S-Editor: Ma YJ L-Editor: A E-Editor: Li X
| 1. | Marcon F, Schlegel A, Bartlett DC, Kalisvaart M, Bishop D, Mergental H, Roberts KJ, Mirza DF, Isaac J, Muiesan P, Perera MT. Utilization of Declined Liver Grafts Yields Comparable Transplant Outcomes and Previous Decline Should Not Be a Deterrent to Graft Use. Transplantation. 2018;102:e211-e218. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Champetier J, Yver R, Létoublon C, Vigneau B. A general review of anomalies of hepatic morphology and their clinical implications. Anat Clin. 1985;7:285-299. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 44] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Glenisson M, Salloum C, Lim C, Lacaze L, Malek A, Enriquez A, Compagnon P, Laurent A, Azoulay D. Accessory liver lobes: anatomical description and clinical implications. J Visc Surg. 2014;151:451-455. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Wolf DC, Walker HK, Hall WD, Hurst JW. Evaluation of the Size, Shape, and Consistency of the Liver. In: Kenneth Walker H, Dallas Hall D, Willis Hurst J, Editors. Clinical Methods: The History, Physical, and Laboratory ExaminationsEdition, 3rd. Welsh: Butterworths, 1990: Chapter 94. [PubMed] [Cited in This Article: ] |
| 5. | Akbulut S, Cakabay B, Sevinc MM, Basak F. Gastric outlet obstruction caused by Riedel's lobe of the liver: a diagnostic and therapeutic challenge for surgeons. Hepatogastroenterology. 2011;58:589-592. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Sabih Z, Durr-e-Sabih, Khan SM. Normal shapes of liver: analysis of normal nuclear scans in Multan. J Pak Med Assoc. 1986;36:33-36. [PubMed] [Cited in This Article: ] |
| 7. | Elfeshawy MS. Bilobed spleen, transposition of the inferior vena cava and Riedel lobe: an extremely rare imaging finding in the same case. BJR Case Rep. 2019;5:20180091. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Gillard JH, Patel MC, Abrahams PH, Dixon AK. Riedel's lobe of the liver: fact or fiction? Clin Anat. 1998;11:47-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |