Published online Mar 19, 2024. doi: 10.5498/wjp.v14.i3.388
Peer-review started: December 12, 2023
First decision: January 2, 2024
Revised: January 12, 2023
Accepted: February 27, 2024
Article in press: February 27, 2024
Published online: March 19, 2024
Major depressive disorder is a common mental illness among adolescents and is the largest disease burden in this age group. Most adolescent patients with depression have suicidal ideation (SI); however, few studies have focused on the factors related to SI, and effective predictive models are lacking.
To construct a risk prediction model for SI in adolescent depression and provide a reference assessment tool for prevention.
The data of 150 adolescent patients with depression at the First People's Hospital of Lianyungang from June 2020 to December 2022 were retrospectively analyzed. Based on whether or not they had SI, they were divided into a SI group (n = 91) and a non-SI group (n = 59). The general data and laboratory indices of the two groups were compared. Logistic regression was used to analyze the factors influencing SI in adolescent patients with depression, a nomogram prediction model was constructed based on the analysis results, and internal evaluation was performed. Receiver operating characteristic and calibration curves were used to evaluate the model’s efficacy, and the clinical application value was evaluated using decision curve analysis (DCA).
There were differences in trauma history, triggers, serum ferritin levels (SF), high-sensitivity C-reactive protein levels (hs-CRP), and high-density lipoprotein (HDL-C) levels between the two groups (P < 0.05). Logistic regression analysis showed that trauma history, predisposing factors, SF, hs-CRP, and HDL-C were factors influencing SI in adolescent patients with depression. The area under the curve of the nomogram prediction model was 0.831 (95%CI: 0.763–0.899), sensitivity was 0.912, and specificity was 0.678. The higher net benefit of the DCA and the average absolute error of the calibration curve were 0.043, indicating that the model had a good fit.
The nomogram prediction model based on trauma history, triggers, ferritin, serum hs-CRP, and HDL-C levels can effectively predict the risk of SI in adolescent patients with depression.
Core Tip: Depression is one of the most serious mental health diseases affecting adolescents. Most adolescents with depression exhibit strong suicidal ideation (SI). This study retrospectively analyzed data from 150 adolescents with depression. According to whether they had SI, they were divided into SI and non-SI groups. Based on previous studies combined with laboratory indicators, the risk factors for SI in adolescent patients with depression were evaluated, and a nomogram model for predicting SI in such patients was developed. The results of this study demonstrate that the model has good prediction accuracy.
- Citation: Zhou JC, Cao Y, Xu XY, Xian ZP. Analysis of risk factors of suicidal ideation in adolescent patients with depression and construction of prediction model. World J Psychiatry 2024; 14(3): 388-397
- URL: https://www.wjgnet.com/2220-3206/full/v14/i3/388.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i3.388
Major depressive disorder (MDD) is a common mental illness characterized by low mood, loss of interest, and lack of pleasure[1]. Studies have shown that more than half of the population between the ages of 9 and 21 meets at least one of the diagnostic criteria; if unclear diagnoses are included, the proportion exceeds 80%[2,3]. This indicates that the prevalence of mental disorders, particularly depression, is gradually increasing in younger individuals. Currently, the prevalence of depression in adolescents is approximately 8%–23.9%[4]. Under the influence of depression, this group experiences a series of psychosocial problems such as weariness, interpersonal difficulties, mobile phone addiction, violence, self-mutilation, and suicide in severe cases[5]. Recently, adolescent suicides have ranked second among the causes of death in this age group[6].
Suicidal ideation (SI) refers to the idea or behavior of losing life expectations without necessarily causing physical harm[7]. Its manifestations range from brief and vague to very specific ideas. Specific ideas include the choice of program, planning, and completion of the entire suicide process. Although SI is not an actual suicide action, it has a particular predictive effect on suicidal behavior[8]. Studies have shown the emergence of SI in many elements, such as emotional regulation disorders, early trauma experience, family upbringing, adverse life events, and peer relationships, among which early trauma experience plays a role[9]. In addition, studies have shown that depression may be a susceptibility factor for SI[10]. The World Health Organization has reported that 62% of adolescents with depression have strong SI and suicidal behavior[6]. Therefore, reducing SI in patients with depression is an important goal in the treatment of depression and is also an important sign of depression alleviation.
Logistic regression is often used to identify the factors influencing SI in patients with depression; however, it cannot directly reflect the influence of individual factors on the results. A prediction model can be developed using a nomogram, which has been widely used as a reliable tool for predicting risk[11] and has good prognostic value in disease prediction. However, nomograms are rarely used in the field of mental illness.
Based on previous studies, this study combined biological factors to determine the risk of SI in adolescent patients with depression and developed a nomogram model to predict SI in such patients. We hope this study will help quickly diagnose depression in adolescent patients with a high risk of SI and prevent possible suicide events.
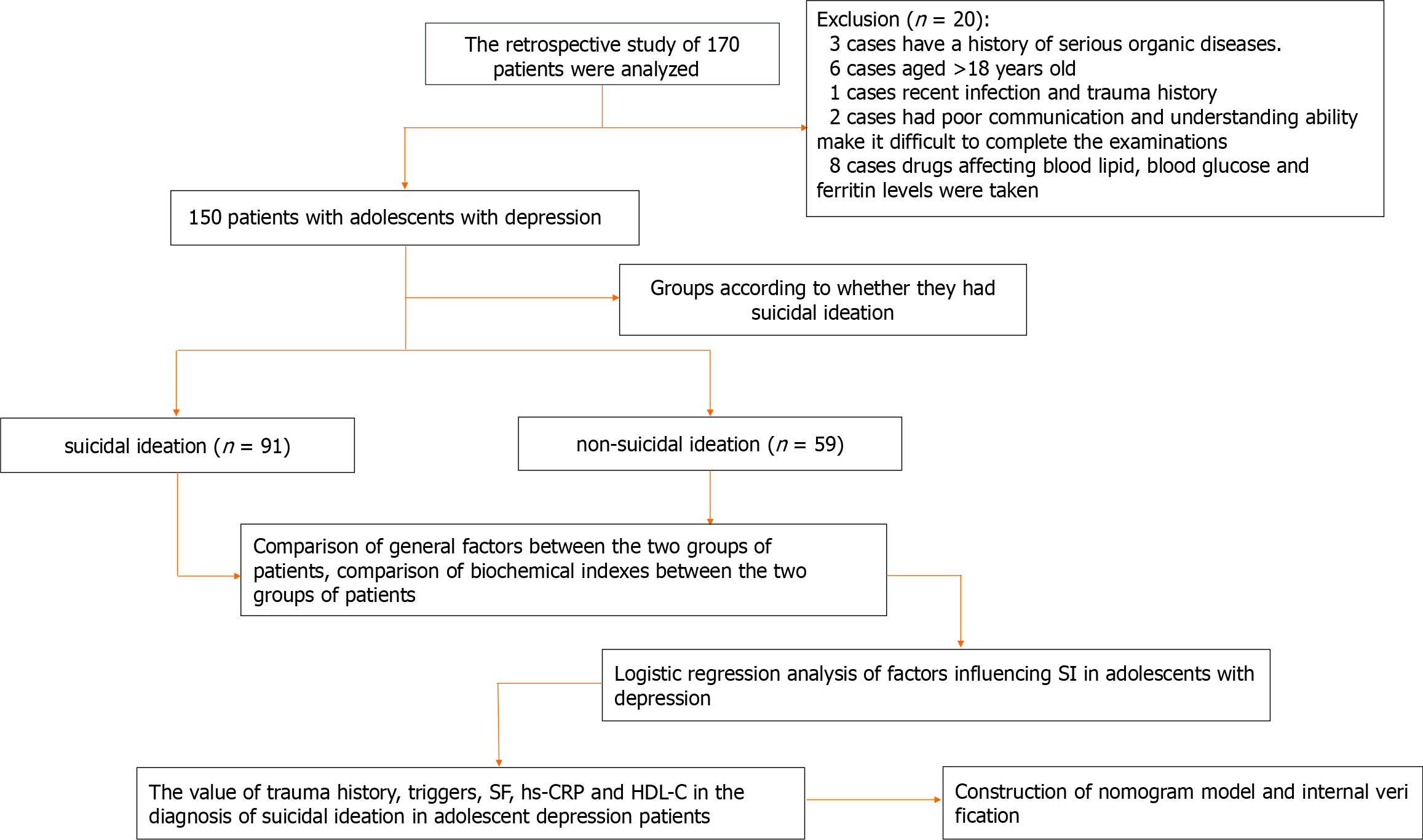
The retrospective study method was adopted. The research process is illustrated in Figure 1. Adolescent patients with depression who received treatment at the First People's Hospital of Lianyungang from June 2020 to December 2022 were selected as research participants. A total of 150 patients were included and divided into the SI (n = 91) and non-SI (n = 59) groups according to whether they had SI. The inclusion criteria were: (1) Patients diagnosed by two psychiatrists who met the criteria for depressive episodes according to the International Classification and Diagnostic Criteria of Mental Disorders 10th Edition[12]. Among the included patients, the SI grouping was performed according to the fifth edition of the American Diagnostic and Statistical Manual of Mental Disorders[13]; (2) Either item 4 or 5 of the Beck Suicidal Ideation Scale-Chinese Version was found to be "weak" or above; (3) Age 12–18 years; and (4) No drugs affecting blood lipid, blood sugar, or ferritin levels were taken during the first three months of enrollment. Exclusion criteria were patients with: (1) A history of severe organic disease; (2) recent infection and history of trauma; (3) depression caused by psychoactive substances; (4) anemia, endocrine system diseases, hyperlipidemia, and recent use of lipid-lowering and diuretic drugs; (5) severe cognitive dysfunction; and (6) poor communication and understanding skills that make it difficult to complete the assessments.
The patients' medical data, including basic patient information, medical records, and test results, were obtained from the hospital records. The collection steps included: (1) Collecting the basic information of patients, including age, sex, and education level; (2) reviewing the patient's electronic medical record. The attending psychiatrist, with more than two years of working experience, summarized the patient's case data, including the disease course and the child’s position in the family, according to the medical record. The presence of a single parent, triggers (frustration in learning, family history of mental illness, poor interpersonal relationships, broken relationships, parent-child tension, etc.)[14], history of trauma, and SI were also recorded; (3) The Beck Scale for Suicide Ideation[15] consists of 19 items with three possible ratings. The corresponding scores from lowest to highest are 0, 1, and 2. The higher the score, the greater the suicide risk. If item 4 or 5 of the scale shows "weak" or above, the patient can be judged to have SI. The strength of SI is obtained according to the total score of items 1–5 on the scale, which varies between 5 and 15 points. The higher the score, the stronger the SI; and (4) Test results of patients who fasted 12 h after admission were retrieved from the hospital records and included blood lipids, serum high-sensitivity C-reactive protein (hs-CRP), glutamic oxaloacetic transaminase, and serotonin levels.
All collected medical records were sorted into Excel format, and SPSS software (v.26.0) was used for statistical analysis. The chi-square test was used for count data, the t-test for measurement data, and the independent sample t-test for continuous variables. Categorical variables are expressed as percentages of positive cases. The measurement data with a normal distribution were expressed as mean ± SD, and the χ2 test was used. All tests were two-sided. P < 0.05 was set as a statistically significant difference.
Based on the results of the multivariate analysis, a nomogram prediction model was constructed using R software. To verify its predictive accuracy, bootstrap sampling was used to conduct internal validation 1000 times, and the receiver operating characteristic (ROC) curve, decision curve analysis (DCA), and calibration curve were used to evaluate the predictive efficacy and clinical utility of the nomogram.
The statistical analysis showed that compared with the non-SI group, patients in the SI group had more trauma history and predisposing factors, and the difference was significant (P < 0.05) (Table 1).
| Characteristic | SI group (n = 91) | Non-SI group (n = 59) | t/χ2 value | P value |
| Sex | ||||
| Male | 25 (27.47) | 20 (33.90) | 0.704 | 0.402 |
| Women | 66 (72.53) | 39 (66.10) | ||
| Age | 14.165 ± 0.793 | 14.220 ± 0.789 | 0.186 | 0.157 |
| Trauma history | ||||
| Yes | 39 (42.86) | 8 (13.56) | 14.28 | 0.001 |
| No | 52 (57.14) | 51 (86.44) | ||
| Only child | ||||
| Yes | 60 (65.93) | 40 (67.80) | 0.056 | 0.813 |
| No | 31 (34.07) | 19 (32.20) | ||
| Single parent | ||||
| Yes | 19 (20.88) | 11 (18.64) | 0.112 | 0.738 |
| No | 72 (79.12) | 48 (81.36) | ||
| First-episode | ||||
| Yes | 66 (72.53) | 46 (77.97) | 0.560 | 0.454 |
| No | 25 (27.47) | 13 (22.03) | ||
| Are there triggers | ||||
| Yes | 42 (46.15) | 23 (38.98) | 13.328 | 0.039 |
| No | 49 (53.85) | 36 (61.02) | ||
| Ethnic groups | ||||
| Han nationality | 82 (90.11) | 53 (89.83) | 0.003 | 0.956 |
| Ethnic minorities | 9 (9.89) | 6 (10.17) | ||
| Educational level | ||||
| High school and above | 39 (42.86) | 21 (35.59) | 0.787 | 0.375 |
| Junior high school and below | 52 (57.14) | 38 (64.41) | ||
| Religious belief | ||||
| Yes | 3 (3.30) | 4 (6.78) | 0.976 | 0.323 |
| No | 88 (96.70) | 55 (93.22) | ||
| Residential area | ||||
| City | 61 (67.03) | 36 (61.02) | 0.567 | 0.451 |
| Rural | 30 (32.97) | 23 (38.98) | ||
| Economic situation | ||||
| Poor | 15 (16.48) | 8 (13.56) | 0.284 | 0.868 |
| Medium | 55 (60.44) | 36 (61.02) | ||
| Better | 21 (23.08) | 15 (25.42) | ||
| Father's education level | ||||
| Junior high school and below | 65 (71.43) | 42 (71.19) | 0.001 | 0.974 |
| High school and above | 26 (28.57) | 17 (28.81) | ||
| Mother's educational level | ||||
| Junior high school and below | 63 (69.23) | 43 (72.88) | 0.230 | 0.631 |
| High school and above | 28 (30.77) | 16 (27.12) |
According to the comparison of laboratory indicators between the two groups of patients, the study found that the levels of serum ferritin (SF) and hs-CRP in the SI group were higher than those in the non-SI group (P < 0.05). In addition, high-density lipoprotein (HDL-C) in patients with SI was lower than that in patients without SI (P < 0.05), while there were no statistically significant differences between the other indicators (Table 2).
| Index | SI group | Non-SI group | t value | P value |
| SF (μg/L) | 71.010 ± 13.278 | 58.422 ± 17.842 | -4.945 | 0.015 |
| Folic acid (mmol/L) | 4.350 ± 0.139 | 4.436 ± 0.172 | 11.864 | 0.053 |
| Vitamin D3 (mg/L) | 12.773 ± 0.836 | 13.200 ± 0.846 | 4.366 | 0.054 |
| hs-CRP (mg/L) | 4.115 ± 1.497 | 3.423 ± 1.012 | -3.115 | 0.020 |
| UA (mmol/L) | 335.989 ± 16.667 | 330.924 ± 16.875 | -1.809 | 0.861 |
| TG (mmol/L) | 1.073 ± 0.103 | 1.061 ± 0.105 | -0.656 | 0.794 |
| TC (mmol/L) | 3.737 ± 0.048 | 3.737 ± 0.047 | -0.023 | 0.949 |
| HDL-C (mmol/L) | 1.039 ± 0.210 | 1.174 ± 0.282 | 3.351 | 0.009 |
| LDL-C (mmol/L) | 2.079 ± 0.055 | 2.076 ± 0.061 | -0.313 | 0.411 |
| TP (g/L) | 76.312 ± 1.088 | 75.951 ± 1.230 | -1.881 | 0.062 |
| ALB (g/L) | 47.230 ± 0.916 | 46.716 ± 1.088 | -3.549 | 0.081 |
| TBIL (μmol/L) | 14.964 ± 0.218 | 14.820 ± 0.203 | -4.045 | 0.121 |
| AST (U/L) | 42.325 ± 0.543 | 41.897 ± 0.501 | -4.852 | 0.089 |
| TSH (mmol/L) | 150.080 ± 1.180 | 149.890 ± 1.109 | 0.986 | 0.326 |
| T3 (pmol/L) | 1.519 ± 0.292 | 1.514 ± 0.246 | -0.124 | 0.902 |
| T4 [M(Q)pmol/L] | 86.850 ± 18.366 | 87.285 ± 19.229 | 0.139 | 0.889 |
| FT3 (pmol/L) | 4.317 ± 0.501 | 4.250 ± 0.437 | 1.913 | 0.050 |
| FT4 (pmol/L) | 11.339 ± 1.965 | 11.244 ± 2.040 | -0.284 | 0.777 |
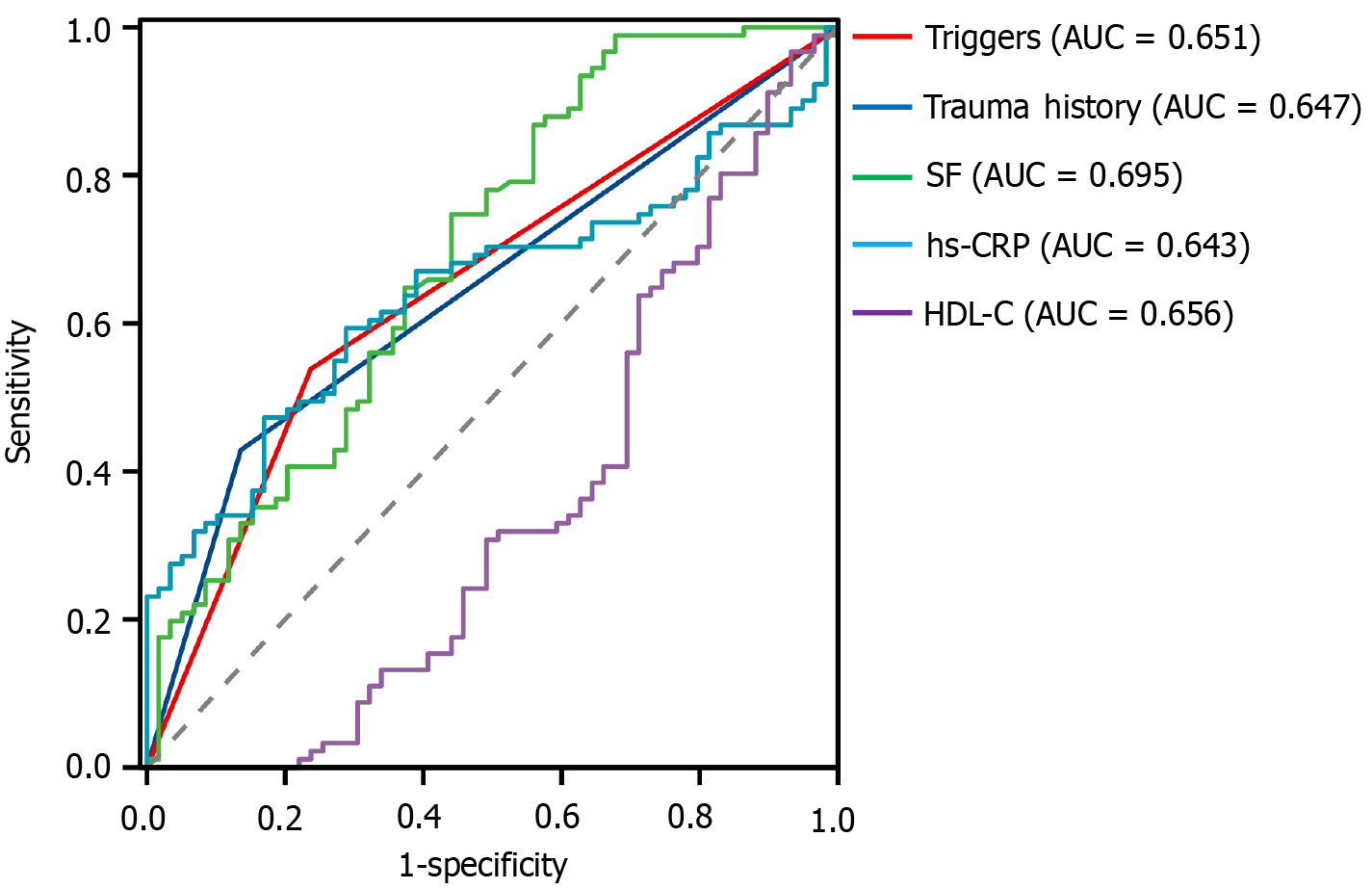
Indicators with significant differences were included in the logistic regression analysis. Among them, the presence or absence of SI (yes = 1, no = 0) was used as the dependent variable, and history of trauma (yes = 1, no = 0), presence or absence of triggers (yes = 1, no = 0), and SF, hs-CRP, and HDL-C levels were used as independent variables. The results showed that a history of trauma, triggers, SF > 49.76, and hs-CRP > 3.829 were risk factors for SI in adolescents with depression [odds ratio (OR) > 1, P < 0.05]. An HDL-C level > 0.683 was a protective factor against SI in adolescents with depression (OR < 1, P < 0.05) (Table 3). The ROC curve was used to evaluate the diagnostic value of each index. The highest area under the ROC curve (AUC) for SF was 0.695; the others are shown in Table 4 and Figure 2.
