Published online Mar 24, 2017. doi: 10.5410/wjcu.v6.i1.30
Peer-review started: December 28, 2016
First decision: January 16, 2017
Revised: January 21, 2017
Accepted: February 20, 2017
Article in press: February 21, 2017
Published online: March 24, 2017
Processing time: 68 Days and 23.5 Hours
Enterovesical fistulae secondary to benign or malignant bowel disease are not uncommonly reported in the literature. However, bladder malignancy as the primary pathology is exceedingly rare. We report a case of muscle invasive urothelial carcinoma of bladder with an enterovesical fistula to a loop of small bowel. The patient first presented with signs and symptoms of per rectal bleeding, haematuria, pneumaturia, faecaluria and rectal micturition. Her initial biochemistry test revealed significant metabolic acidosis with normal anion gap and hypokalemia. A computed tomography abdomen/pelvis with rectal contrast demonstrated an enterovesical fistula from the dome of bladder to a loop of small bowel. The patient underwent radical cystectomy with en-bloc resection of a loop of involved ileum and sigmoid colon due to the intraoperative findings of the sigmoid colon adherent to the tumour. The published literature is reviewed, focusing on the incidence, diagnostic modality and treatment strategies available for this rare condition.
Core tip: A 68-year-old lady presented with per rectal bleeding and haematuria. Other important history includes her reporting diarrhea with associated weight loss over the last 3 mo and faecaluria, pneumaturia and rectal micturition. On presentation, she was found to be in severe metabolic acidosis with hypokalemia. A computed tomography scan with rectal contrast showed an enterovesical fistula from bladder to a loop of small bowel. She underwent radical cystectomy, en-bloc resection of a loop of the involved small bowel and sigmoid colon with formation of ileal conduit and end-colostomy.
- Citation: Ng ZQ, Low WKW, Jr S, Subramanian P, Stein J. Radical cystectomy and en-bloc resection of enterovesical fistula from bladder cancer. World J Clin Urol 2017; 6(1): 30-33
- URL: https://www.wjgnet.com/2219-2816/full/v6/i1/30.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v6.i1.30
Enterovesical fistulae (EVF) are not uncommon in the setting of colonic diseases such as inflammation and malignancy. Nevertheless, EVF secondary to a primary urological malignancy is extremely rare with an estimated incidence of 0.5 per 100000[1]. We herein report a patient who presented initially with per rectal bleeding and haematuria and metabolic acidosis with normal anion gap. During the work-up, an EVF was found caused by a urothelial carcinoma of the bladder.
A 68-year-old female presented with per rectal (PR) bleeding and haematuria. She had been suffering from diarrhea and with associated 10 kg of weight loss within the last three months, and was profoundly hypokalaemic on presentation (potassium 2.4 mmol/L). She had also reported faecaluria, pneumaturia and recently noticed that she had been passing urine through the rectum. However, she denied any symptoms of recurrent urinary tract infections. A cystoscopy done 4 years previously for investigation of haematuria found an erythematous and velvety patch on the posterior bladder wall which was biopsied at the time and only showed chronic inflammation with no evidence of malignancy. Urine cytology was also negative for malignancy.
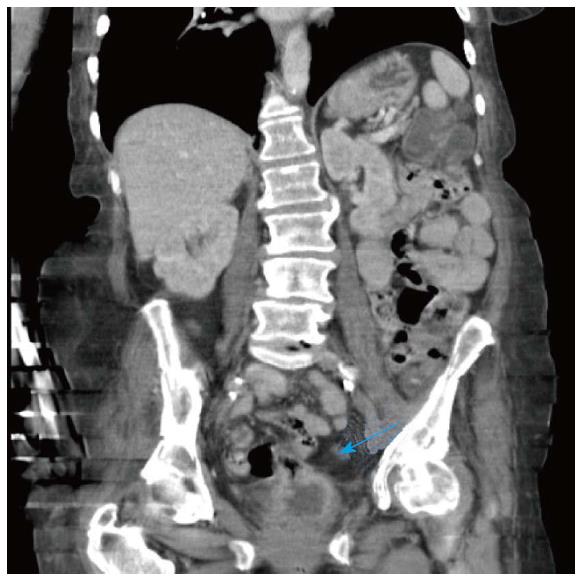
On examination, her vital signs were stable and she was afebrile. Her abdomen was soft with mild generalized tenderness. PR examination was unremarkable. Biochemical tests revealed metabolic acidosis with normal anion gap (pH 7.13, bicarbonate 10 mmol/L, hypokalemia and iron deficiency anaemia. The initial unenhanced computed tomography (CT) scan revealed a bladder fistula with possible communication to large bowel. She underwent a colonoscopy which did not show any colonic pathology or evidence of a colovesical fistula. A subsequent CT abdomen/pelvis with rectal contrast showed an EVF from dome of bladder to mid-to-distal ileum (Figure 1). At cystoscopy, the EVF was confirmed to be involving the posterior wall of the bladder within close proximity of the trigone and the right ureteric orifice.
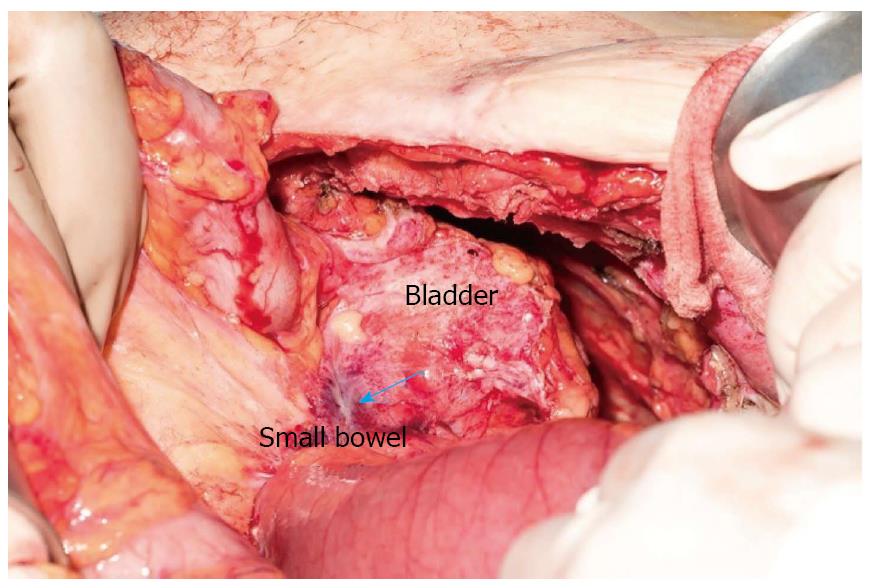
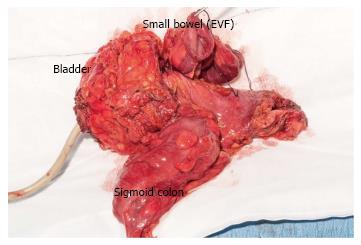
Total parenteral nutrition was initiated to optimize her pre-operatively. A midline laparotomy was performed. Intraoperatively, an EVF was found 15 cm from terminal ileum with the sigmoid colon adherent to bladder (Figure 2). Decision was made to perform an en-bloc radical cystectomy, small bowel resection and sigmoid colectomy with formation of both an ileal conduit and end colostomy (Figure 3). Histopathology confirmed a high-grade urothelial carcinoma with extensive squamous differentiation. There was significant tumour infiltration to the sigmoid colon but there was no evidence of a colovesical fistula.
An enterovesical fistula is an abnormal tract between the epithelialized surface of bowel and the bladder. They are considered a difficult complication of various causes such as inflammation (52%), malignancy (35%) and trauma (16%)[2]. Only a few cases of primary urological EVF have been described in the literature[3-6]. In a series of 100 cases of EVFs, the majority of cases were secondary to an inflammatory bowel condition (61%) and bowel cancer (16%); only 5% were due to bladder carcinoma[6]. The classical symptoms and signs described in the literature include pneumaturia, faecaluria and haematuria as shown in our case[7]. Refractory urinary tract infections[7] were not present in our case. The low intravesical bladder pressure favours unidirectional flow of bowel contents into the bladder. Infrequently, rectal micturition can occur and is reported to be approximately 19% of cases[7]. They may also have a constellation of symptoms such as suprapubic pain, frequency, dysuria and tenesmus, known as Gouverneur syndrome.
The diagnosis of EVF usually relies on a high index of suspicion. Metabolic acidosis with normal anion gap could be indicative of this condition due to loss of bicarbonate or a reduction of renal acid excretion as shown in our case. Typically, this occurs in patients with chronic diarrhea or prolonged exposure of urine to colonic/ileal mucosa[8]. There is no consensus for a diagnostic algorithm. Various diagnostic studies can be considered such as CT scan, MRI, barium enema, cystogram, cystoscopy and colonoscopy. CT and MRI have the advantages of helping in pre-operative planning by clearly defining the fistulous tract and its anatomic relationship with adjacent structures. The distinguishing features on CT scan are air or contrast within the bladder, thickening of bladder wall, or an extraluminal gas-containing mass adjacent to the bladder[9]. A cystoscopy has a diagnostic sensitivity that ranges from 77% to 79%[4] and is usually performed to obtain biopsies from the fistulous tract for histological evaluation. The initial signs under cystoscopy examination maybe subtle, with only a hyperemic area noted in the early stage, and with cystic mucosal hyperplasia or localized granulation tissue at the late stage. Hence, in retrospect, our patient may have had early dysplastic changes on her initial cystoscopy four years ago. Alternatively, cystogram or barium enema will be able to demonstrate the presence of fistulous tract with a sensitivity of 66.6% and 20%-35% respectively[5]. Given that some of the symptoms such as pneumaturia, faecaluria and rectal micturition are not uncommon in cases of colovesical fistula caused by inflammatory or malignant bowel disease, colonoscopy is essential to rule out a synchronous colovesical fistula.
