Published online Aug 12, 2014. doi: 10.5318/wjo.v4.i3.63
Revised: June 19, 2014
Accepted: June 27, 2014
Published online: August 12, 2014
Processing time: 222 Days and 12.7 Hours
Orthokeratology is a reversible technique that temporarily changes the curvature of the cornea with the aim of addressing refractive errors. The United States Food and Drug Administration (FDA) granted approval for using reverse geometry contact lenses to correct myopia without any age restriction. Information from the pre-market applications to the FDA was rated as level II evidence. Another unapproved use of overnight orthokeratology is for the prevention of myopic progression. Although orthokeratology is advocated to reduce myopic progression, there are limited long-term studies with substantial evidence of its benefits. Much of this evidence comes from non-robust experimental studies using historical or self-selected controls with relative high dropout rates. Although some positive results have been published in temporarily reducing the myopic refractive error and its progression, the use of these lenses can be associated with serious complications such as microbial keratitis. Microbial keratitis is a potentially vision-threatening adverse response associated with contact lens wear. In fact, contact lens wear has been shown to be the predominant risk factor of microbial keratitis in some developed countries. Most of the published cases on overnight orthokeratology related microbial keratitis occurred in children or adolescents. Parents considering orthokeratology must make an informed decision about its temporary benefit and its potential for permanent loss of vision. The ophthalmic community should be reminded of the potential complications of orthokeratology.
Core tip: Orthokeratology uses specially designed rigid contact lenses to temporarily reshape the cornea to ameliorate refractive errors and it has also been suggested to slow the progression of myopia. None of the published studies to date in assessing its efficacy are rated as level I evidence. Orthokeratology carries the risk of microbial keratitis, which is potentially sight threatening and the safety of orthokeratology remains difficult to assess. Practitioners prescribing orthokeratology must receive appropriate training with respect to the local standards, inform patients and/or their parents of the potential risks, and ensure their patients’ compliance in proper handling of the day to day care of their lenses to minimize the infective risks.
- Citation: Wan KHN, Jhanji V, Young AL. Orthokeratology lens related infections. World J Ophthalmol 2014; 4(3): 63-70
- URL: https://www.wjgnet.com/2218-6239/full/v4/i3/63.htm
- DOI: https://dx.doi.org/10.5318/wjo.v4.i3.63
Orthokeratology is defined as the reduction, modification, or elimination of refractive anomalies by the programmed application of contact lenses[1]. Modern day orthokeratology was first advocated during the Second World Contact Lens Congress in Chicago in 1962, where George Jessen, the father of orthokeratology, introduced fitted polymethyl methacrylate (PMMA) contact lenses which had a curve flatter than the cornea to alter the curvature of the cornea and reduce myopia[1]. These lenses were worn during daytime and provided clear uncorrected vision for a few hours after they were removed in the afternoon. Over the next few decades, few other studies comparing daily wear of orthokeratology lenses reported similar modest but not significantly different myopic reduction as compared with conventional alignment fitted lens. Disappointment began to set in as inducible corneal astigmatism was reported due to lens instability. Variable and temporary refractive outcomes were observed, requiring continuous use of retainer lens to maintain its refractive effectiveness and/stabilisation.
Re-emergence of interest in this technique came in the late 1980’s with the development of rigid gas permeable (RGP) lens that has a significantly higher oxygen transmission (Dk). Such material allows for a relatively safer closed-eye contact lens usage[2]. This led to the concept of overnight orthokeratology (OOK) where lenses are worn during the night time and removed during the daytime, allowing unaided vision during waking hours. Computer-assisted corneal topographic mapping also provided more detailed assessment of the elevation and curvature of the cornea, allowing more accurate lens design and fitting. Conventional rigid lens surfaces are designed to have a central base surrounded with progressively flattening concentric curves. With the development of reverse geometry lenses, designed to have a flat-back central optical zone with steeper intermediate zone, more accelerated flattening of the central corneal zone is possible compared to the previous lens designs[3].
This review will highlight the published literature on the efficacy of orthokeratology and the evidence of potential limitations, and outline the complications related to the use of these lenses.
Orthokeratology temporarily reduces the overall refractive power by flattening the central cornea to reduce the corneal sagittal height in order to reduce myopia[4]. The corneal periphery becomes relatively thicker, enhancing the peripheral corneal curvature. There is conflicting evidence about the time sequences of these events, but the combined effect is proposed to be the mechanism behind the refractive changes[5]. Thinning of central epithelium has been observed with optical coherence tomography[6]. Correlating with the morphological changes, unaided vision usually improves on an average by 1 wk, and stabilizes by 1 mo[7]. However, such visual improvement is transient, unless retainer lenses are continuously used at night time to maintain the flattened central cornea, where the frequency of use would depend on the degree of myopia, and ranges from every 1-2 nights to maintain the flattening effect[7]. The US Food and Drug Administration (FDA) approved the Paragon Corneal Refractive Therapy (CRT) for myopia reduction in 2002 based on their premarket study consisting of 205 subjects, only 24 of whom were between the age of 12 and 18 years[8]. During the evaluation, the FDA advisory panel commented that they would only recommend the approval of Paragon CRT be limited to patients 18 years and older, but FDA granted the approval of OOK without any age restriction. Later in 2004, Euclid Systems also received FDA approval for their orthokeratology to control myopia.
An unapproved use of OOK is for prevention of myopic progression. It is proposed that OOK prevents myopia progression via“peripheral hyperopic defocus”[9]. This theory suggests that the peripherally flatter cornea reduces peripheral hyperopia by aligning the image shell onto the mid peripheral retina, signalling the peripheral retina to control axial elongation. This controversial theory was tested in studies and it was found that relative peripheral hyperopia exerts little consistent influence on the rate of myopia progression or axial elongation[10]. The reported reduction in axial length also may be attributed to the gradual slowing of myopic progression in the control group with age, which may be expected. The published studies so far were neither randomized nor prospective, leading to observer bias. Five studies using historical or self-selected controls reported relative slower myopic progression (by 32%-55%) in low-to-moderately myopic children wearing OK lenses compared with those wearing conventional eyeglasses[11-14] or single-vision soft contact lenses[15]. The dropout rate reported in these studies with orthokeratology varies from 6%[14] to 30%[15]. The Longitudinal Orthokeratology Research in Children trial studied 35 children in Hong Kong who wore OK lenses for 2 years[11]. The authors found that the axial length in the orthokeratology group increased by 0.29 mm vs 0.54 mm for the control group. However, a major drawback in this study was that a historical control group of children wearing single vision lenses was used as the control. The Corneal Reshaping and Yearly Observation of Near-sightedness Pilot Study[15] compared 28 participants using corneal reshaping contact lenses to a historical control subject who were randomly assigned to wear soft contact lenses during the Contact Lens and Myopia Progression study[16]. Although the authors reported the annual rate of change in axial length was 0.16 mm per year less for corneal reshaping lens wearers than soft contact lens wearers (P = 0.00004), the low number of participants, the choice of control, as well as a 30% dropout rate limit the strength of the conclusions drawn from this study. Another study followed the OOK participants over 5 years and reported that changes in axial length over each year were significantly different; however, by the end of year 5, the changes in axial length were no longer significantly different (P = 0.8633)[13]. A recently published randomized controlled trial attempted to determine whether OK was effective in slowing myopia progression[17]. They found that subjects wearing OOK lenses had a slower axial elongation by 43% compared with those wearing single-vision glasses. Younger children less than 7 years of age had faster axial elongation and may have additional benefit from early OK treatment. However, the examiners measuring the axial length were not masked and a dropout rate of 27% was reported in the orthokeratology group. In addition, although the OK group had a reduction in axial length over the study 2-year period, corresponding changes in refraction were not reported and the clinical significance of an isolated reduction in axial elongation without refractive changes is not known.
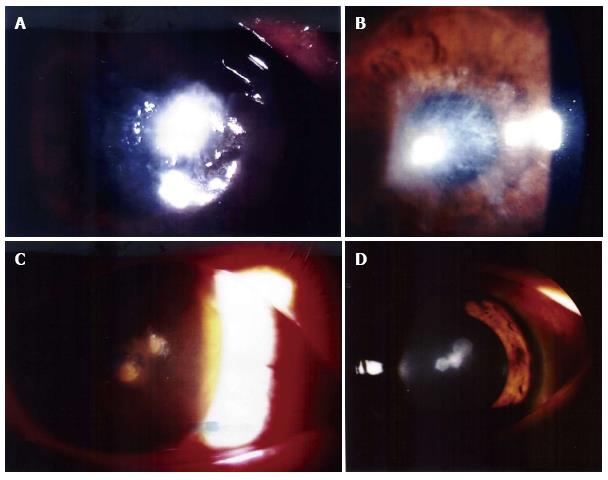
A review by Watt and Swabrick analysed all cases of microbial keratitis (MK) associated with OOK since 2001 to 2007[18]. Not surprisingly, most of the findings remain unchanged from the initial analysis of the first 50 cases[19]. Microbial keratitis raised significant concerns in using OOK lenses. The majority of these infections were central and severe. Two of our own examples can be seen in Figure 1. The final best-corrected visual acuity (BCVA) after resolution of infection was reported in 93 cases, 18% of which had BCVA less than 20/200. Most cases occurred in children or adolescents: 55% of the cases were between 8-15 years old, 41% were between 16-25 years old, and the remaining 4% were above 25 years of age. There is particular concern with OOK in children and young adults since this is the age group with the highest number of users[20]. It would be ideal to stratify the OOK users by age cohorts and analyse the outcomes in terms of initial and final BCVA in order to identify risk factors associated within each cohort, and subsequently with strategies to reduce risk of MK. However, based on the information available related to lens design, material or fitting, lens care and compliance, it was difficult to draw conclusions about risk factors with regards to the specific cohorts by age group. In this review, Pseudomonas aeruginosa infection accounted for 37% of the cases while Acanthamoeba infection was responsible for 33%. Acanthamoeba infection is capable of causing corneal scarring, ultimately leading to a significant vision loss. Acanthamoeba infections are known to be associated with contaminated water sources, which further raise the worry regarding the care of OK lenses. Thus it is crucial not to use any tap water during the cleansing of lenses. The prevalence of Acanthamoeba related MK is only reported to be 3%-5% in case series for other contact lens wearing modalities. The much higher prevalence of Acanthamoeba infection in OOK remains a cause of concern[21,22]. Tear film immunoglobulin A level is found to be reduced in children and may contribute to increased risk of Acanthamoeba keratitis in this age group[23]. No significant differences were reported in the ocular flora profile over time in patients with multiple conjunctival cultures before and during OOK use[24]. It is likely the OOK related MK is related to opportunistic pathogens already present on the corneal surface infecting the underlying compromised corneal epithelial, which resulted from the physical reshaping of the cornea and hypoxic stress from nocturnal wear. Apart from thinning of the cornea, OOK also changes the structural integrity of the epithelium, where the central epithelium significantly differs in cell shape and size. The deeper layers of the cornea may also lose their normal plicae[25,26]. Even with the most oxygen permeable lenses, animal studies found significant Pseudomonas adhesions to the cornea with the use of reverse geometry contact lens compared with alignment fit lenses. The enhanced binding is accompanied by thinning and reduced turnover of the epithelium. All these factors may attribute to the increased susceptibility of microbial invasion to the cornea[27]. Clinical trials in human subjects with alignment fit RGP lenses using the highest Dk material did not report an increase in Pseudomonas binding after 30 nights of usage[28]. This suggests that the reverse-geometry lens architecture may produce risk of Pseudomonas induced MK. The compressive forces of the reverse geometry lenses may lead to disrupted epithelial surfaces, and the reverse geometry lenses may provide a reservoir for bacteria deposition, which is further aggravated by a compromised ocular surface from overnight wear[29,30]. Pseudomonas infection is also associated with OOK related corneal ulcer in children. In an observational case series with children, 83% of cases were culture positive for P. aeruginosa. Although these ulcers were neither central nor paracentral, all patients suffered a loss in their BCVA with respect to the location of the corneal scar[31]. East Asian ethnicity comprised roughly 95% of the disease population in a review on microbial keratitis associated with OOK[18]. The reported demographic profile could either reflect ethnical susceptibility (as a high proportion of East Asian children are myopic) or could just reflect the demographic profile of the worldwide OK lens wearing population since the usage in more affluent economies[32]. The estimated myopia in urban Chinese children at the age of 18 years would be up to 2.0 dioptres higher than their parents, and their refractive errors at the age of 11 would already be similar to their parents. This suggests a strong environmental effect on myopia development as evident by this remarkable single-generation myopic shift. In addition, the genetic risk factors, and the environmental and lifestyle factors present in the Chinese population may lead to a lower threshold for the Chinese parents to allow their children to wear OK lens[33]. Lin et al[34] reported that there is a greater increase in epithelial permeability following overnight contact lens wear in Asian as compared to Caucasian subjects, which could lead to a more easily compromised epithelial barrier, however the rates of MK were not reported to be significantly different from the rest of the world[21]. Further research is warranted to answer whether there is ethnical difference in MK susceptibility.
The cases of microbial keratitis associated with orthokeratology were largely documented by the review published in 2007[18]. Since then, we identified another 12 cases via our literature search in PubMed[35-39]. Table 1 summarizes the features from the 34 published reports on orthokeratology related microbial keratitis cases up to March 2014[29,31,35-66]. Despite reported case series on MK with OOK, these do not help to determine the true incidence or the relative risks compared with other contact lens modalities. The number of cases reported in the literature likely represents an underestimation, as the values of publications on the same topic become relatively less once a few cases have already been reported in the literature, thus further publication on the same topic is less likely to be accepted by the respective journals, and the incentive for authors to prepare a manuscript also lessens. Without a good estimation of the denominator and numerator, it would be difficult to comment on the absolute risk of microbial keratitis associated with orthokeratology.
| Ref. | Year of publication | Country of origin | Number of cases | Microbiology |
| Chen et al[40] | 2001 | Taiwan | 1 | Serratia marcescens |
| Lü et al[41] | 2001 | China | 16 | 7 = P. aeruginosa; 8 = Acanthamoeba; 1 = fungus |
| Chen et al[42] | 2002 | Taiwan | 1 | Pseudomonas putida |
| Hutchinson et al[43] | 2002 | Australia | 2 | 1 = P. aeruginosa; 1 = Acanthamoeba, P. aeruginosa and Burkholderia cepacia |
| Keddie et al[44] | 2002 | Canada | 2 | Acanthamoeba |
| Lin et al[45] | 2002 | China | 1 | Nocardia sp. |
| Lau et al[46] | 2003 | Taiwan | 2 | P. aeruginosa |
| Poole et al[47] | 2003 | United Kingdom | 1 | Not identified |
| Wang et al[48] | 2003 | Singapore | 1 | P. aeruginosa |
| Xugang et al[49] | 2003 | China | 4 | Acanthamoeba |
| Young et al[29] | 2003 | Hong Kong | 1 | P. aeruginosa |
| Hsiao et al[50] | 2004 | Taiwan | 7 | 6 = P. aeruginosa; 1 = Not identified |
| Lang et al[51] | 2004 | United States | 2 | 1 = P. aeruginosa; 1 = Not identified |
| Van Der Worp et al[52] | 2004 | Netherlands | 1 | P. aeruginosa |
| Young et al[31] | 2004 | Hong Kong | 6 | 5 = P. aeruginosa; 1 = Not identified |
| Araki-Sasaki et al[53] | 2005 | Japan | 1 | P. aeruginosa |
| Macsai et al[54] | 2005 | United States | 2 | 1 = P. aeruginosa; 1 = H. influenza |
| Hsiao et al[55] | 2005 | Taiwan | 21 | 9 = P. aeruginosa; 2 = coagulase-negative Staphylococcus sp.; 1 = Serratia marcescens; 1 = Acanthamoeba |
| Tseng et al[56] | 2005 | Taiwan | 10 | 2 = Acanthamoeba; 1 = P. aeruginosa; 1 = non fermentative Gram negative bacilli; 6 = Not identified |
| Wilhelmus et al[57] | 2005 | United States | 1 | Acanthamoeba |
| Yepes et al[58] | 2005 | Canada | 3 | 1 = P. aeruginosa; 1 = Serratia marcescens; 1 = Acanthamoeba |
| Lee et al[59] | 2006 | South Korea | 1 | Acanthamoeba |
| Priel et al[60] | 2006 | Israel | 1 | P. aeruginosa |
| Sun et al[61] | 2006 | China | 28 | 8 = P. aeruginosa; 13 = Acanthamoeba; 1 = Nocardia sp.; 1 = Providencia stuartii; 2 = fungus; 1 = Gram negative rods; 2 = Not identified |
| Voyatzis et al[62] | 2006 | United Kingdom | 1 | P. aeruginosa |
| Ying-Cheng et al[63] | 2006 | Taiwan | 1 | Burkholderia cepacia, Pseudomonas putida, and P. aeruginosa |
| Lee et al[64] | 2007 | South Korea | 4 | 1 = Acanthamoeba; 1 = Acanthamoeba and trophozoites; 2 = Not identified |
| Robertson et al[65] | 2007 | United States | 1 | Acanthamoeba |
| Watt et al[66] | 2007 | Australia | 9 | 4 = P. aeruginosa; 2 = Acanthamoeba; 3 = Not identified |
| Kim et al[37] | 2009 | South Korea | 1 | Acanthamoeba (bilateral) |
| Shehadeh-Masha'ou et al[38] | 2009 | Israel | 4 | P. aeruginosa |
| Arance-Gil et al[35] | 2013 | Spain | 1 | Acanthamoeba |
| Greenwell et al[36] | 2013 | Australia | 2 | Acanthamoeba |
| Tran et al[39] | 2014 | Australia | 4 | 1 = Acanthamoeba; 1 = P. aeruginosa; 2 = Not identified |
Assessment of the risks and adverse effects is limited, as none of the published articles on OOK are level I evidence. Furthermore, the issue on safety could not truly be concluded from the small number of subjects in studies. Adverse effects are often under-reported or inconsistently documented, due to poor indexing, making it more difficult to look up published literature on safety of treatment[67]. The details of reported cases vary in lens type, lens wearing regime, type of lens and compliance to cleansing regime. Despite the credentialing and training programs offered for OOK practices, a learning curve would exist. The interpretation of fluorescein patterns requires skill and experience; the central flat zone of a reverse-geometry contact lens is more discernible to experienced practitioners. Safety about usage and prescription of OOK raises scrutiny. The FDA requires OOK practitioners to be certified to a minimal standard of orthokeratology education and granted the OOK approval without age restriction on the basis that no additional safety concerns are specific to adolescents as long as OOK is fitted by trained personnel and used accordingly[68]. Manufacturers of OOK lenses launched online training program, which consists of certificate course and tests that can be completed in a short period of time. Whether such training program is adequate in providing proper knowledge and skills in the practice of orthokeratology warrants further investigations.
Contact lens use remains the commonest risk factor for microbial keratitis in the paediatric population and orthokeratology is one of the leading causes of contact lens related infection in East Asia[69]. Although many of the cases published have reported data from children, it does not necessary mean that children are at a greater risk of developing MK. Given the potential theoretical benefit in reducing myopia progression, there may be more children using OOK than adults[11]. Due to the larger number of cumulative years that a child may be exposed to potential risks, complications in children may be reported more frequently than adults. The FDA approval for overnight orthokeratology was based on the premarket study cohort where adolescents aged 12-17 years old comprised 11% of the study sample. In fact, orthokeratology fits represent 28% of all contact lenses prescribed to minors[70]. The FDA issued Section 522 in 2006, requiring manufacturers to conduct post-market surveillance to address “the relative risk of developing MK in persons under the age of 18 as compared to adults in patients undergoing overnight OK treatment”. This question was addressed in a retrospective study using a practitioner survey of 1317 OOK patients (51% children)[20]. They found 8 cases of corneal infiltrates associated with a painful red eye (six in children and two in adults). Two were classified as MK and occurred in children, but neither resulted in a loss of visual acuity. The overall estimated incidence of MK is 7.7 per 10000 years of wear (95%CI: 0.9-27.8). For children, the estimated incidence of MK is 13.9 per 10000 patient-years (95%CI: 1.7-50.4). While for adults, the estimated incidence of MK is 0 per 10000 patient-years (95%CI: 0-31.7). This is the largest study to quantify the risk of MK associated with OOK with 2599 patient-years of wears and worthy to note the difference between children and adult rates. Based on the incidence estimated in this study, the two FDA pre-market approval studies[8,71] and another retrospective study of 296 patients by Lipson et al[72] did not report any cases of MK. Although the confidence intervals between the adult and children groups overlap, it should not be interpreted as no difference in incidence among the 2 groups as true differences less than 50 cases per 10000 patient-years were beyond the power of that study[20].
Although exact incidence of MK associated with OK lenses is not known, it has the potential to compromise vision. Degree of damage (i.e., reduction in visual acuity) is only one aspect of risk evaluation. In order to maintain the control in myopia, patients have to continue indefinite application of OK lenses overnight. Despite using high oxygen permeable lenses, this will still put the patient at risk of MK, as the reduction of myopia is only temporary without regular overnight application. Comparing OOK with other myopia corrective devices, such as daytime contact lens wear, the risk of infectious keratitis is higher in overnight contact lens wear[73], and there is minimal risk in using spectacle wear. Comparing OOK with LASIK is inappropriate as the latter is an invasive procedure which is not FDA approved for children.
The therapeutic value of overnight orthokeratology remains unclear and many questions remain unanswered, such as the optimal treatment age and duration. Practitioners and end-users of OOK should work together to minimize the risk of MK by reinforcing compliance to proper cleansing techniques and minimizing exposure to contaminated water. OOK users should discontinue lens wear if they feel any pain and seek medical attention immediately. Practitioners must be competent in the prescription of OK lenses through accredited certification courses from appropriate statutory bodies. Better-designed prospective randomized clinical studies are needed to demonstrate the benefit of orthokeratology in reducing myopic progression and to adequately assess their safety, along with the contemporaneous reporting of adverse events. The reported dropout rates of more than 20% in the previous trials also raise concerns regarding tolerability and satisfaction in using OOK. Long-term follow-ups are needed as visual loss related to MK were only encountered in many patients who wore hard contact lens for more than 2 years. The genuine risk of severe MK associated with poor long-term visual outcomes in children needs to be highlighted to parents considering orthokeratology in an effort to avoid preventable visual loss.
P- Reviewer: Mimura T, Razeghinejad MR, Shih YF S- Editor: Song XX L- Editor: Wang TQ E- Editor: Lu YJ
| 1. | Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006;89:124-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 182] [Cited by in F6Publishing: 181] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 3. | MacKeen DL, Sachdev M, Ballou V, Cavanagh HD. A prospective multicenter clinical trial to assess safety and efficacy of Menicon SF-P RGP lenses for extended wear. CLAO J. 1992;18:183-186. [PubMed] [Cited in This Article: ] |
| 4. | Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002;85:284-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 45] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 5. | Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci. 2003;44:2518-2523. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 205] [Cited by in F6Publishing: 197] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 6. | Zhong X, Chen X, Xie RZ, Yang J, Li S, Yang X, Gong X. Differences between overnight and long-term wear of orthokeratology contact lenses in corneal contour, thickness, and cell density. Cornea. 2009;28:271-279. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Wang J, Fonn D, Simpson TL, Sorbara L, Kort R, Jones L. Topographical thickness of the epithelium and total cornea after overnight wear of reverse-geometry rigid contact lenses for myopia reduction. Invest Ophthalmol Vis Sci. 2003;44:4742-4746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | US Food and Drug Administration Center for Devices and Radiological Health, Paragon Vision Sciences. Summary of safety and effectiveness data from premarket approval application supplement number P870024/S43. Cited: 2014-03-03. Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf/P870024S043b.pdf. [Cited in This Article: ] |
| 9. | Smith EL. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029-1044. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 159] [Cited by in F6Publishing: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | Mutti DO, Sinnott LT, Mitchell GL, Jones-Jordan LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest Ophthalmol Vis Sci. 2011;52:199-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 11. | Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 343] [Cited by in F6Publishing: 382] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 12. | Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52:2170-2174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 239] [Cited by in F6Publishing: 262] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 13. | Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913-3919. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 243] [Cited by in F6Publishing: 288] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 14. | Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060-5065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 192] [Cited by in F6Publishing: 213] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 15. | Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181-1185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 252] [Cited by in F6Publishing: 280] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 16. | Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomized trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004;122:1760-1766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 107] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077-7085. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 362] [Cited by in F6Publishing: 486] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 18. | Watt KG, Swarbrick HA. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens. 2007;33:373-377; discussion 382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Watt K, Swarbrick HA. Microbial keratitis in overnight orthokeratology: review of the first 50 cases. Eye Contact Lens. 2005;31:201-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90:937-944. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 21. | Lam DS, Houang E, Fan DS, Lyon D, Seal D, Wong E. Incidence and risk factors for microbial keratitis in Hong Kong: comparison with Europe and North America. Eye (Lond). 2002;16:608-618. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 219] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 22. | Cheng KH, Leung SL, Hoekman HW, Beekhuis WH, Mulder PG, Geerards AJ, Kijlstra A. Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet. 1999;354:181-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 402] [Cited by in F6Publishing: 392] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 23. | Alizadeh H, Apte S, El-Agha MS, Li L, Hurt M, Howard K, Cavanagh HD, McCulley JP, Niederkorn JY. Tear IgA and serum IgG antibodies against Acanthamoeba in patients with Acanthamoeba keratitis. Cornea. 2001;20:622-627. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Boost MV, Cho P. Microbial flora of tears of orthokeratology patients, and microbial contamination of contact lenses and contact lens accessories. Optom Vis Sci. 2005;82:451-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Cheah PS, Norhani M, Bariah MA, Myint M, Lye MS, Azian AL. Histomorphometric profile of the corneal response to short-term reverse-geometry orthokeratology lens wear in primate corneas: a pilot study. Cornea. 2008;27:461-470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Nieto-Bona A, González-Mesa A, Nieto-Bona MP, Villa-Collar C, Lorente-Velázquez A. Short-term effects of overnight orthokeratology on corneal cell morphology and corneal thickness. Cornea. 2011;30:646-654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 27. | Ladage PM, Yamamoto N, Robertson DM, Jester JV, Petroll WM, Cavanagh HD. Pseudomonas aeruginosa corneal binding after 24-hour orthokeratology lens wear. Eye Contact Lens. 2004;30:173-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Ren DH, Yamamoto K, Ladage PM, Molai M, Li L, Petroll WM, Jester JV, Cavanagh HD. Adaptive effects of 30-night wear of hyper-O(2) transmissible contact lenses on bacterial binding and corneal epithelium: a 1-year clinical trial. Ophthalmology. 2002;109:27-39; discussion 39-40. [PubMed] [Cited in This Article: ] |
| 29. | Young AL, Leung AT, Cheung EY, Cheng LL, Wong AK, Lam DS. Orthokeratology lens-related Pseudomonas aeruginosa infectious keratitis. Cornea. 2003;22:265-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Choo JD, Holden BA, Papas EB, Willcox MD. Adhesion of Pseudomonas aeruginosa to orthokeratology and alignment lenses. Optom Vis Sci. 2009;86:93-97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Young AL, Leung AT, Cheng LL, Law RW, Wong AK, Lam DS. Orthokeratology lens-related corneal ulcers in children: a case series. Ophthalmology. 2004;111:590-595. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Cho P, Cheung SW, Edwards MH, Fung J. An assessment of consecutively presenting orthokeratology patients in a Hong Kong based private practice. Clin Exp Optom. 2003;86:331-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 33. | Liang YB, Lin Z, Vasudevan B, Jhanji V, Young A, Gao TY, Rong SS, Wang NL, Ciuffreda KJ. Generational difference of refractive error in the baseline study of the Beijing Myopia Progression Study. Br J Ophthalmol. 2013;97:765-769. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 34. | Lin MC, Graham AD, Fusaro RE, Polse KA. Impact of rigid gas-permeable contact lens extended wear on corneal epithelial barrier function. Invest Ophthalmol Vis Sci. 2002;43:1019-1024. [PubMed] [Cited in This Article: ] |
| 35. | Arance-Gil Á, Gutiérrez-Ortega ÁR, Villa-Collar C, Nieto-Bona A, Lopes-Ferreira D, González-Méijome JM. Corneal cross-linking for Acanthamoeba keratitis in an orthokeratology patient after swimming in contaminated water. Cont Lens Anterior Eye. 2014;37:224-227. [PubMed] [Cited in This Article: ] |
| 36. | Greenwell TH, Loh RS, Chehade M, Mills RA. Misdiagnosis of orthokeratology-related Acanthamoeba keratitis as herpes simplex virus keratitis. Clin Experiment Ophthalmol. 2013;41:418-420. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Kim EC, Kim MS. Bilateral acanthamoeba keratitis after orthokeratology. Cornea. 2009;28:348-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Shehadeh-Masha'our R, Segev F, Barequet IS, Ton Y, Garzozi HJ. Orthokeratology associated microbial keratitis. Eur J Ophthalmol. 2009;19:133-136. [PubMed] [Cited in This Article: ] |
| 39. | Tran T, Samarawickrama C, Petsoglou C, Watson S. Recent cluster of childhood microbial keratitis due to orthokeratology. Clin Experiment Ophthalmol. 2014;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Chen KH, Kuang TM, Hsu WM. Serratia Marcescens corneal ulcer as a complication of orthokeratology. Am J Ophthalmol. 2001;132:257-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 49] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Lü L, Zou L, Wang R. [Orthokeratology induced infective corneal ulcer]. Zhonghua Yan Ke Za Zhi. 2001;37:443-446. [PubMed] [Cited in This Article: ] |
| 42. | Chen K, Hsu W, Li S. Corneal ulcers as a complication of orthokeratology. Clin Exp Ophthalmol. 2002;30:A214. [Cited in This Article: ] |
| 43. | Hutchinson K, Apel A. Infectious keratitis in orthokeratology. Clin Experiment Ophthalmol. 2002;30:49-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Keddie S. Bilateral Acanthameoba keratitis in juvenile night-wear orthokeratology treatment. Global Orthokeratology Symposium. 2002;Course 6C:1-3. [Cited in This Article: ] |
| 45. | Lin C, Su X, Xu T. Nocardia keratitis as a complication of orthokeratology. Chin Med J. 2005;115:1014-1015. [Cited in This Article: ] |
| 46. | Lau LI, Wu CC, Lee SM, Hsu WM. Pseudomonas corneal ulcer related to overnight orthokeratology. Cornea. 2003;22:262-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 47. | Poole TR, Frangouli O, Ionides AC. Microbial keratitis following orthokeratology. Eye (Lond). 2003;17:440-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 48. | Wang JC, Lim L. Unusual morphology in orthokeratology contact lens-related cornea ulcer. Eye Contact Lens. 2003;29:190-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Xuguang S, Lin C, Yan Z, Zhiqun W, Ran L, Shiyun L, Xiuying J. Acanthamoeba keratitis as a complication of orthokeratology. Am J Ophthalmol. 2003;136:1159-1161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Hsiao CH, Yeh LK, Chao AN, Chen YF, Lin KK. Pseudomonas aeruginosa corneal ulcer related to overnight orthokeratology. Chang Gung Med J. 2004;27:182-187. [PubMed] [Cited in This Article: ] |
| 51. | Lang J, Rah M. Case report: central corneal ulcer with overnight orthokeratology. USA: American Academy of Optometry annual meeting 2003; . [Cited in This Article: ] |
| 52. | Van Der Worp E, Nolf P. Case report. Pseudomonas infection. Global Orthokeratology Symposium. 2004;Session 08B:1-102004. [Cited in This Article: ] |
| 53. | Araki-Sasaki K, Nishi I, Yonemura N, Takatsuka H, Mutoh K, Matsumoto K, Asari S, Tanihara H. Characteristics of Pseudomonas corneal infection related to orthokeratology. Cornea. 2005;24:861-863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 54. | Macsai MS. Corneal ulcers in two children wearing paragon corneal refractive therapy lenses. Eye Contact Lens. 2005;31:9-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 55. | Hsiao CH, Lin HC, Chen YF, Ma DH, Yeh LK, Tan HY, Huang SC, Lin KK. Infectious keratitis related to overnight orthokeratology. Cornea. 2005;24:783-788. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 56. | Tseng CH, Fong CF, Chen WL, Hou YC, Wang IJ, Hu FR. Overnight orthokeratology-associated microbial keratitis. Cornea. 2005;24:778-782. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 57. | Wilhelmus KR. Acanthamoeba keratitis during orthokeratology. Cornea. 2005;24:864-866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 58. | Yepes N, Lee SB, Hill V, Ashenhurst M, Saunders PP, Slomovic AR. Infectious keratitis after overnight orthokeratology in Canada. Cornea. 2005;24:857-860. [PubMed] [Cited in This Article: ] |
| 59. | Lee SJ, Jeong HJ, Lee JE, Lee JS, Xuan YH, Kong HH, Chung DI, Ock MS, Yu HS. Molecular characterization of Acanthamoeba isolated from amebic keratitis related to orthokeratology lens overnight wear. Korean J Parasitol. 2006;44:313-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 60. | Priel A, Grinbaum A, Barequet IS. Severe Pseudomonas aeruginosa keratitis shortly after initiation of corneal refractive therapy. Eye Contact Lens. 2006;32:1-2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 61. | Sun X, Zhao H, Deng S, Zhang Y, Wang Z, Li R, Luo S, Jin X. Infectious keratitis related to orthokeratology. Ophthalmic Physiol Opt. 2006;26:133-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Voyatzis G. Pseudomonas keratitis in a 9 year old patient using orthokeratology. Contact Lens Anterior Eye. 2006;183. [Cited in This Article: ] |
| 63. | Ying-Cheng L, Chao-Kung L, Ko-Hua C, Wen-Ming H. Daytime orthokeratology associated with infectious keratitis by multiple gram-negative bacilli: Burkholderia cepacia, Pseudomonas putida, and Pseudomonas aeruginosa. Eye Contact Lens. 2006;32:19-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 64. | Lee JE, Hahn TW, Oum BS, Choi HY, Yu HS, Lee JS. Acanthamoeba keratitis related to orthokeratology. Int Ophthalmol. 2007;27:45-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Robertson DM, McCulley JP, Cavanagh HD. Severe acanthamoeba keratitis after overnight orthokeratology. Eye Contact Lens. 2007;33:121-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 66. | Watt KG, Boneham GC, Swarbrick HA. Microbial keratitis in orthokeratology: the Australian experience. Clin Exp Optom. 2007;90:182-187; quiz 182-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 67. | Golder S, McIntosh HM, Duffy S, Glanville J. Developing efficient search strategies to identify reports of adverse effects in MEDLINE and EMBASE. Health Info Libr J. 2006;23:3-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 68. | Schein OD. Microbial keratitis associated with overnight orthokeratology: what we need to know. Cornea. 2005;24:767-769. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 69. | Young AL, Leung KS, Tsim N, Hui M, Jhanji V. Risk factors, microbiological profile, and treatment outcomes of pediatric microbial keratitis in a tertiary care hospital in Hong Kong. Am J Ophthalmol. 2013;156:1040-1044.e2. [PubMed] [Cited in This Article: ] |
| 70. | Efron N, Morgan PB, Woods CA. Survey of contact lens prescribing to infants, children, and teenagers. Optom Vis Sci. 2011;88:461-468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 71. | US Food and Drug Administration Center for Devices and Radiological Health. Euclid Systems Corporation, Summary of safety and effectiveness data from premarket approval application number P010062. Cited: 2014-03-03. Available from: http: //www.accessdata.fda.gov/cdrh_docs/pdf/P010062b.pdf. [Cited in This Article: ] |
| 72. | Lipson MJ. Long-term clinical outcomes for overnight corneal reshaping in children and adults. Eye Contact Lens. 2008;34:94-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 73. | Van Meter WS, Musch DC, Jacobs DS, Kaufman SC, Reinhart WJ, Udell IJ. Safety of overnight orthokeratology for myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115:2301-2313.e1. [PubMed] [Cited in This Article: ] |