| Independent variable | B | SE | Wald | P value | OR | 95%CI |
| Trauma history | 1.106 | 0.519 | 4.552 | 0.033 | 3.023 | 1.094–8.354 |
| Triggers | 1.311 | 0.461 | 8.107 | 0.004 | 3.711 | 1.505–9.153 |
| SF (μg/L) | 0.051 | 0.014 | 12.598 | 0.000 | 1.052 | 1.023–1.082 |
| hs-CRP (mg/L) | 0.453 | 0.172 | 6.927 | 0.008 | 1.573 | 1.123–2.205 |
| HDL-C (mmol/L) | -2.104 | 0.852 | 6.095 | 0.014 | 0.122 | 0.023–0.648 |
| FT3 (pmol/L) | -1.217 | 0.502 | 5.886 | 0.078 | 0.296 | 0.111–0.791 |
| Constant | -2.293 | 1.609 | 2.031 | 0.154 | 0.101 | - |
| Independent variable | Cutoff | AUC | Sensitivity | Specificity | Youden index | P value | 95%CI |
| Trauma history | - | 0.647 | 0.429 | 0.864 | 0.293 | 0.002 | 0.558–0.734 |
| Triggers | - | 0.651 | 0.538 | 0.763 | 0.301 | 0.002 | 0.562–0.740 |
| SF (μg/L) | 49.76 | 0.695 | 0.989 | 0.322 | 0.311 | 0.000 | 0.607–0.783 |
| hs-CRP (mg/L) | 3.829 | 0.643 | 0.593 | 0.712 | 0.305 | 0.003 | 0.556–0.731 |
| HDL-C (mmol/L) | 0.683 | 0.656 | 0.967 | 0.068 | 0.035 | 0.001 | 0.250–0.439 |
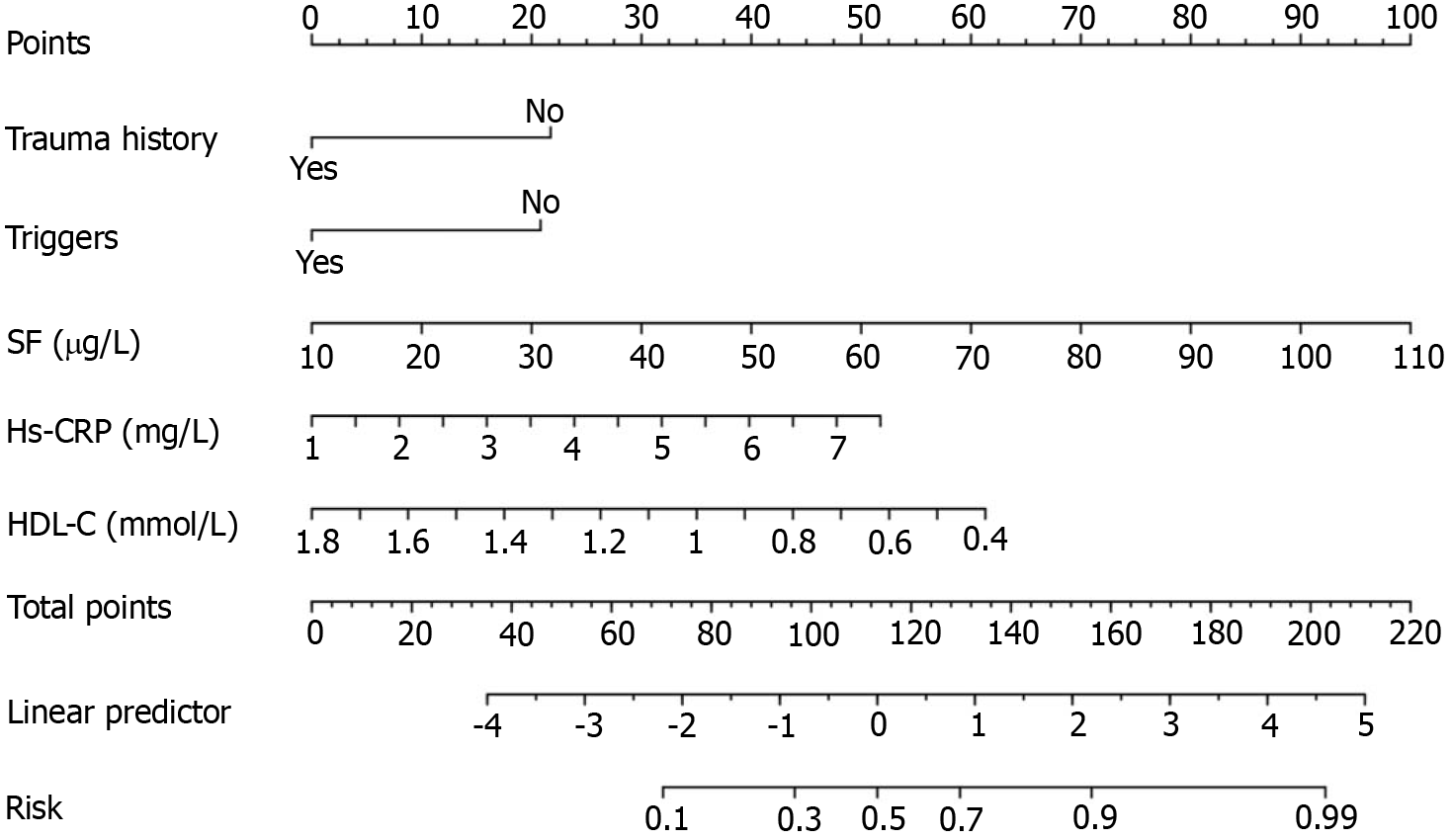
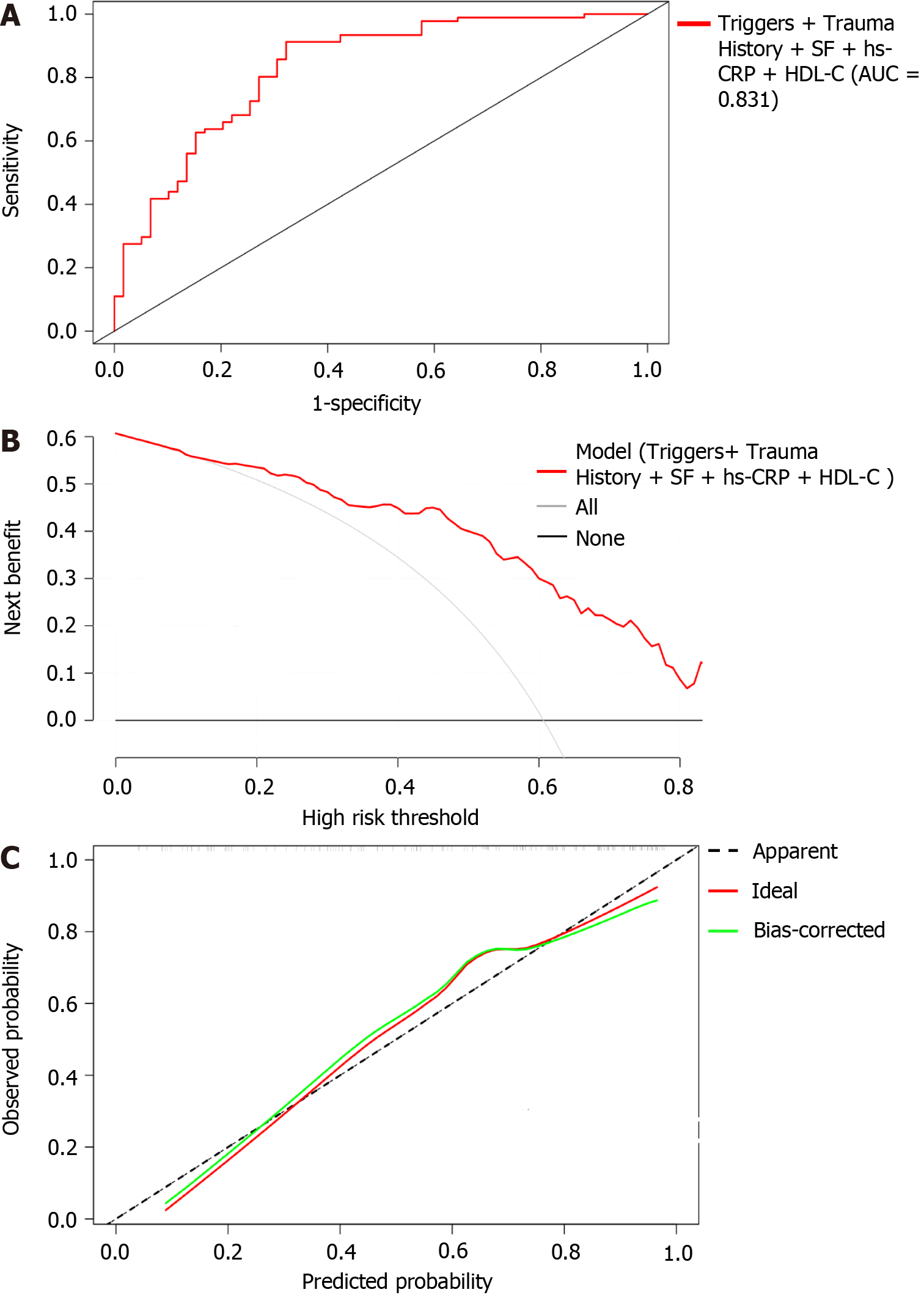
A nomogram model was constructed based on the results of the multivariate analysis (Figure 3). Internal validation used bootstrap sampling 1000 times, and the AUC, DCA, and calibration curve were used to evaluate the efficacy of the nomogram. The AUC was 0.831, the sensitivity was 0.912, and the specificity was 0.678, with a 95%CI of 0.763–0.899, indicating that the model had predictive capability, as shown in Figure 4A. According to the DCA, the net benefit of the model was greater within a larger threshold range, indicating better clinical efficacy of the model (Figure 4B). In addition, the calibration curve further showed that the predicted value was in good agreement with the measured value, and the average absolute error (0.043) was small, indicating that the nomogram model had good predictive efficacy (Figure 4C).
In this study, we analyzed the occurrence of SI in adolescent patients with depression and developed a nomogram model with good predictive efficacy to predict SI risk.