EVF due to malignancy carries a very poor prognosis as by definition the tumour is considered a T4 tumour under the TNM classification due to extravesical spread. The optimal treatment remains an area of debate. Surgical treatment is usually offered to patients. En-bloc resection of surrounding structures that are adherent to it may be necessary to provide an R0 resection and a multidisciplinary approach thereafter for a combination of adjuvant chemo-radiotherapy to improve progression free survival. In patients with intractable symptoms who are poor surgical candidates, octreotide can be considered as a viable therapeutic option in the palliative setting[10].
EVF from a primary urological malignancy remains rare and a high degree of clinical suspicion is required. Pre-operative optimization of nutrition status is paramount for successful reconstruction. The ideal management is surgical intervention and may involve en-bloc resections. A multidisciplinary approach may be required for the best clinical outcome.
A 68-year-old lady who presented initially with per rectal bleeding and haematuria was found that she has been suffering from a 3-mo history of diarrhea and more recently she has been troubled by pneumaturia, faecaluria and rectal micturition.
Pneumaturia, faecaluria and rectal micturition were suggestive of enterovesical fistula.
Colorectal malignancy or inflammatory bowel disease forming a colovesical fistula, inflammatory bowel disease forming an enterovesical fistula.
Metabolic acidosis with normal anion gap.
An enterovesical fistula is seen from the dome of bladder to the terminal ileum.
A high-grade urothelial carcinoma with extensive squamous differentiation.
Radical cystectomy with en-bloc resection of a loop of involved ileum and sigmoid colon with ileal conduit and end colostomy formation.
Enterovesical fistula due to malignancy carries a very poor prognosis as the tumour is considered a T4 tumour. En-bloc resection is usually required to achieve RO resection. If the patient is not a surgical candidate, medical management with octreotide is an alternative palliative option for intractable symptoms.
Enterovesical fistula is an abnormal tract between the epithelialized surface of bowel and the bladder. Enterovesical fistula arising from a primary urological malignancy is extremely rare.
Enterovesical fistula from a primary urological malignancy remains a rare entity and usually requires a high degree of clinical suspicion. Optimization of pre-operative nutritional status is often helpful to achieve good post-operative healing. Often, a multidisciplinary approach involving various subspecialties may need required for the best outcome for the patient.
The case report is well written, clear and concise.
Manuscript source: Unsolicited manuscript
Specialty Type: Urology and Nephrology
Country of Origin: Australia
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Naselli A, Rais-Bahrami S S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Karamchandani MC, West CF. Vesicoenteric fistulas. Am J Surg. 1984;147:681-683. [PubMed] [Cited in This Article: ] |
| 2. | Couris GD, Block MA. Intestinovesical fistula. Surgery. 1963;54:736-742. [PubMed] [Cited in This Article: ] |
| 3. | Sellers W, Fiorelli R. Enterovesical Fistula Secondary to Squamous Cell Carcinoma of the Bladder. Urol Case Rep. 2015;3:201-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Dawam D, Patel S, Kouriefs C, Masood S, Khan O, Sheriff MK. A “urological” enterovesical fistula. J Urol. 2004;172:943-944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Yang CH, Liu KH, Chen TC, Chang PL, Yeh TS. Enterovesical fistula caused by a bladder squamous cell carcinoma. World J Gastroenterol. 2009;15:4215-4217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Carson CC, Malek RS, Remine WH. Urologic aspects of vesicoenteric fistulas. J Urol. 1978;119:744-746. [PubMed] [Cited in This Article: ] |
| 7. | Vidal Sans J, Pradell Teigell J, Palou Redorta J, Villagrasa Serrano M, Banús Gassol JM. Review of 31 vesicointestinal fistulas: diagnosis and management. Eur Urol. 1986;12:21-27. [PubMed] [Cited in This Article: ] |
| 8. | Coelho R, Rodrigues-Pinto E, Cardoso H, Santos-Antunes J, Marques M, Horta e Vale A, Malheiro L, Macedo G. Severe metabolic acidosis: the presenting sign of an enterovesical fistula. Int J Colorectal Dis. 2016;31:785-786. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 9. | Golabek T, Szymanska A, Szopinski T, Bukowczan J, Furmanek M, Powroznik J, Chlosta P. Enterovesical fistulae: aetiology, imaging, and management. Gastroenterol Res Pract. 2013;2013:617967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Shinjo T, Kondo Y, Harada K, Yamazaki J, Okada M. Treatment of malignant enterovesical fistula with octreotide. J Palliat Med. 2009;12:965-967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |