Published online Nov 27, 2016. doi: 10.5313/wja.v5.i3.62
Peer-review started: July 29, 2016
First decision: September 6, 2016
Revised: October 3, 2016
Accepted: October 22, 2016
Article in press: October 24, 2016
Published online: November 27, 2016
Intraoperative awareness is the explicit recall of sensory perceptions during general anesthesia. I presume the epidemiology and characteristics of intraoperative awareness from these surveys in Japan. A questionnaire survey was conducted via the Internet. The first survey was conducted in 2008. Our survey showed 17% of anesthesiologists experienced definite or possible awareness. The second survey was conducted to evaluate the first survey in detail in 2008. A total of 172 anesthesiologists answered. The total number of reported anesthetic cases was 85156. Twenty-four cases of definite or possible awareness were reported by 21 anesthesiologists. The most surprising finding was total intravenous anesthesia (TIVA) was used in 21 of the 24 cases. The third survey was conducted in 2011 as a continuous survey. Six cases of definite or possible awareness were reported by six anesthesiologists (7%). Two cases were maintained by TIVA, and 2 cases were sevoflurane. The survey showed 76% anesthesiologists routinely use bispectral index (BIS) for TIVA, but for sevoflurane only 27% anesthesiologists routinely use BIS. The incidence of intraoperative awareness decreased in the third survey. The continuous survey revealed the current status of daily anesthesia and the results might be used to prevent the awareness during general anesthesia.
Core tip: The epidemiology and characteristics of intraoperative awareness from these surveys in Japan are reviewed in this manuscript. The incidence of intraoperative awareness decreased in the third survey. The continuous survey revealed the current status of daily anesthesia and the results might be used to prevent the awareness during general anesthesia.
- Citation: Morimoto Y. Awareness during anesthesia: Current status in Japan. World J Anesthesiol 2016; 5(3): 62-66
- URL: https://www.wjgnet.com/2218-6182/full/v5/i3/62.htm
- DOI: https://dx.doi.org/10.5313/wja.v5.i3.62
Intraoperative awareness is a rare but still serious problem in clinical anesthesia. It is defined as ann explicit recall of sensory and auditory awareness during general anesthesia. The incidence of intraoperative awareness has been reported as 0.1%-0.2%[1,2]. Although this problem is rare, some patients might suffer prolonged psychological side effects, including post-traumatic stress disorders.
Widespread changes have occurred after the introduction of remifentanil in Japan in 2007. This caused a reduction of the maintenance dose or concentrations in volatile anesthesia. These changes might induce the increase in the incidence of intraoperative awareness. Therefore, we conducted three separate questionnaire surveys of anesthesiologists from 2008 through 2011. From the results of these surveys, we were able to make presumptions about the epidemiology and characteristics of intraoperative awareness, and discuss recommendations to decrease its incidence.
Remifentanil was released in Japan in 2007, followed by widespread changes in anesthesiology procedures. The doses of anesthetics used in combination with remifentanil might decrease. Moreover, the choice of total intravenous anesthesia (TIVA) increased. These changes might have increased the incidence of awareness.
The incidence of awareness during general anesthesia has not been evaluated prospectively in Japan. Therefore, we conducted a questionnaire survey in 2008[3]. The purpose of the survey was to assess the status of anesthesia after the release of remifentanil and the incidence of intraoperative awareness during remifentanil anesthesia.
Letters were sent to the chief staff anesthesiologists in Japanese hospitals to response the survey. The responders answered the survey questions anonymously on an open access website. It was designed to acquire the information concerning daily clinical anesthesia, choice of anesthetics, and experiences of intraoperative awareness during 2007.
A total of 145 anesthesiologists responded to the survey. Five (3%) anesthesiologists reported cases of definite awareness, and 21 (14%) anesthesiologists reported cases of possible awareness.
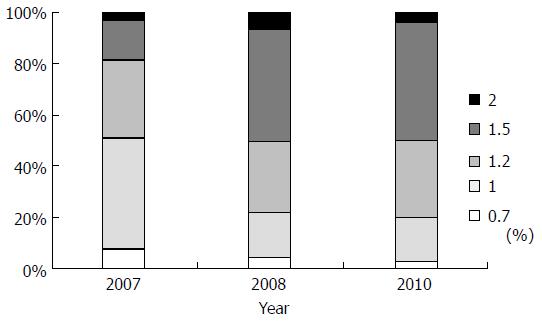
The relationship between daily anesthesia practice and experience with intraoperative awareness was evaluated. Concerning the standard maintenance concentration of sevoflurane in combination with remifentanil, 7% of the anesthesiologists used 0.7%, 44% used 1%, 30% used 1.2%, and 16% used 1.5%. These low concentrations might be explained by the manufacturer’s usage guide for remifentanil stating that sevoflurane should be used at a 1.0% concentration in combination with remifentanil. The choice of sevoflurane concentrations might also have been influenced by a report by Manyam et al[4] that recommended 0.75% sevoflurane in combination with remifentanil. Figure 1 shows the relationship between cases of awareness reported by the anesthesiologists and their standard maintenance sevoflurane concentration. The anesthesiologists who experienced definite awareness cases maintained sevoflurane concentrations below 1.0%. Cases of intraoperative awareness were significantly lower for anesthesiologists who maintained sevoflurane concentrations above 1.2% than for those who maintained concentrations below 1.0%. This result is compatible with a study by Avidan et al[5] that found the incidence of awareness in patients maintained with end-tidal volatile anaesthetic concentrations above 0.7 minimum alveolar concentration (1.2%-1.4% sevoflurane) was 0.1%, which is compatible with the incidence in patients maintained at target bispectral index (BIS) values between 40 and 60. Our results show that, after the release of remifentanil, the incidence of intraoperative awareness might have been higher because 17% of anesthesiologists experienced definite or possible awareness cases in one year. Maintaining sevoflurane concentrations below 1.0% might be associated with a high risk for intraoperative awareness. Our results indicate that maintaining volatile anesthetic concentrations is the most important factor in preventing intraoperative awareness.
To get more detailed information, the second survey was planned[6]. The second survey was planned to obtain information concerning the cases involving intraoperative awareness in 2008. The survey method was similar to that of the first survey. A total of 172 anesthesiologists responded to the second survey. The total number of general anesthesia cases in 2008 was 85156 in this survey. Twenty-one anesthesiologists reported 24 cases of definite or possible awareness, of which 14 were cases of definite awareness and 10 were possible awareness. One patient experienced definite awareness twice, and another patient suffered possible awareness three times. The incidence of intraoperative awareness, including cases of possible awareness, was 0.028%. Many previous studies demonstrate a higher incidence of about 0.2%[1,2]. However, the results of a retrospective study revealed that the actual incidence of awareness is underestimated. For example, a recent report[7] from the Fifth National Audit Project (NAP5), the national United Kingdom survey of intraoperative awareness during general anesthesia based on voluntary reporting by doctors, estimated that the incidence of awareness in general anesthesia was as low as 1:15414. Our survey results are consistent with the results of a retrospective study reported by Mashour et al[8]. The results of our study indicate that the incidence of awareness during anesthesia in Japan is compatible with the incidence reported in other countries.
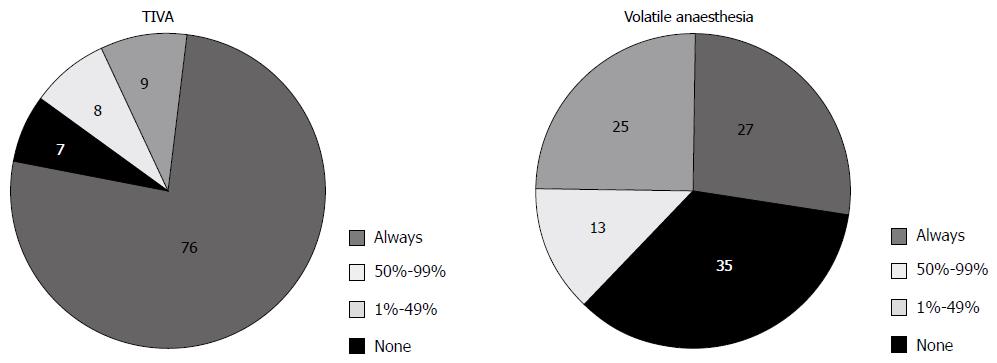
The most surprising finding from the second survey was that propofol was used as the anesthetic in TIVA in 21 of the 24 cases. Therefore, our results provide information about the characteristics of awareness in TIVA. Based on the data about daily anesthesia acquired from the survey, 16% of anesthesiologists reported using mostly propofol, 17% used more propofol than volatile anesthetics, 9% used propofol and volatile anesthetics equally, 26% used more volatile anesthetics than propofol, and 32% used mainly volatile anesthetics. This result indicates that volatile anesthetics were chosen more commonly than propofol. Our survey indicates that TIVA might be a risk for intraoperative awareness.
TIVA’s role as a risk for intraoperative awareness is still controversial. No prospective studies evaluated the incidence of awareness between the anesthetics. However, some studies have stated to TIVA as a risk factor for awareness[9]. One reported risk is associated with the failures of infusion pumps. The absence of real-time feedback of blood anesthetic concentrations might also be a risk factor. Moreover, the inter-individual variability in need of anesthetics essential to prevent movement during the noxious stimulation may be not as much of volatile anesthetics than TIVA[10]. The target-controlled infusion system predicts the plasma anesthetics concentrations, which might be different from the actual concentration. Therefore, the use of brain monitoring, including BIS, is essential. In our survey, BIS monitoring was used in seven (33%) out of 21 awareness cases that were maintained by TIVA. This shows that the use of a BIS monitor could not prevent all cases of awareness. The usefulness of BIS to prevent awareness in TIVA should be evaluated in a future study.
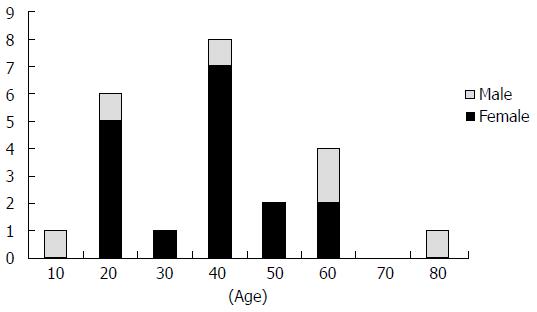
In our survey, 16 (67%) of the patients experiencing awareness during general anesthesia were below 50 years of age, and the majority of patients were female (Figure 1). Similarly, previous studies showed that the incidence of awareness is higher in female patients[11]. Moreover, women recovered from propofol anesthesia more rapidly than men[12]. This might indicate that women are less sensitive to propofol.
The reported surgical procedures included one craniotomy, four facial operations, seven neck and chest wall operations, one cardiac operation, three gynecologic operations, three operations for fractures of the leg, and one spinal operation. The results indicate that the surgical procedures with the highest risk for awareness are cervicofacial and chest wall surgery. In brief, surgery in the upper part of body produced the highest risk of awareness. Gynecologic and orthopedic procedures were the next most likely to be associated with intraoperative awareness.
The high incidence of awareness in cervicofacial surgery[2] has not reported previously. Although the reasons are unclear, it is thought that visual and auditory stimulation during surgery play a part[12]. The higher risk during orthopedic surgery supports this hypothesis because elevated levels of acoustic stimulation are common during orthopedic operations. There might also be an increased risk of awareness when general anesthesia is maintained by TIVA.
The third survey was conducted in 2011 as a continuous survey[13]. We particularly sought to evaluate whether TIVA is a risk factor for intraoperative awareness. The survey was designed to obtain information regarding cases involving intraoperative awareness in 2010. Responses were received from 119 anesthesiologists. Because of incomplete data, only 91 responses were analyzed. Respondents reported 29340 general anesthesia cases in 2010; volatile anesthetics were used in 18109 cases, and propofol was used in 10184 cases.
Anesthesiologists reported six cases of definite or possible awareness. By the third survey, the incidence of awareness, including possible awareness, was 0.02%. This result is similar to the result of the second survey. Sevoflurane and propofol were used for maintenance of general anesthesia in four cases, two cases for each anesthetic (Table 1). The remaining two cases involved caesarean deliveries. Therefore, the incidence of intraoperative awareness in procedures with volatile agents and TIVA was 0.011%, and 0.019%, respectively. The difference in the incidence of awareness between volatile anesthesia and TIVA was not statistically significant (P = 0.622).
| Case | Age | Sex | Anesthetics | BIS monitoring | Detail |
| 1 | 30 | M | Sevoflurane | - | Low sevoflurane concentration before surgery |
| 2 | 50 | M | Sevoflurane | + | Low sevoflurane concentration during bleeding |
| 3 | 70 | F | TIVA | - | |
| 4 | 80 | F | TIVA | - | Trouble in infusion pump |
The survey results show that 74% of anesthesiologists routinely used BIS for TIVA, but only 28% of anesthesiologists routinely used BIS for volatile anesthesia (Figure 2). Use of BIS monitoring was more frequent during TIVA than volatile anesthesia (P < 0.01). These results suggest that anesthesiologists feel that there is a need for BIS monitoring when they use TIVA for maintenance of general anesthesia, perhaps because propofol has a wide variability in dosing.
The results of our second survey, which showed that TIVA was a risk factor for awareness, might have affected the frequency with which anesthesiologists used BIS monitoring. This concept is supported by the results of a review by Avidan et al[5]. The authors recommended using an end-tidal anesthetic concentration alarm rather than BIS when a volatile agent is used as the primary anesthetics. On the other hand, they suggested using BIS when volatile anesthetics are not used, because BIS monitoring prevents awareness in TIVA.
In one of two reported awareness cases, the patient might have awakened when sevoflurane was maintained at a low concentration before surgery; in the second case, the patient might have awakened when the sevoflurane concentration dropped because of hypotension caused by massive blood loss. These awareness cases could have been prevented if the sevoflurane concentration had been maintained above a certain level. There should be a further decrease in the incidence of awareness shortly.