In this study, 60.67% (91/150) of adolescent patients with depression had SI, which is consistent with a previous study[16]. In our study, female patients showed higher SI than male patients, consistent with the results of domestic and foreign studies[17,18]. This may be related to the hormone levels of female patients. The proportion of patients with SI with a history of trauma was significantly higher than that in the control group, suggesting that childhood trauma is a risk factor[19]. In addition, the study also found that a higher proportion of patients with various triggers had SI than those without triggers, indicating that triggers play a role in SI in adolescent patients with depression[20].
Ferritin is an important marker of inflammation and oxidative stress. It is also a unique protein that stores iron and is often used to assess the level of iron stored in the body. Studies have shown that the mechanism underlying increased SF levels in patients with depression is mainly an oxidative stress reaction caused by increased ferritin[21]. Oxidative stress is directly related to the pathogenesis of depression, indicating that ferritin can indirectly affect the occurrence and development of depressive symptoms by triggering an oxidative stress response. In this study, the SI group had significantly higher SF levels than the non-SI group, suggesting that SF levels are associated with depression.
Furthermore, according to previous studies, elevated serum hs-CRP levels can oversecrete inflammatory cytokines, causing dysfunction of the 5-hydroxytryptamine and noradrenaline systems, thereby inducing depressive symptoms[22]. According to the study of Tabaeizadeh et al[23], there is a correlation between hs-CRP levels and depression in adolescent girls. Our study found that adolescents with depression and SI had higher hs-CRP levels. These results indicate that hs-CRP levels are associated with depression. In recent years, an increasing number of studies on the relationship between HDL-C and depression accompanied by suicidal thoughts have shown that patients with depression have a unique lipid metabolism profile compared to those without depression[24]. Our study showed that the HDL-C level in adolescent patients with depression and SI was lower than that in the non-SI group, which is consistent with previous studies. For example, Maes et al[25] showed that serum HDL-C levels in patients with depression and SI were low. This suggests that HDL-C may be a biological marker of MDD accompanied by SI. Simultaneously, it provides a new therapeutic target for treating depression and depressive symptoms, especially in patients with depression and SI, by regulating lipid levels through various mechanisms[26,27].
Based on the related risk factors for SI in adolescent patients with depression, we developed a risk prediction model and conducted internal validation. The calibration curve suggests good consistency between the values predicted by the model and measured values, and the DCA suggests that the net benefit of the model is better when the threshold is above 20%, indicating that the model has high clinical practicability. These results indicate that the model has good predictive efficacy. To the best of our knowledge, this is the first nomogram model that includes sociological factors and laboratory indicators to predict SI in patients with depression. This can help implement early clinical measures to reduce suicide mortality in adolescent patients with depression.
This study has some limitations. First, the participants were adolescents with depression. This is a relatively special group, as they are in a period of growth and development; therefore, fluctuations in hormone levels can significantly affect the results. Second, the dietary habits and nutritional status of patients were not considered. This may affect the levels of iron, hs-CRP, and HDL-C in the body, which may have caused bias in the study results. Further external validation is required in future studies. Finally, the insufficient sample size may have affected the validity of the nomogram model.
In conclusion, this study found that trauma history, predisposing factors, ferritin level, hs-CRP level, and HDL-C level may be early factors influencing SI in adolescent patients with depression. The nomogram model can effectively predict the occurrence of SI in adolescent patients with depression, which can help to quickly diagnose adolescent patients with depression at high risk of SI to prevent suicidal events.
Depression is one of the most severe diseases affecting the mental health of adolescents. Most adolescents with depression have suicidal ideation (SI). However, few studies have focused on the factors related to SI, and there is a lack of effective predictive models.
This study determined the factors influencing SI in adolescent patients with depression and construct a risk prediction model to provide a theoretical basis for prevention and intervention.
This study aimed to construct a risk prediction model for SI in adolescents with depression and provide an assessment tool for early screening.
Based on a retrospective analysis of social factors and laboratory indicators of 150 adolescent patients with depression and SI, this study constructed and internally validated a risk prediction model.
Studies have shown that trauma history, predisposing factors, and serum ferritin levels (SF), high-sensitivity C-reactive protein levels (hs-CRP), and high-density lipoprotein (HDL-C) levels influence SI in adolescents with depression. The AUC of the nomogram prediction model was 0.831 (95%CI: 0.763–0.899), the sensitivity was 0.912, and the specificity was 0.678. The high net benefit of the DCA and the average absolute error of the calibration curve were 0.043, indicating that the model had a good fit.
The nomogram model based on trauma history, predisposing factors, SF, hs-CRP levels, and HDL-C levels can effectively predict the occurrence of SI in adolescents with depression, which can help in implementing early clinical measures to reduce suicide mortality in adolescents with depression.
According to the general data and laboratory indicators of adolescents with depression, we identified risk factors for SI and used them to develop an effective predictive model for quick detection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Marasy SA, Egypt S-Editor: Wang JL L-Editor: A P-Editor: Zhao S
| 1. | Yang L, Zhao Y, Wang Y, Liu L, Zhang X, Li B, Cui R. The Effects of Psychological Stress on Depression. Curr Neuropharmacol. 2015;13:494-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 346] [Cited by in F6Publishing: 287] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 2. | GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 436] [Cited by in F6Publishing: 1119] [Article Influence: 559.5] [Reference Citation Analysis (0)] |
| 3. | Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2011;50:252-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 182] [Cited by in F6Publishing: 180] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 4. | Naicker K, Galambos NL, Zeng Y, Senthilselvan A, Colman I. Social, demographic, and health outcomes in the 10 years following adolescent depression. J Adolesc Health. 2013;52:533-538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 173] [Cited by in F6Publishing: 181] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 5. | Grossberg A, Rice T. Depression and Suicidal Behavior in Adolescents. Med Clin North Am. 2023;107:169-182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Mojtabai R, Olfson M, Han B. National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics. 2016;138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 753] [Cited by in F6Publishing: 725] [Article Influence: 90.6] [Reference Citation Analysis (0)] |
| 7. | Wang M, Qin A, Wei Z, Sun L. Differentiating the associations between alcohol use, cigarette smoking, and conditional suicidal behaviors among adolescents. J Affect Disord. 2023;341:112-118. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 8. | Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018;212:279-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 285] [Cited by in F6Publishing: 373] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 9. | Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020;107:234-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 267] [Cited by in F6Publishing: 731] [Article Influence: 182.8] [Reference Citation Analysis (0)] |
| 10. | Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 319] [Cited by in F6Publishing: 447] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 11. | Luo Y, Lai Q, Huang H, Luo J, Miao J, Liao R, Yang Z, Zhang L. Risk factor analysis and nomogram construction for predicting suicidal ideation in patients with cancer. BMC Psychiatry. 2022;22:353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Innes K, Hooper J, Bramley M, DahDah P. Creation of a clinical classification. International statistical classification of diseases and related health problems--10th revision, Australian modification (ICD-10-AM). Health Inf Manag. 1997;27:31-38. [PubMed] [Cited in This Article: ] |
| 13. | First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. 2013;201:727-729. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 14. | Olié E, Le Bars E, Deverdun J, Oppenheim C, Courtet P, Cachia A. The effect of early trauma on suicidal vulnerability depends on fronto-insular sulcation. Cereb Cortex. 2023;33:823-830. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 15. | Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343-352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1857] [Cited by in F6Publishing: 1808] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 16. | Kang C, Zheng Y, Yang L, Wang X, Zhao N, Guan TF, Qiu S, Shi J, Hu J. Prevalence, risk factors and clinical correlates of suicidal ideation in adolescent patients with depression in a large sample of Chinese. J Affect Disord. 2021;290:272-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947-957. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1753] [Cited by in F6Publishing: 1839] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 18. | Su Y, Ye C, Xin Q, Si T. Major depressive disorder with suicidal ideation or behavior in Chinese population: A scoping review of current evidence on disease assessment, burden, treatment and risk factors. J Affect Disord. 2023;340:732-742. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 19. | Misiak B, Szewczuk-Bogusławska M, Samochowiec J, Moustafa AA, Gawęda Ł. Unraveling the complexity of associations between a history of childhood trauma, psychotic-like experiences, depression and non-suicidal self-injury: A network analysis. J Affect Disord. 2023;337:11-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 20. | Itzhaky L, Shahar G, Stein D, Fennig S. In Eating-Disordered Inpatient Adolescents, Self-Criticism Predicts Nonsuicidal Self-Injury. Suicide Life Threat Behav. 2016;46:385-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Munkholm K, Jacoby AS, Vinberg M, Kessing LV. Ferritin as a potential disease marker in patients with bipolar disorder. J Affect Disord. 2023;332:247-253. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 22. | Chen X, Pu J, Liu Y, Tian L, Chen Y, Gui S, Xu S, Song X, Xie P. Increased C-reactive protein concentrations were associated with suicidal behavior in patients with depressive disorders: a meta-analysis. Psychiatry Res. 2020;292:113320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Tabatabaeizadeh SA, Abdizadeh MF, Meshkat Z, Khodashenas E, Darroudi S, Fazeli M, Ferns GA, Avan A, Ghayour-Mobarhan M. There is an association between serum high-sensitivity C-reactive protein (hs-CRP) concentrations and depression score in adolescent girls. Psychoneuroendocrinology. 2018;88:102-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 24. | Bot M, Milaneschi Y, Al-Shehri T, Amin N, Garmaeva S, Onderwater GLJ, Pool R, Thesing CS, Vijfhuizen LS, Vogelzangs N, Arts ICW, Demirkan A, van Duijn C, van Greevenbroek M, van der Kallen CJH, Köhler S, Ligthart L, van den Maagdenberg AMJM, Mook-Kanamori DO, de Mutsert R, Tiemeier H, Schram MT, Stehouwer CDA, Terwindt GM, Willems van Dijk K, Fu J, Zhernakova A, Beekman M, Slagboom PE, Boomsma DI, Penninx BWJH; BBMRI-NL Metabolomics Consortium. Metabolomics Profile in Depression: A Pooled Analysis of 230 Metabolic Markers in 5283 Cases With Depression and 10,145 Controls. Biol Psychiatry. 2020;87:409-418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 102] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 25. | Maes M, Smith R, Christophe A, Vandoolaeghe E, Van Gastel A, Neels H, Demedts P, Wauters A, Meltzer HY. Lower serum high-density lipoprotein cholesterol (HDL-C) in major depression and in depressed men with serious suicidal attempts: relationship with immune-inflammatory markers. Acta Psychiatr Scand. 1997;95:212-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 197] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 26. | Lee MC, Peng TR, Lee CH, Wang JY, Lee JA, Chen SM, Shiang JC. Statin use and depression risk: A systematic review and meta-analysis. J Affect Disord. 2021;282:308-315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Ghanizadeh A, Hedayati A. Augmentation of fluoxetine with lovastatin for treating major depressive disorder, a randomized double-blind placebo controlled-clinical trial. Depress Anxiety. 2013;30:1084-1088. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |