Published online May 9, 2023. doi: 10.5319/wjo.v10.i2.23
Peer-review started: October 13, 2022
First decision: December 13, 2022
Revised: December 17, 2022
Accepted: February 9, 2023
Article in press: February 9, 2023
Published online: May 9, 2023
Lymphangiomas are a group of benign swellings which are commonly seen in children. The most common sites of presentation is the head and neck region, less commonly seen in axilla, chest, liver, spleen, etc. The ideal modality of treatment has always been surgical excision irrespective of the site and age group. But with the advent of minimally invasive surgical techniques, it is now possible to perform excision of parapharyngeal space lesions with minimal morbidity and good clearance.
A 42-year-old male patient who presented with difficulty in swallowing and had undergone surgery twice outside, where Transcervical approach was attempted to remove the parapharyngeal mass, but failed. Magnetic resonance imaging scan demonstrated a 6 cm x 5 cm x 4 cm left parapharyngeal mass. He underwent transoral robotic surgery for the excision of the parapharyngeal lesion and had an uneventful post-operative recovery.
Lymphangiomas are hamartomatous swellings which are benign in nature. The symptoms of the patient with large parapharyngeal mass include dysphagia, dyspnoea and neck swelling. Clinicoradiological evaluation is of utmost im
Core Tip: This report describes a rare case of adult parapharyngeal space lymphangioma. It also emphasizes the role of minimally invasive techniques like transoral robotic surgery for the excision of parapharyngeal space tumors which has resulted in less morbidity in the patients and gives good clearance of tumor.
- Citation: Dabas S, Menon NN, Ranjan R, Gurung B, Shukla H, Sharma AK, Tiwari S, Sinha A, Bhatti SS, Sangal R. Transoral robotic surgery for adult parapharyngeal lymphangioma: A case report. World J Otorhinolaryngol 2023; 10(2): 23-29
- URL: https://www.wjgnet.com/2218-6247/full/v10/i2/23.htm
- DOI: https://dx.doi.org/10.5319/wjo.v10.i2.23
Cystic hygroma, also known as cystic lymphangioma, jugular lymphatic obstructive sequence and hygromacollicysticum, was first described in 1828 by Redenbacher[1]. Only 6% of benign lumps in patients aged less than 20 years are attributable to lymphangiomas[2]. Parapharyngeal space is an extremely rare subsite for lymphangiomas in the head and neck. Other sites include axilla, mediastinum, groin and abdominal cavity[3].
Different etiological and pathogenic factors have been considered causal, including traumatic, infectious and chronic inflammatory factors, as well as alterations in embryological development[4]. In adults, late proliferation of cellular nests of the lymphatic system may appear due to stimulation caused by trauma or infection[5].
Lymphangiomas in the head and neck region commonly develop as an asymptomatic neck mass around 2 years of age.
The imaging modality preferred for lymphangiomas include ultrasound (USG) supplemented by computerized tomography (CT) and magnetic resonance imaging (MRI) scans for obtaining more information about the structural features, internal as well as peripheral enhancement patterns[6].
The most common treatment modality includes surgical excision of the mass. The other treatment modalities include aspiration, sclerotherapy, steroids, laser and radiotherapy.
We here describe a rare case of adult parapharyngeal space lymphangioma which was managed with transoral robotic surgery.
A 42-year-old male patient presented to our outpatient department with chief complaint of difficulty in swallowing both solids and liquids for the past 2 months.
The patient had dysphagia in the past 2 months with no associated odynophagia, respiratory difficulty or neck mass. He had a history of transcervical surgery twice outside for the same reason, which resulted in incomplete removal of the concerned pathology. No surgical records of the previous surgeries were available at the time he presented to us.
The patient had no history of any significant comorbidities.
Vital signs recorded were as follows: temperature 36.5 ℃, pulse rate 88/ min, blood pressure 130/80 mmHg and respiratory rate 18 /min. On clinical examination, a submucosal bulge was noted in the left tonsillar area. No swelling was however palpable in the neck.
Results of routine blood tests as part of pre-operative work-up were within normal limits.
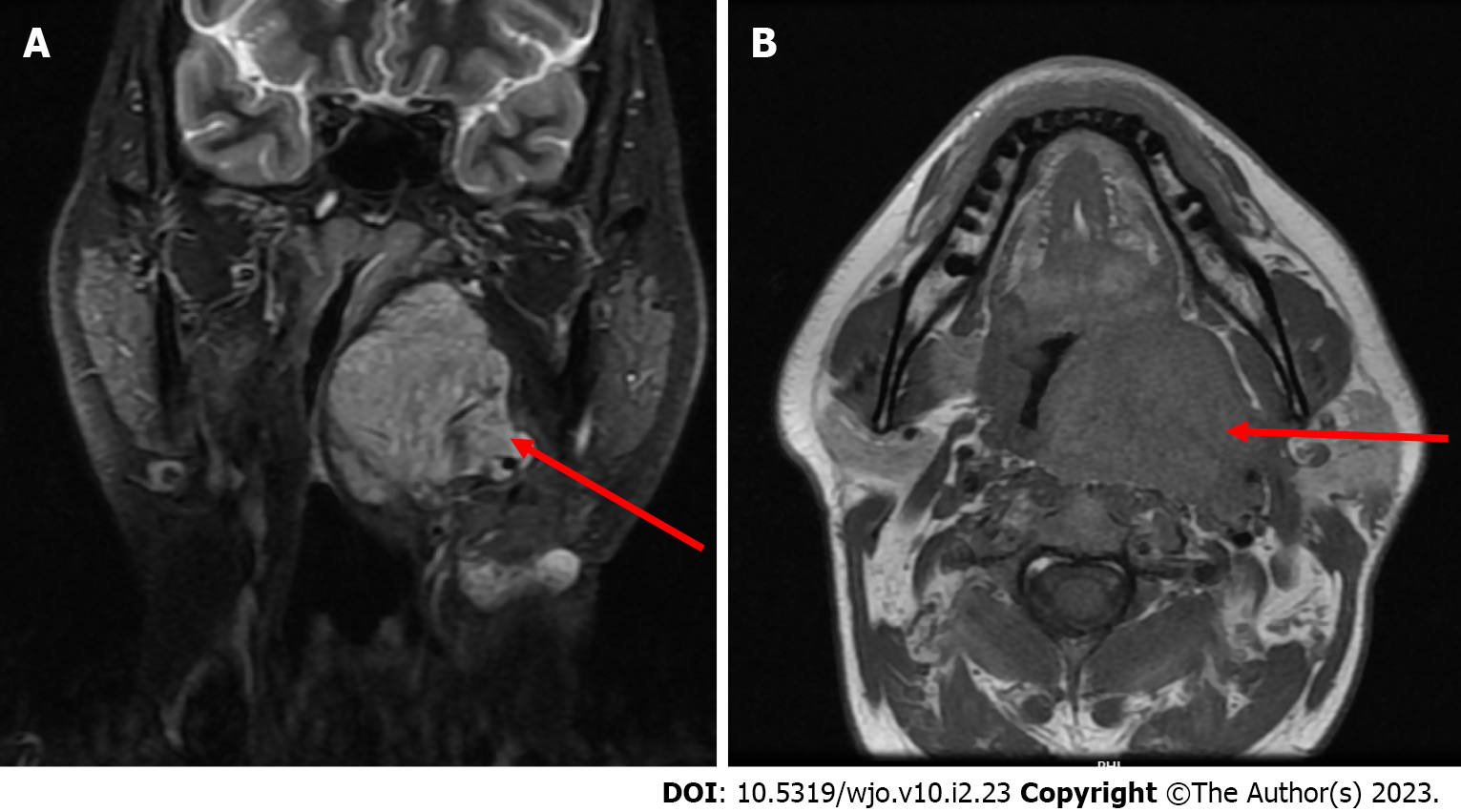
Fibreoptic laryngoscopy (FOL) showed a bulge in the region of the left lateral oropharyngeal wall with significant narrowing of the airway. MRI showed a 6 cm x 5 cm x 4 cm lobulated heterogeneous lesion involving the left lateral oropharyngeal wall, parapharyngeal space and peritonsillar area (Figure 1). The lesion compressed and displaced the left palatine tonsil anteroinferiorly, laterally reached the deep lobe of parotid gland, abuts medial pterygoid muscle anterolaterally and indents longus coli muscle posteriorly and compressed the external carotid artery. Postoperative changes were noted in the region of the left submandibular gland and anterior to the sternocleidomastoid muscle.
The main differential diagnosis was vascular malformation and lymphoreticular malformation. The final diagnosis was established after histopathological examination, after surgery.
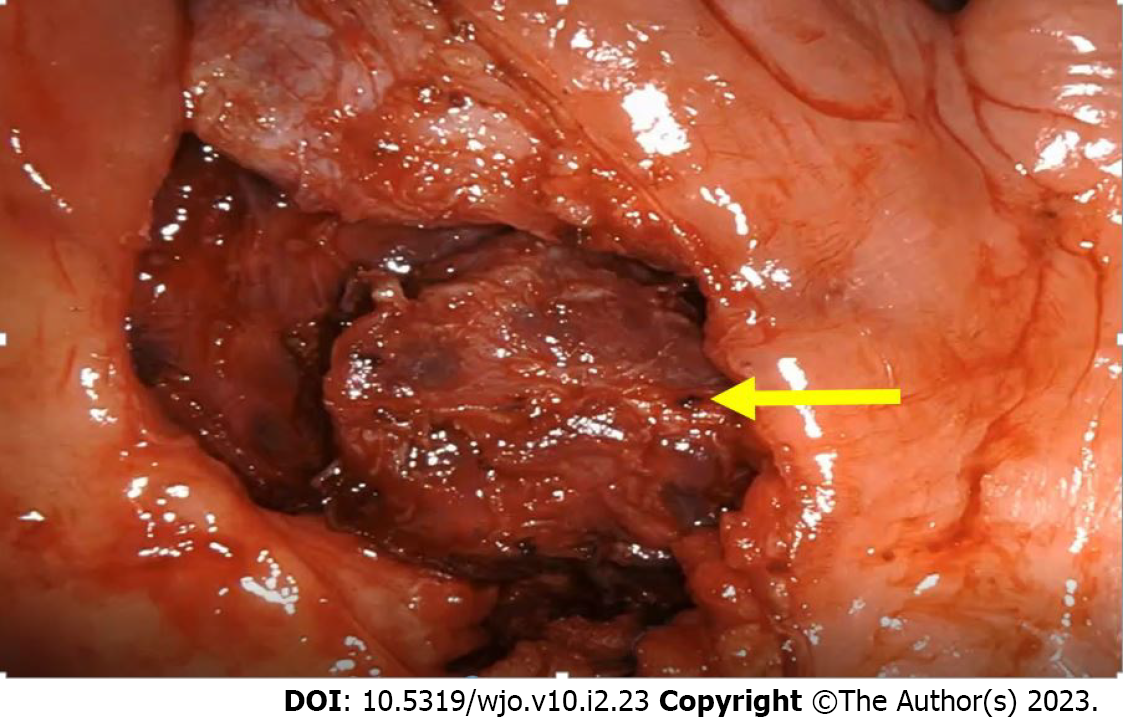
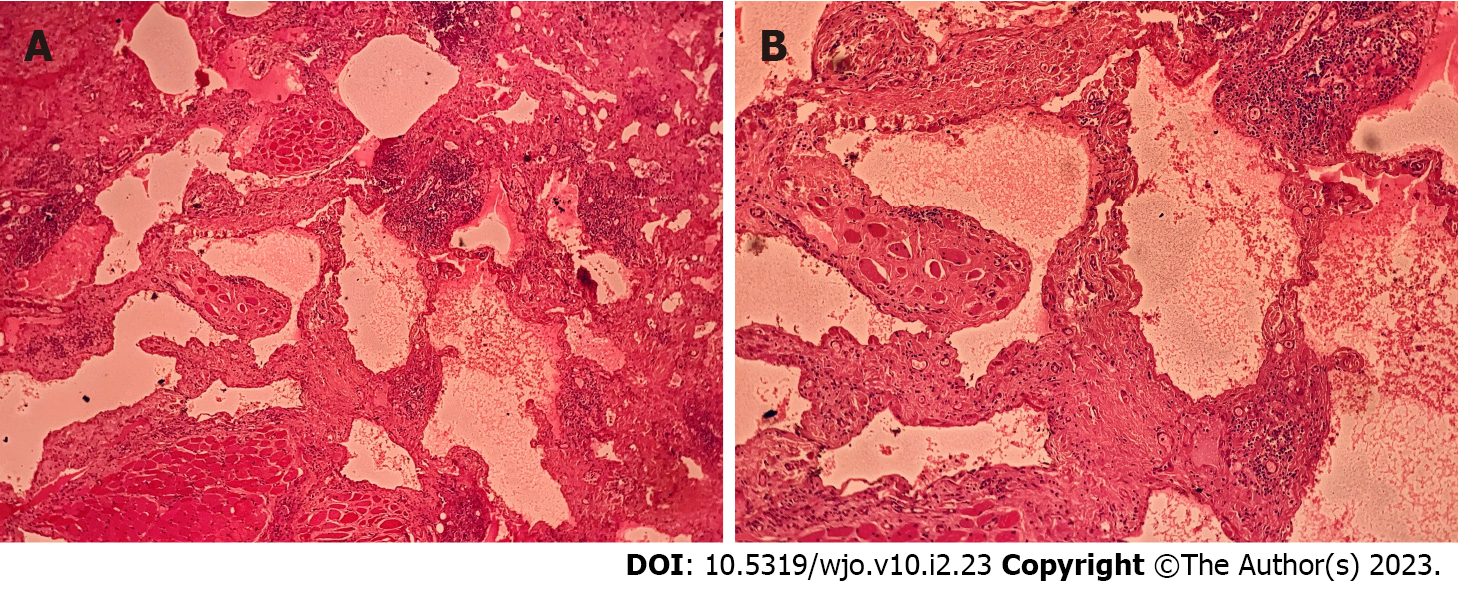
The patient was planned for upfront transoral robotic surgery (TORS) after obtaining anesthesia clearance. A written and informed consent was obtained from the patient before the procedure. The procedure was performed under general anesthesia. Feyh-Kastenbauer retractor was placed and da Vinci Xi robotic system was docked. Three arms of the robot were used for performing the surgery which contained the camera, bipolar and monopolar cautery. After making incision in the peritonsillar area, layer by layer dissection of the mucosa, submucosa and constrictor muscles with adequate hemostasis at each step was performed. A well encapsulated lesion was identified in the left parapharyngeal space which was excised (Figure 2) in toto and specimen was sent for histopathological examination. There were no intra- or peri-operative complications. The final histopathological report showed a multilobulated lesion with lymph containing sac and the diagnosis was lymphangioma (Figure 3).
Postoperatively, the patient stayed in the hospital for 3 days and was administered antibiotics and analgesics. For the initial 1 week, the patient was on Ryle’s tube feed. Postoperatively, the patient followed up at the outpatient department on day 7, and fibreoptic laryngoscopy (FOL) showed a healed wound. The patient’s speech and swallowing were evaluated. The speech of the patient was normal and his swallowing was also unimpaired. He was then started on liquids followed by soft diet. Normal diet was started on day 15 after surgery. The patient has been on regular follow-up since then for a period of 6 months and has no signs of residual disease, recurrence or any other post-operative complications.
Lymphangiomas are defined as benign, congenital and hamartomatous lesions which develop due to abnormalities in the lymphatic system. Their incidence was reported to be 1.2 -2.8 per 1000 new births [4]. First 5 years of life show the highest incidence of lymphangiomas (80%-90%)[7].
Histologically, lymphangiomas are classified as capillary, cavernous and cystic hygromas[8]. Based on size, it is divided into microcystic (< 2 cm) and macrocystic types (> 2 cm)[3]. Bhayya et al[9] classified them as lymphangioma simplex, cavernous lymphangioma, cystic lymphangioma and benign lymphangioendothelioma[9]. Based on anatomical location, in 1995, de Serres et al[10] proposed a classification system as follows: Class I, unilateral infrahyoid lesion; Class II, unilateral suprahyoid lesion; Class III, unilateral combined supra and infrahyoid lesion ; Class IV, bilateral suprahyoid lesion, and Class V, bilateral combined supra and infrahyoid lesion[10].
It is reported that 80% of lymphangiomas develop in the neck and 85% are unilateral[4]. Most common presentations include swelling in the neck, respiratory distress, difficulty in swallowing and pain secondary to infection or haemorrhage[7]. Although lymphangiomas are benign lesions with no malignant potential, occasionally it can enlarge to compress and invade the adjacent structures. The latter is a feature of poor prognosis in advanced cases[2]. Clinically, they usually appear as painless and cystic lumps, which are transilluminant in nature. They are associated with pain only when they are complicated with infection or haemorrhage[3].
Lymphangiomas are associated with various congenital syndromes which include trisomies of 13, 18, 21, Ullrich Turner syndrome, Noonan-Ehmke syndrome, aortic coarctation, hypoplastic left heart syndrome, Cantrell Haller Ravitsch syndrome, Apert syndrome, Brachmann-de Lange syndrome, foetal alcohol spectrum disorders, Fryns syndrome, Escobar syndrome, limb hypertrophy, fetal akinesia deformation sequence and hydrops[8].
Imaging is an important diagnostic modality to understand the exact origin, location and extent of lymphangioma. On ultrasound done during the antepartum period, lymphangiomas appear as thin walled multiloculated cysts. CT scan is better compared to USG for imaging lymphangiomas. In CT scans, they appear as low attenuation masses with regular margins and an enhancing rim on intravenous contrast. On T1 weighted images, they appear with low signal compared to muscles and on T2 weighted images, they appear hyperintense compared to fat[4,6].
In addition, 50% of parapharyngeal space tumors have a salivary cause, 20% have a neurogenic root, and 30% are benign and malignant lymphoreticular lesions, metastatic lesions, carotid body tumors and lipomas. Amongst neurogenic tumors, Schwannomas arising from the vagus nerve, presenting as post styloid compartment lesions are the most common[11]. On imaging, homogenous lesions seen displacing the internal carotid or common carotid artery anteriorly is suggestive of schwannoma arising from vagus nerve or sympathetic trunk[12]. Lipomas appear as hyperintense lesions on T1- and T2-weighted images with internal septations[13]. Vascular tumors are generally more conspicuous on T2-weighted images. Pleomorphic adenomas are usually characterized by the smooth and regular, non-infiltrating margins with cystic or necrotic areas[14]. Paragangliomas have a characteristic “salt and pepper” appearance on MRI scan[15]. Dermoid and epidermoid cysts are differentiated from other similar lesions as they often appear as unilocular masses with homogeneous hypoattenuating fluid on CT scan[16].
The selection criteria employed for treatment of lymphangiomas include large size, disfigurement, recurrent infections, dysphagia or respiratory distress. Literature shows spontaneous regression in 15% cases[8]. Surgery forms the mainstay of treatment[17]. Other treatment options include laser excision, radiotherapy, sclerosant injection, unroofing, aspiration or steroids[4].
The decision on choosing the type of approach for surgery depends on the site and nature of the lesion. Traditionally, the transcervical transmandibular approach was observed to give good exposure of the parapharyngeal space[3]. The main disadvantages of this approach include the dysphagia and persistent respiratory difficulties, which occur secondary to the post-operative mucosal edema and loss of pharyngeal innervation[7].
Traditionally, surgeons believed that in case of lesions extending to parapharyngeal space, complete surgical excision was difficult to obtain without damaging nervous and vascular structures and thus they used to resort to alternatives like drainage and sclerotherapy with different substances such as tetracycline, bleomycin and triamcinolone and radiofrequency ablation[18]. Complications and associated morbidity can include infections, tissue necrosis, cranial nerve lesions, vascular thrombosis and even endocrine disorders[19]. But now, with the advent of robotic surgery, these disadvantages have been overcome and it is possible to obtain 100% clearance of lesions in parapharyngeal space without injuring any neural or vascular structure[20].
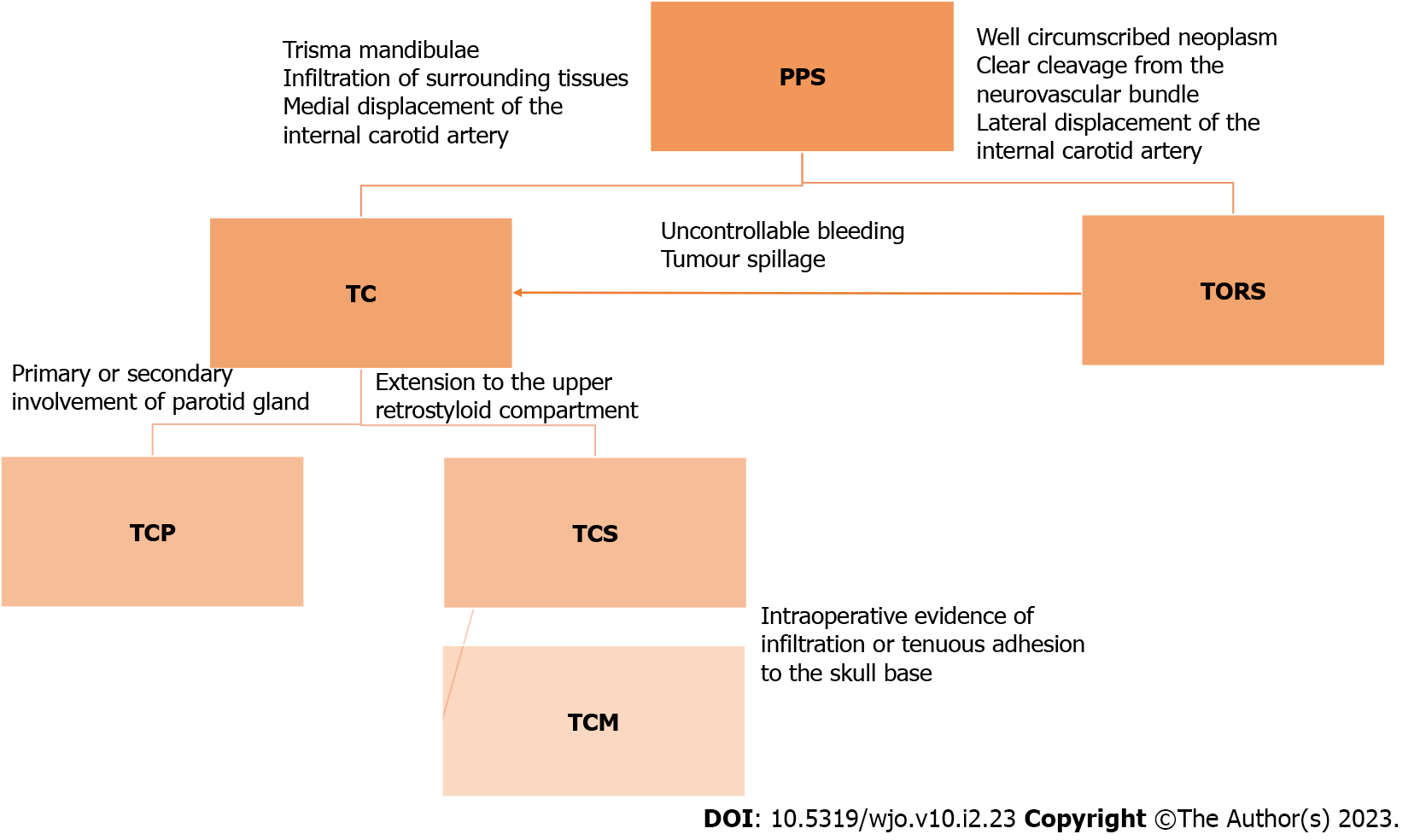
A surgical algorithm was proposed by Chu et al[21] in 2017 for access to parapharyngeal space (Figure 4).
TORS should be preferred for well circumscribed lesions in the pre- or post-styloid compartment[21] as suggested by Chu et al[21]. Transoral robotic surgery was opted in our case as it gives a magnified and high resolution view, along with motion scaling and tremor filtration which allows for delicate dissection around the tumor capsule. This approach is also less morbid compared to the other traditional approaches and reduces the chances of complications like swallowing problems, trismus, auriculotemporal syndrome, first bite syndrome, marginal mandibular and hypoglossal nerve palsy. Cosmesis achieved with this approach is also excellent compared to the transcervical approaches. The other advantages of using robotic surgery in this case include minimal blood loss, shorter hospital stay and early initiation of oral diet for the patient. Postoperatively our patient had no infections or wound dehiscence, and we were able to start orally by day 7.
Recurrence is usually noted in the first year following incomplete excision of lymphangiomas due to regeneration of the lymph vessels[22]. Besides completeness of excision, recurrence rate is based on the type and complexity of the mass. Simple lesions which are completely excised have 0% recurrence rate whereas complex lesions with partial excision have a recurrence rate of 10%–27 % and in those with complete excision, it is 50%–100%[4,7].
Lymphangiomas are benign hamartomatous lesions which rarely present in the parapharyngeal space. Large size, dysphagia, respiratory distress, pain due to recurrent infection and hemorrhage are the main indications warranting treatment. MRI is the ideal imaging modality. Transoral robotic surgery is one of the best approaches to parapharyngeal space lesions with favorable anatomy, with minimal morbidity and excellent clearance.
I would like to acknowledge contributions from the department of surgical oncology and robotic surgery, radiology and pathology of BLK- MAX Superspeciality hospital and thank them for the same.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He YF, China; Maurea S, Italy S-Editor: Liu GL L-Editor: Ma JY P-Editor: Liu GL
| 1. | Mehta MR. Cystic hygroma: Presentation of two casfes with a review of the literature. Indian J Otolaryngol Head Neck Surg. 2000;52:319-322. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Hartl DM, Roger G, Denoyelle F, Nicollas R, Triglia JM, Garabedian EN. Extensive lymphangioma presenting with upper airway obstruction. Arch Otolaryngol Head Neck Surg. 2000;126:1378-1382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 63] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Balineni P, C H VPK, Reddy E D, Reddy JS. Extensive parapharyngeal lymphangioma in a adult-Case report and review of literature. Int J Surg Case Rep. 2020;75:85-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Jaiswal AA, Garg AK, Ravindranath M, Sarkar J, Mohanty MK. ‘A huge congenital cervical lymphangioma’–case report with review of literature. Egyptian Journal of Ear, Nose, Throat and Allied Sciences. 2015;16:283-290. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Aneeshkumar MK, Kale S, Kabbani M, David VC. Cystic lymphangioma in adults: can trauma be the trigger? Eur Arch Otorhinolaryngol. 2005;262:335-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Romeo V, Maurea S, Guarino S, Sirignano C, Mainenti PP, Picardi M, Salvatore M. A case of lower-neck cystic lymphangioma: correlative US, CT and MR imaging findings. Quant Imaging Med Surg. 2013;3:224-227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 7. | Grasso DL, Pelizzo G, Zocconi E, Schleef J. Lymphangiomas of the head and neck in children. Acta Otorhinolaryngol Ital. 2008;28:17-20. [PubMed] [Cited in This Article: ] |
| 8. | Sharma JVP, Kazi FN. Cystic lymphangioma in adult-a rare case scenario or a misdiagnosis? J Surg Case Rep. 2021;2021:rjab062. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 9. | Bhayya H, Pavani D, Avinash Tejasvi ML, Geetha P. Oral lymphangioma: A rare case report. Contemp Clin Dent. 2015;6:584-587. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | de Serres LM, Sie KC, Richardson MA. Lymphatic malformations of the head and neck. A proposal for staging. Arch Otolaryngol Head Neck Surg. 1995;121:577-582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 172] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Giraddi G, Vanaki SS, Puranik RS. Schwannoma of parapharyngeal space. J Maxillofac Oral Surg. 2010;9:182-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Atkinson JC, Gaze MN, Wilson JA. Benign neck disease. In: Stell and Maran’s head and neck surgery. Oxford, Butterworth Heinemenn 2000; 4: 193-194. [Cited in This Article: ] |
| 13. | Lee HSH, Ngai CM. Parapharyngeal space lipoma: a case report. Hong Kong Med J. 2020;26:438-440. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 14. | Jain SN, Kumar A, Dhongade HS, Varma R, Hathiram B, Khattar V. Imaging of parapharyngeal space and infratemporal fossa. Int J Otorhinolaryngol Clin. 2012;4:113-121. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Riffat F, Dwivedi RC, Palme C, Fish B, Jani P. A systematic review of 1143 parapharyngeal space tumors reported over 20 years. Oral Oncol. 2014;50:421-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 129] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 16. | Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics. 1999;19:121-46; quiz 152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 257] [Cited by in F6Publishing: 266] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 17. | Wang J, Yang Y, Guo J, Yao Y, Dong L, Mou Y, Zhang Y, Song X. Cervical lymphangioma in adults: A report of seven cases and review of the literature. Laryngoscope Investig Otolaryngol. 2022;7:751-756. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 18. | Colbert SD, Seager L, Haider F, Evans BT, Anand R, Brennan PA. Lymphatic malformations of the head and neck-current concepts in management. Br J Oral Maxillofac Surg. 2013;51:98-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Gowa L, Rampat R, Khanb A, Mihaimeed F. Adult-onset cystic hygroma: a case report and review of management. Grand Rounds. 2011;11:5-11. [DOI] [Cited in This Article: ] |
| 20. | Chan JY, Tsang RK, Eisele DW, Richmon JD. Transoral robotic surgery of the parapharyngeal space: a case series and systematic review. Head Neck. 2015;37:293-298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | Chu F, Tagliabue M, Giugliano G, Calabrese L, Preda L, Ansarin M. From transmandibular to transoral robotic approach for parapharyngeal space tumors. Am J Otolaryngol. 2017;38:375-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Jakubikova J. Retropharyngeal lymphangioma. Bratisl Lek Listy. 2006;107:439-441. [PubMed] [Cited in This Article: ] |