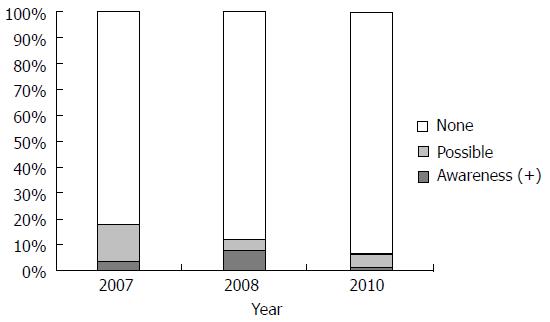
We conducted three surveys at separate times. The results were quickly disseminated to Japanese anesthesiologists after each survey. Figure 3 shows the standard maintenance sevoflurane concentration for daily clinical anesthesia reported in each of the three surveys. In the first survey, only 20% of the anesthesiologists used a sevoflurane concentration above 1.5%. However, in the second and third surveys, about 50% of the anesthesiologists used sevoflurane concentrations above 1.5%. This increased use of higher sevoflurane concentrations might be the reason for the lower incidence of awareness under sevoflurane reported in the second and third surveys. In the first survey, 18% of the anesthesiologists experienced cases of intraoperative awareness, including possible cases. However, this decreased to 7% in the third survey (Figure 4). Moreover, the tendency of TIVA to be a risk factor for intraoperative awareness was not observed. The continuous survey revealed the current status of anesthesia in Japan, and the results might be used to prevent awareness during general anesthesia.
In conclusion, awareness with explicit recall during general anesthesia remains a problem that should be prevented. Understanding the incidence of awareness and the status of daily anesthesia are one possible approach to a cure for this problem.
Manuscript source: Invited manuscript
Specialty type: Anesthesiology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Abdallah C, Markic D, Yang JJ S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Ghoneim MM. Awareness during anesthesia. Anesthesiology. 2000;92:597-602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 90] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Sebel PS, Bowdle TA, Ghoneim MM, Rampil IJ, Padilla RE, Gan TJ, Domino KB. The incidence of awareness during anesthesia: a multicenter United States study. Anesth Analg. 2004;99:833-839, table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 439] [Cited by in F6Publishing: 365] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 3. | Morimoto Y, Nogami Y. Intraoperative awareness during sevoflurane-remifentanil anesthesia. Rinshomasui (J Clin Anesth). 2009;33:1283-1285. [Cited in This Article: ] |
| 4. | Manyam SC, Gupta DK, Johnson KB, White JL, Pace NL, Westenskow DR, Egan TD. Opioid-volatile anesthetic synergy: a response surface model with remifentanil and sevoflurane as prototypes. Anesthesiology. 2006;105:267-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Avidan MS, Mashour GA. Prevention of intraoperative awareness with explicit recall: making sense of the evidence. Anesthesiology. 2013;118:449-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Morimoto Y, Nogami Y, Harada K, Tsubokawa T, Masui K. Awareness during anesthesia: the results of a questionnaire survey in Japan. J Anesth. 2011;25:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Pandit JJ, Cook TM, Jonker WR, O’Sullivan E. A national survey of anaesthetists (NAP5 Baseline) to estimate an annual incidence of accidental awareness during general anaesthesia in the UK. Anaesthesia. 2013;68:343-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Mashour GA, Wang LY, Turner CR, Vandervest JC, Shanks A, Tremper KK. A retrospective study of intraoperative awareness with methodological implications. Anesth Analg. 2009;108:521-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Errando CL, Sigl JC, Robles M, Calabuig E, García J, Arocas F, Higueras R, Del Rosario E, López D, Peiró CM. Awareness with recall during general anaesthesia: a prospective observational evaluation of 4001 patients. Br J Anaesth. 2008;101:178-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Vuyk J, Lim T, Engbers FH, Burm AG, Vletter AA, Bovill JG. Pharmacodynamics of alfentanil as a supplement to propofol or nitrous oxide for lower abdominal surgery in female patients. Anesthesiology. 1993;78:1036-1045; discussion 23A. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Domino KB, Posner KL, Caplan RA, Cheney FW. Awareness during anesthesia: a closed claims analysis. Anesthesiology. 1999;90:1053-1061. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 222] [Cited by in F6Publishing: 174] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 12. | Gan TJ, Glass PS, Sigl J, Sebel P, Payne F, Rosow C, Embree P. Women emerge from general anesthesia with propofol/alfentanil/nitrous oxide faster than men. Anesthesiology. 1999;90:1283-1287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 107] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Thiele RH, Knipper E, Dunn LK, Nemergut EC. Auditory stimuli as a contributor to consciousness while under general anesthesia. Med Hypotheses. 2013;80:568-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |